FINAL Azathioprine-6Mercaptopurine IBD ESCA
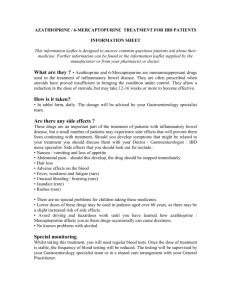
advertisement
WORKING IN PARTNERSHIP WITH EFFECTIVE SHARED CARE AGREEMENT (ESCA) DRUG NAMES: AZATHIOPRINE and MERCAPTOPURINE INDICATION/S COVERED: INFLAMMATORY BOWEL DISEASE Coastal West Sussex Traffic Light system classification: Amber N.B. The eligibility criteria included here apply to new patients commencing treatment under this agreement & not to existing patients whose treatment was initiated under the previous version. However, monitoring and discontinuation criteria apply to all patients. NOTES to the primary care prescriber Amber drugs: Prescribing to be initiated by a consultant / specialist but with the potential to transfer to primary care. The expectation is that this agreement should provide sufficient information to enable primary care prescribers to be confident to take clinical and legal responsibility for prescribing these drugs . The questions below will help you confirm this: Is the patient’s condition predictable? Do you have the relevant knowledge, skills and access to equipment to allow you to monitor treatment as indicated in this effective shared care agreement? Have you been provided with relevant clinical details including monitoring data? If you can answer YES to all these questions (after reading this ESCA), then it is appropriate for you to accept prescribing responsibility. Sign and return a copy of the final page to the requesting consultant / specialist. Until the requesting consultant / specialist has received a signed copy of the final page indicating that shared care has been agreed all care (including prescribing) remains with the consultant / specialist. If the answer is NO to any of these questions, you should not accept prescribing responsibility. You should write to the consultant / specialist within 14 days, outlining your reasons for NOT prescribing. If you do not have the confidence to prescribe, we suggest you discuss this with your local Trust/specialist service, which will be willing to provide training and support. If you still lack the confidence to accept clinical responsibility, you still have the right to decline. Your Medicines Management pharmacist will assist you in making decisions about shared care. Prescribing unlicensed medicines or medicines outside the recommendations of their marketing authorisation alters (and probably increases) the prescriber’s professional responsibility and potential liability. The prescriber should be able to justify and feel competent in using such medicines. The patient’s best interests are always paramount The primary care prescriber has the right to refuse to agree to shared care, in such an event the total clinical responsibility will remain with the consultant Effective from: January 2014 Review date: January 2016 Page 1 of 7 AZATHIOPRINE and MERCAPTOPURINE, version 1 Information This information sheet does not replace the Summary of Product Characteristics (SPC), which should be read in conjunction with this guidance. Prescribers should also refer to the appropriate paragraph in the current edition of the BNF. 1. Link to the relevant SPC websites: http://www.medicines.org.uk/emc/medicine/26876/SPC/Azathioprine+50+mg+film-coated+tablets/ http://www.medicines.org.uk/emc/medicine/2882/SPC/Imuran+Tablets+50mg/ http://www.medicines.org.uk/EMC/medicine/24688/SPC/PURI-NETHOL+50+mg+Tablets/ 2. Background to use for the indication/s, including licence status: The thiopurine drugs azathioprine and its metabolite mercaptopurine, also known as 6mercaptopurine, are used in treatment of resistant or frequently relapsing cases of ulcerative colitis and Crohns’ disease. They are used mainly as steroid-sparing agents and are effective for both active disease and maintaining remission. Although unlicensed for these indications a large body of evidence exists supporting their use and they are included in both national and international IBD treatment guidelines. The thopurines are cytotoxic immunomodulaters that act to supress the immune system, hence their use in inflammatory conditions such as IBD. The exact mechanism of action of these agents, and their numerous metabolites are unknown, but it is likely multifactorial with purine antimetabolite activity, inhibition of nucleic acid biosynthesis (inhibiting proliferation and activity of immuncompetent B- and T- lymphocytes) and damage to DNA through incorporation of thiopurine analouges. Azathioprine is a pro-drug and is non-enzymatically metabolised to mercaptopurine in vivo. The loss of a nitro-imidazole side chain in this process is thought to explain some of the side effects, such as nausea, seen with azathioprine and which may be less of a problem with mercaptopurine. Thiopurines are considered for patients who require two or more corticosteroid courses within a calendar year; those whose disease relapses as the dose of steroid is reduced below 15 mg; relapse within 6 weeks of stopping steroid steroids. 3. Dose & administration Azathioprine Dosage in adults over 18: Severe acute Crohn's disease, maintenance of remission of Crohn's disease or ulcerative colitis in adult over 18 years, by mouth, usually 2–2.5 mg/kg daily; titrated according to response. Mercaptopuriune Dosage in adults over 18: Severe acute Crohn's disease, maintenance of remission of Crohn's disease or ulcerative colitis in adult over 18 years, by mouth, 0.75–1.5 mg/kg daily; titrated according to response. For both azathioprine and mercaptopurine consideration should be given to reducing the dose in renal impairment and hepatic dysfunction. No specific dose reduction is required in the elderly but doses should be started at the lower end of the range. 4. Cautions There are risks from bone marrow suppression and patients should have frequent monitoring. Patients must also be advised to inform their doctor or specialist immediately about ulcerations of the throat, fever, infections, bruising, bleeding or other signs of myelosuppression Undue exposure to UV rays should be avoided due to an increased number of skin tumours seen, and skin should be regularly examined Impaired hepatic and renal function Reduced TPMT activity Effective from: January 2014 Review date: January 2016 Page 2 of 7 AZATHIOPRINE and MERCAPTOPURINE, version 1 Concomitant drugs that inhibit TPMT see interactions. As these are cytotoxic drugs patients should be warned about the risks associated with handling these drugs Lesch-Nyhan syndrome Risk of developing neoplasia, non-melanoma skin cancer and lymphoproliferative disorders. Pregnancy and lactation: Azathioprine and mercaptopurine are potentially teratogenic and are also excreted in the breast milk. All patients contemplating becoming pregnant should be seen by a consultant gastroenterologist to discuss the complex issues around using thiopurine agents in both pregnancy and lactation. In any individual case the potential hazard to the foetus must be balanced against the expected benefit to the mother. Recommendations from international guidelines at present are such that the benefits of continuing established therapy outweigh the small risks to the foetus9. It is important that when decisions are being made in this area a specialist is involved and the prescriber uses the most up to date information. Use in lactation is contra-indicated in the Summary of Product Characteristics for both drugs. The BNF states that azathioprine can be used if the risk outweighs the benefit. Any possible use of these drugs in lactation would therefore be outside of license and should only be considered under specialist advice. As with all cytotoxic chemotherapy, adequate contraceptive precautions should be advised if either partner is receiving azathioprine or mercaptopurine. 5. Contraindications Immunisation using a live organism Severe infection Severely impaired hepatic or bone marrow function Absent TPMT activity Hypersensitivity to any component of the preparations as well as those listed in cautions and interactions. Breast Feeding – see pregnancy and lactation 6. Side effects: Nausea and vomiting is a very common side effect. The most common cause of intolerance (affecting up to 20%) are flu-like symptoms (myalgia, headache, diarrhoea, fever, arthralgia, rash) that characteristically occur after 2–3 weeks and cease rapidly when the drug is withdrawn. The most serious complication is profound bone marrow suppression causing leucopenia. This can develop suddenly and unpredictably in between blood tests, although it is rare (around 3%). Patients should be informed seek advice from their GP or specialist team if they develop possible symptoms of myelosuppression such as sore throat or easy bruising. In such cases and urgent FBC should be performed. Hepatotoxicity and pancreatitis have occurred but are uncommon (<5%). For the most up to date information and a full list of all other side effect please refer to current BNF and SPC 7. Interactions Allopurinol – DO NOT give unless co-initiated under specialist supervision Sulfamethoxazole plus trimethoprim (as co-trimoxazole) and trimethoprim alone – increased risk of haematological toxicity. Please avoid these antibiotics Vaccines – AVOID LIVE VACCINES. Severe or fatal infections may occur if a live vaccine is given. Inactivated vaccines can be given but may produce a lower response. Neuromuscular agents – anaesthetist should be contacted prior to surgery Aminosalicylates – possible increased risk of leucopoenia (e.g. olsalazine, mesalazine, sulfasalazine) Coumarins Clozapine Febuxostat Ribavirin. For up to date information on interactions prescribers are advised to consultant the most recent BNF or contact a pharmacist for advice. If any of the above drugs are considered essential the specialist Effective from: January 2014 Review date: January 2016 Page 3 of 7 AZATHIOPRINE and MERCAPTOPURINE, version 1 should be contacted for advice. 8. Criteria for use Should only be initiated by clinicians experienced in the treatment of inflammatory bowel disease (unlicensed indication) and prescribing transferred to primary care once patient’s dose is stabilised. 9. Any further information (e.g. supporting therapies) TPMT (thiopurine methyltransaminase) testing is recommended as best practice prior to initiation of thipourine therapy. This enzyme is involved in the metabolism of these drugs and a genetic polymorphism can lead to accumulation and subsequent bone marrow suppression. WSHfT offers TMPT deficiency testing. 10. References 1. Mowat C, Cole A, Windsor A, et al. Guidelines for the management of inflammatory bowel disease in adults for the BSG. Gut [online] 2011; Available from: http://www.bsg.org.uk/images/stories/docs/clinical/guidelines/ibd/ibd_2011.pdf <Acessed on 29/10/2013> 2. Dignass A, et al. The second European evidence-based consensus on the diagnosis and management of Crohns disease: Current management. Journal of Crohns and Colitis [online] 2010; 4, 28-62. Available from: http://www.ecco-jccjournal.org/article/S1873-9946(09)00145-7/fulltext < Acessed on 29/10/2013> Travis S P L et al. European evidence-based Consensus on the management of ulcerative colitis: Current management. Journal of Crohns and Colitis [online] 2008 2, 24-62 Available from: http://gut.bmj.com/content/55/suppl_1/i16.full < Acessed on 29/10/2013> Crohns and Colitis UK. Drug treatment information–azathioprine and mercaptopurine Available from: http://www.crohnsandcolitis.org.uk/Resources/CrohnsAndColitisUK/Documents/Publications/Drug%20Info/Azathi oprine%20and%20Mercaptopurine.pdf < Acessed on 29/10/2013> Kandiel A, Fraser AG, Korelitz BI, et al. Increased risk of lymphoma among inflammatory bowel disease patients treated with azathioprine and 6-mercaptopurine. Gut 2005; 54:1121. Disanti W, Rajapakse RO, Korelitz BI, et al. Incidence of neoplasms in patients who develop sustained leukopenia during or after treatment with 6-mercaptopurine for inflammatory bowel disease. Clin Gastroenterol Hepatol 2006; 4:1025. Beaugerie L, Brousse N, Bouvier AM, et al. Lymphoproliferative disorders in patients receiving thiopurines for inflammatory bowel disease: a prospective observational cohort study. Lancet 2009; 374:1617. Peyrin-Biroulet L, Khosrotehrani K, Carrat F, et al. Increased risk for nonmelanoma skin cancers in patients who receive thiopurines for inflammatory bowel disease. Gastroenterology 2011; 141:1621. Janneke van de Woude C, et al. European evidence-based consensus on reproduction in inflammatory bowel disease. Journal of Crohns and Colitis [online] 2010 4, 493-510. Available from: http://www.planapregnancy.co.uk/PP2010/static/ibd_euro_guidelines.pdf < Acessed on 29/10/2013> 3. 4. 5. 6. 7. 8. 9. RESPONSIBILITIES and ROLES 1 2 3 4. 5 Consultant / Specialist responsibilities Confirmation of diagnosis and identification of suitable patients Request agreement of shared care with primary care prescriber Initiation of appropriate therapy Discussion of risks and benefits with patients, outline possible side effects and patients should have sufficient information provided as part of hospital management. This is to inform a rational personal choice about treatment options. On consideration of initiation of these drugs, patients should be given literature explaining the rationale for treatment such as that provided by Crohns and Colitis UK. Monitoring requirements and appropriate dose adjustments and relevant action to be taken if adverse effects are experienced. Monitoring undertaken by the specialist should include the following Before Treatment: Exclude pregnancy Consider vaccinations for influenza, pneumococcus. (HPV and Hepatitis B in addition in high risk groups). Liver Function Tests (LFTs) (including AST/ALT) Full Blood Count (FBC) (including differential white blood cell count and platelets) U&E’s (including creatinine) TPMT assay During treatment (first three months): Every week: FBC and LFTs for six weeks, then continue every two weeks until dose stable for 6 weeks, then monthly Effective from: January 2014 Review date: January 2016 Page 4 of 7 AZATHIOPRINE and MERCAPTOPURINE, version 1 During treatment (after three months): Every THREE months FBC and LFTs if stable on maintenance dose for 6 months. After dose change do FBC and LFT two weeks later then monthly. In heterozygous TPMT (intermediate TPMT levels), monitor at a minimum of monthly intervals. U&E/Creatinine 6 monthly Action and advice in response to blood monitoring and side effects: Blood Test Results Lymphocytes <0.5 x 109/L Neutrophils < 2.0 x 109/L Action Discuss with specialist hospital clinician. Discuss with specialist hospital clinician. < 1.5 x 109/L Platelets < 150 x 109/L Liver function tests >2 fold rise in AST, ALT (from upper limit of reference range) Stop and discuss with hospital specialist clinician. Discuss with hospital specialist clinician. Contact hospital specialist clinician. > 4 fold rise in AST, ALT Symptoms Rash (significant new) Stop azathioprine and contact hospital specialist clinician immediately. Action Stop azathioprine and check FBC. Contact IBD nurse or hospital specialist clinician for advice once results are available. Do not restart until results of FBC known. Stop azathioprine, check FBC and contact IBD nurse or hospital specialist. Do not restart until results of FBC known. Severe or persistent infections, fever, chills. Persistent sore throat Abnormal bruising or bleeding Varicella Nausea For sore throat throats, take FBC and contact the hospital specialist. Stop azathioprine and check FBC. Contact IBD nurse or hospital specialist clinician for advice once results are available. Do not restart until results of FBC known. If in contact with the virus, contact hospital specialist clinician or IBD nurse. Advise patient to divide dosage and take with food. If no improvement, reduce dosage or stop based on advice from IBD nurse or hospital specialist clinician. Blood tests will be monitored by the gastroenterology team and results fed back to primary care prescribers, together with advised action to continue as before or to adjust or stop prescribing as necessary. The gastroenterology team will provide patients with blood forms to present to their primary care prescriber /Phlebotomist for all monitoring blood tests. The gastroenterology team will ensure that the consultants name is on the form and that a copy of the result is sent to the patient’s primary care prescriber. 6 7 Issuing initial prescription(s) until the patient is stabilised (minimum of one month) and until ESCA is in place Ensure that all newly treated patients (and/or their carers) receive appropriate education and advice regarding their drug therapy and shared care arrangements. This should include written information where appropriate 8 Providing primary care prescriber with clinic letter stating planned introduction and reviews 9 Provide outpatient reviews, monitor effectiveness/side effects 10 Give a copy of the information sheet to the patient / carer and explain their roles 11 Notify the primary care prescriber of the patient’s failure to attend for clinical review or drug monitoring 1 2 3 4 5 6 7 8 Primary care prescriber responsibilities Initial referral to secondary care. To inform the consultant if unwilling to enter into shared-care arrangements. The primary care prescriber should ensure that monitoring has taken place in the agreed time scales before issuing a prescription and a demonstrable system exists to ensure this occurs. To provide repeat prescriptions once ESCA is agreed and in place and the patient is stabilised (not before initial one month stabilisation period). To record any changes in therapy in the prescribing record on receipt of such communication from secondary care. To monitor patients overall health and well-being and to report any adverse drug reactions or interactions to secondary care. Liaise with gastroenterology if any cause for concern or drug discontinued. To provide a copy of this ESCA to the patient to ensure that they are familiar with all roles and responsibilities Effective from: January 2014 Review date: January 2016 Page 5 of 7 AZATHIOPRINE and MERCAPTOPURINE, version 1 Patient's / Carer’s role 1 Ask the gastroenterology team or primary care prescriber for information, if he or she does not have a clear understanding of the treatment. 2 Share any concerns in relation to treatment with azathioprine or mercaptopurine 3 Tell the gastroenterology team or primary care prescriber of any other medication being taken, including overthe-counter products. 4 Read the patient information leaflet included with the medication and report any side effects or concerns to the gastroenterology team or primary care prescriber. 5 Arrange blood tests as per gastroenterology team request 6 Report to their gastroenterologist any side effects from the medicine. BACK-UP ADVICE AND SUPPORT Specialist / Consultant: Alternative specialist (e.g. departmental contact): Hospital Pharmacy: Out of hours (e.g. medical team on call): Name / position Gastroenterology (Worthing): Dr Andy LI Dr Atul Sinha Dr Kerry Thomspson Dr Zinu Philipose Dr Sam Thomson Ms Julia Medcalf (IBD CNS Worthing) Telephone 01903 205 111 Gastroenterology (SRH) Dr Adam Stone Dr Jocelyn Fraser Ms Carla Hookaway (IBD CNS SRH) 01243 788122 As above 01903 205 111 01243 788 122 Worthing Hospital St Richards Hospital 01903 205 111, ext 5698 01243 788 122, ext 3347 01903 205 111 On call Medical team Email Secretaries: tina.lock@ wsht.nhs.uk jemma.neave@wsht.nhs.uk Lynne.battrick@wsht.nhs.uk pharmacy@wsht.nhs.uk Version History Document Name: Azathioprine and mercaptopurine Document Type: Effective Shared Care Agreement Relevant to: All primary care prescribers working within Coastal West Sussex and all relevant clinicians at Western Sussex Hospitals Foundation NHS Trust. Version No. Date Author of original development or review Details of document development 1 Dr Andy Li Consultant Gastroenterologist Original development Approval for organisational use ESCA authorised for use in Coastal West Sussex by Specialist/consultant: Dr Andy Li, Consultant Gastroenterologist 15th January 2014 Coastal West Sussex Area Prescribing Committee (APC): 15th January 2014 Effective from: January 2014 Review date: January 2016 Page 6 of 7 AZATHIOPRINE and MERCAPTOPURINE, version 1 EFFECTIVE SHARED CARE AGREEMENT (ESCA) DRUG NAME: AZATHIOPRINE and MERCAPTOPURINE INDICATION: INFLAMMATORY BOWEL DISEASE Agreement for transfer of prescribing to PRIMARY CARE PRESCRIBER Patient details: Name: Address: DoB: NHS No: Hospital No: Drug name and dose: The following tests and investigations have been carried out: Details of tests: Date treatment initiated: At the last patient review the drug appeared to be effectively controlling symptoms / providing benefit: Yes/No The patients has now been stabilised on a dose of: I will arrange to review this patient regularly. Date of next clinic appointment: Title of specialist: Name: Department: Agreement to shared care, to be signed by primary care prescriber and consultant/specialist. Hospital address: Consultant/specialist signature: Contact Number: Date: Primary care prescriber: Address: Contact Number: Main Carer: Contact Number: Key worker if appropriate: Contact Number: Effective from: January 2014 Primary care prescriber signature: Date: If shared care is agreed and the primary care prescriber has signed above please return a copy of this page to the requesting consultant or alternatively fax to: Review date: January 2016 Page 7 of 7