Azathioprine Protocol
advertisement

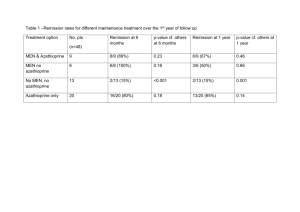
The Birmingham Children’s Hospital NHS Trust Department of Gastroenterology & Nutrition GP/PHYSICIAN GUIDELINES AZATHIOPRINE IN CHILDREN WITH INFLAMMATORY BOWEL DISEASE The team: Professor IW Booth, Dr MS Murphy, Dr. S. Protheroe Sister Ranjit Sandhu-Gastroenterology Liaison Nurse Telephone 0121 333 8718/8720/8705 Fax 0121 333 8701 Please fax or send copies of all blood results to Gastroenterology Dept. at the above address/fax Introduction: Inflammatory Bowel Disease (I.B.D) affects 1 in 10 000 children < 16 years of age. Given the significant adverse effects of long-term steroid therapy, adjunctive or alternative maintenance immunosuppressive therapy are often used and has been shown to be effective in reducing serious adverse effects of steroid therapy and efficacious in reducing complications of the disease. Azathioprine is the safest and best-tried immunosuppressive drug treatment in children. Indication for therapy: Azathioprine was found to be useful in inflammatory bowel diseases: Maintenance of remission As a steroid sparing agent ( in steroid dependant patients) When steroids alone has not provided adequate disease control (steroid resistant cases) In fistulising Crohn’s Disease Prevention of post-operative recurrence of Crohn’s Disease Mechanism of action: AZA is non-enzymatically converted in to 6-Mercaptopurine in the body. About 85% of 6-MP is converted to 6-Thiouracil, by xanthine oxidase. Remaining 15% is competitively metabolised by two enzymes - Thiopurine methyl transferase (TPMT) converts 6-MP into 6-methyl mercaptopurine. Both 6-TU and 6-MMP are inactive metabolites. Hypoxanthine phosphorybosyl transferase (HPRT) converts 6-MP via a series of steps into 6-Thioguanine nucleotides (6-TGN) which is the active metabolite. 6-TGN induces apoptosis of T lymphocytes leading to immunosuppression. Activity of TPMT enzyme is a genetically determined trait. One in 300 individuals have absent or very low levels of this enzyme. These patients are at a very high risk of bone marrow toxicity due to excessive production of 6-TGN nucleotides. About 11% of population have intermediate levels and the rest of the population have normal or high levels. It is advisable to obtain TPMT level before starting AZA so that a safe dose could be prescribed. Please use EDTA bottle (FBC bottle) and take 5 ml of blood. 1 Dose: 2 - 2.5mg /kg/day once daily . This dose can be started straight away in in those with normal TPMT activity. In those children with intermediate activity start a lower dose and increase gradually, closely monitoring blood counts. In those with absent or very low levels it will probably be necessary to avoid Azathioprine - Please discuss with the consultant in charge of the patient. White blood and neutrophil counts are good predictors of achieving and maintaining remission. Lymphocyte count is not valuable for predicting remission or monitoring. Side effects: Non-dose dependent: nausea, vomiting, flu like illness, pancreatitis. Dose dependant: bone marrow suppression (2-5%) severe infections Hepatotoxicity – drug induced hepatitis (0.3%) Patients should be warned to report promptly of infections especially severe sore throat, varicella or herpes infection, unexplained bruising or bleeding. If you are concerned about potential side effects please contact the team. Azathioprine therapy should only be introduced by a hospital specialist trained in paediatric gastroenterology. Before starting Azathioprine, we will provide written information to the family discuss in detail regarding the treatment and arrangements for monitoring . Monitoring: Monitoring for bone marrow toxicity is mandatory throughout the duration of Azathioprine treatment. The following schedule is recommended: Before start Full blood count and differential (including platelets), ESR, Creatinine, CRP, LFT’s, (AST or ALT), albumin, amylase, Varicella Zoster titre and TPMT activity. During the first 8 weeks of therapy Full blood count and differential, Creatinine, LFT’s should be performed weekly. Thereafter, 3 monthly throughout treatment Full blood count and differential, Creatinine, LFT’s, albumin, LFT’s and amylase should be checked at any time if symptoms suggesting an adverse drug effect develop 2 For families’ convenience, bloods may be drawn locally at the G.P’s surgery. Please send copies of all results to Gastroenterology Department at above address/fax. Blood results are entered into our Azathioprine register . Our Liaison Nurse will contact parents if blood monitoring (according to protocol) not received or needs repeating. Adverse reactions: - Stop treatment immediately in the event of development of neutropenia or thrombocytopenia & contact team if any of the following occur: FBC Platelets < 150 x 109/l WCC < 3.0 x 109/l Neutrophils < 1.5 x 109/l Repeat test in 1 week If there is evidence of abnormal LFTs or amylase, the team should be informed who will decide whether to discontinue azathioprine after careful consideration of risk –benefits. Please contact the team if you plan to reduce / stop Azathioprine for any reason. The Gastroenterology team will supervise dose adjustment if required. Treatment is resumed carefully at a lower individualised dose on the advice of the Consultant Specialist after full blood count and /or platelet count has returned to normal. Monitoring should be maintained at weekly intervals until the blood count has become stable. Recovery of Azathioprine –induced myelosuppression is seen within one month after cessation of treatment. Reintroduction of a lower dose is successful (without development of leucopenia or thrombocytopenia) in about 50% of patients. Duration of treatment: Azathioprine has a slow onset of action. Response to treatment is generally seen in about three months after starting therapy but could be delayed. Once started, Azathioprine is continued for atleast 4 to 5 years . If a decision is made to attempt discontinuation, this requires careful consideration of individual patients, previous difficulties, disease control etc and the timing of discontinuation. Refernces : 1. F N Aberra et al: Monitoring of immunomodulators in IBD Aliment Pharmacol Ther 2005; 21 : 307-319 2. A G Fraser et al: The efficacy of azathioprine treatment; a 30 year review. Gut 2002; 50: 85-489 3. M C Dubinsky: Azathioprine, 6-Mercaptopurine in IBD:haarmclogy, efficacy and safety. Clin Gastroenterol Hepatol 2004; 2: 73-734 3 Shared care A consultant may seek the paediatrician and GP’s involvement in sharing care and prescribing for a child with Inflammatory Bowel Disease. This leaflet provides the necessary information for the shared care of patients requiring Azathioprine therapy in the management of I.B.D. and suggested ways in which the responsibilities for managing the prescribing of Azathioprine can be shared between the specialist and general practitioner. Areas of responsibility for the sharing of care. Aspects of care for which the Consultant Specialist is responsible: 1. Select patients requiring Azathioprine therapy with due consideration of the contraindications and precautions. The consultant should inform the general practitioner of the reasons for selection. 2. Decide on the dose, frequency, and duration of therapy and subsequent dosage adjustments. 3. Initiate and prescribe until the dose is stable (normally for the first 8 weeks) 4. Ensure compatibility with other medication 5. Ensure that parents / patients understand the nature and complications of drug therapy and their role in reporting adverse events promptly 6. Ask the GP whether she /she is willing to participate in shared care, and provide the patient with a monitoring and dosage record. 7. Advise the GP when to adjust the dose, stop treatment, or consult with a specialist. 8. Perform baseline tests and recommend frequency of monitoring. 9. Monitor FBC each week for the first 8 weeks and 3 monthly thereafter for the duration of therapy 10. Assess the patient’s condition and communicate promptly with the GP when the treatment is changed. 11. Agree to review patients promptly if required by the general practitioner concerned. 12. Report adverse events to the CSM and GP. 13. Ensure that back up arrangements exist for GP’s to obtain advice and support. Aspects of care for which the General Practitioner is responsible 1. Reply to the request for shared care as soon as possible 2. Prescribe Azathioprine at the dose recommended and adjust the dose as advised by the specialist. 3. Ensure compatibility with other medication. 4. Fax copies of all blood results to Department of Gastroenterology. 5. Stop treatment on the advice of the specialist or immediately if an urgent need to stop treatment arises. 6. Report adverse events to the specialist and CSM. Aspects of care for which the patient/parent is responsible 1. Take the recommended dose and attend for regular blood tests. 2. Report to the specialist or GP if he or she does not have a clear understanding of the treatment 3. Inform specialist or GP of any other medication being taken, including over the counter products 4. Patents/parents should contact their general practitioner if they develop any signs of infection (in order to exclude neutropenia) or bleeding (to exclude thrombocytopenia). 4 Chicken pox contact Chicken pox status is checked by history and serology. ( It is our practice to routinely check varicella titers in all children before they are put on azathioprine) Immunosuppressed patients include: -those being treated with Azathioprine or have received it during the last 3 months, and -children who, within the last 3 months, have received prednisolone, orally or rectally, at a daily dose (or equivalent) of 2mg/kg/day for at least a week, or 1mg/kg/day for 1 month (and are not on Azathioprine). Advice is given on contact with chicken pox. 1. If VZ titers positive (immune) , no further action necessary 2. If VZ titre is negative (non immune) or not known, contact the team, if significant contact with chicken pox eg play or direct contact in same room for > 15 minutes in household, ward or school during the infectious period (from 2 days before onset of rash until crusting of all vesicles) or direct contact with exposed lesions of Herpes Zoster. 3. If less than 72 hours from contact, consider I.M Varicella Zoster Immunoglobulin (VZIG prophylaxis) Dose 250mg (1 vial) for age 0-5yrs 500mg (2 vials) for 6-10 years of age 750mg (3 vials) for 11-14 years of age 1000mg (4 vials) for 15 years and over. TIMING: - VZIG should be give as soon as possible following exposure and not later than 7 days after exposure. ROUTE OF ADMINISTRATION: -VZIG is for intra muscular administration only. Do not treat : Contacts of a contact Patients who have been exposed within 4 weeks of previous VZIG administration Patients in whom the contact occurred more than 7 days previously 4. If child develops chickenpox, stop Azathioprine and contact the team for further advice. VZIG should not be given. 5. Alternative antiviral prophylaxis Acyclovir may be given orally 400mg four times a day for 21 days (up to 2 years of age) or 800mg four time a day (greater than 2 years of age) for 21 days. This is not a licensed indication for Acyclovir. VZIG is prepared from pooled plasma of from non-UK blood donors who are HIV, hepatitis B and C negative. Because of the limited availability of suitable donors, use of VZIG is restricted to those at greatest risk from chicken pox and for whom it is most likely to be effective. (From BCH Guidelines on the prescribing of VZIG, Departments of Pharmacy & Microbiology 1999). 5 Vaccinations Live vaccines should not be given while taking Azathioprine and should be postponed to at least 6 months after stopping Azathioprine. Live vaccines eg Rubella vaccine MMR vaccine Oral polio vaccine BCG vaccine Oral typhoid vaccine (this list is not exclusive) Killed vaccines are safe. Influenza vaccination is not a live vaccine and is recommended annually for patients taking Azathioprine. Back up advice and support Contact details Gastroenterology Department Dr Protheroe/ Prof Booth Dr Murphy Liaison Nurse Hospital Interface Pharmacist Revised July 2005 / M Ravikumara S Protheroe S Murphy 6 Tel no. Fax 0121 333 8720 / 0121 333 8701 0121 333 8705 / 0121 333 8701 0121 333 8718 / 0121 333 8701 0121 333 9772/8 /0121 333 9771