Azathioprine for Inflammatory Bowel disease : better the devil you
advertisement

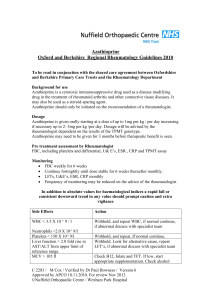
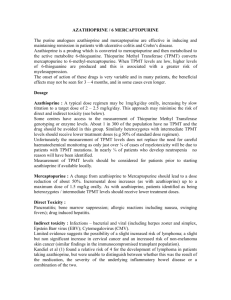
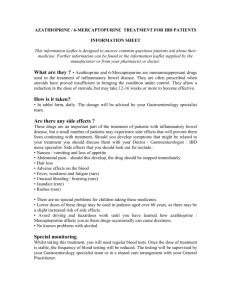
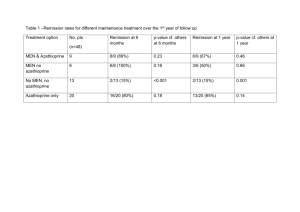
Azathioprine for Inflammatory Bowel disease : better the devil you know Jeremy D. Sanderson Consultant Gastroenterologist Guy’s and St. Thomas’ Hospital Despite our best intentions over recent decades, advances in the medical therapy of Crohn’s disease and ulcerative colitis have yet to make a major difference to the ultimate endpoint of requirement for surgery. This is particularly the case for Crohn’s disease. Biologicals such as anti-tumour necrosis factor alpha are exciting but, in reality, represent another means of achieving a remission which must be sustained by conventional treatments. Of these, azathioprine and 6-mercaptopurine remain the best drugs available for maintaining a steroid-free remission with rates of remission generally being in the region of 55-70% (see slides). Importantly, much more is now known about the pharmacokinetics of azathioprine such that we should be able to use the drug more effectively and push response rates higher. 1 in 10 of the population is heterozygous for a polymorphism halving the activity of thiopurine methyl transferase (TPMT) and resulting in excessive production of cytotoxic thioguanine nucleotides (TGN) and hence a significant risk of myelosuppression. 1 in 300 are homozygous and at severe risk of marrow suppression and even death on treatment with azathioprine. This is wholly avoidable by prior knowledge of TPMT activity. Furthermore, treatment with low dose azathioprine in heterozygotes appears safe and highly effective. Very low doses of azathioprine (5mg alternate days) may be an option in homozygous deficient cases. An additional aspect of TPMT is that higher levels of the enzyme may predict a poor response to the drug. This remains uncertain but would be predicted by the pharmacokinetics such that very high TPMT should result in lower TGN levels. In theory, therefore, patients with very high TPMT might require “supranormal” doses of azathioprine to achieve a clinical response and this needs testing in a prospective clinical trial. Such a dose escalation may, however, add further problems due to the high methylation of azathioprine metabolites leading to possible increased hepatotoxicity. Recent interest has focused on whether the measurement of TGN levels might provide a therapeutic window to facilitate effective use of azathioprine (as well as compliance). Levels of above 230 or 250(pmol/8x108rbc) correlate broadly with clinical remission but, again, a prospective study is required. Apart from perhaps Methotrexate, thiopurines are the only drugs we have to sustain effectively a steroid free remission in Crohn’s disease. We have an increasing variety of ways to induce remission, including biological therapy, but we rely heavily on thiopurines for subsequent therapy. It is of great importance therefore that we make efforts to use these drugs safely and more effectively and greater knowledge of the pharmacokinetics and genomics of thiopurines should enable us to do exactly this.