Lung Cancer Lecture Notes
advertisement
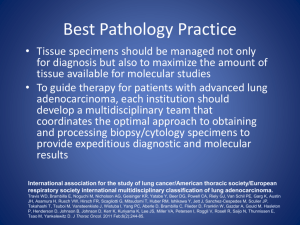
SLIDE 1: Management of Lung Cancer o o o o Introduction: Cindy Card Medical Oncologist at TBCC in Thoracic and Endocrine Oncology Pleasure to be talking to you today o 3 things that I have done to help you understand cancer o Intro to Onc primer o Hand-out to accompany this talk with additional details and resources, including links to guidelines, referrals and pt resources o regardless of which field you go into, you will have patients with cancer so o My hope for today is that you will come out of this lecture with some understanding of how we manage lung cancer, but more importantly why we do this o The patient is the focus, and whatever we can do to help whether that be a treatment for cure or a treatment to palliate, then we need to be able to be there to provide that care Key points that will covered in today’s talk o Lung cancer is not one disease not only in terms of pathology but also in the way it behaves and can be managed o Lung cancer is a disease that is perceived by patients, health care professionals (including many doctors) and even society in a different way than most diseases. There is often a sense that this was self-inflicted and is a diagnosis that carries a lot of shame. o Lastly, I will spend some time reviewing the management of lung cancer o I will do this by presenting 2 cases… or even better stories… of patients that are currently under my care SLIDE 2: Disclosure of Conflict of Interest None SLIDE 3: What does lung cancer look like? – CT image How it looks How to diagnose it That it is “BAD” SLIDE 4: What does lung cancer look like? – Cigarette It is true that smoking is the #1 cause of lung cancer with about 80% of NSCLC seen in current/former smokers, and ~99% of SCLC seen in smokers (highest correlations to smoking of any cancer, FYI) It is normal to feel guilty when first diagnosed with lung cancer if you have smoked. And the comments from people around them probably doesn’t help. I have had many patients who have told me that the first thing anyone asks them when they hear they have lung cancer is “did you smoke?” Studies have shown that people who have smoked and develop lung cancer experience higher levels of guilt, shame, anxiety and depression than those with other forms of cancer, even if they are/were smokers. The danger of lung cancer smoker’s guilt can go even beyond the emotional toll it takes. Due to the stigma, people often hide their diagnosis, fearing that they will be judged as causing their disease. Others don’t seek medical attention as they feel they deserve the problems that they have because they smoked. One study even suggested a higher mortality rate in those who experience this guilt. Why couldn’t it have been breast cancer? Even non-smokers feel shame and guilt at their diagnosis. I had a woman a few weeks ago say to me “Why couldn’t it have been breast cancer” when we met for the first time to discuss her diagnosis of stage IV NSCLC. She felt that people did not believe that she never smoked, including many physicians that she had encountered over the few months leading up to her initial cancer centre consult. The physician who told her of her diagnosis started the conversation by stating that “she should make peace with herself” which made her feel like she must have done something to deserve this. Nobody is perfect. Some of us don’t smoke, but that doesn’t mean we don’t drive too fast at times, eat unhealthy food, stay our in the sun too long, or bask in sedentary behaviors that are risk factors just the same. SLIDE 5: What does lung cancer look like? – People Lung Cancer is not one disease I know that you have had lectures during this course by respirologists and surgeons, where you learned that they are 2 types of lung cancer: Small Cell Lung Cancer and Non Small Cell Lung Cancer. If it were 7-8 years ago, that would really be all we would need to know from pathology in order to make decisions about management Today we have a far greater understanding of lung cancer. We still need to know if it is a SCLC vs NSCLC. But with NSCLC, it is also important for us to know if it is a Squamous cell or a Non-Squamous cell. This is because the chemotherapy drugs that we use, and in what order do we use them depends on this differentiation. Within Non-squamous cell, there are certain subtypes that also may change our management. For example, a patient with a Non-squamous cell which is EGFR mutation positive would likely receive a targeted agent called an EGFR tyrosine kinase inhibitor. These newer chemo drugs are better tolerated than the traditional chemotherapy with higher response rates and longer duration of response. Another example is Large Cell Neuroendocrine Lung Cancer. Although technically this falls under the NSCLC type, its behavior and response to treatment is much more like SCLC, and many oncologists will treat at Lg cell NET like a SCLC It is also important to note that just as there are no two people who are the same in this world, there are no two cancers that are the same. You may have 2 patients with the same diagnosis, same stage, same age and yet the way their cancers are managed will vary based on their personal experiences, on their desires and views and also on their social and spiritual environment. So although I provided a sort of algorithm for the management of lung cancer, this is only a general guide and there is a lot of “Art” in medicine and in oncology that guides specific decisions. Slide 6: Case #1 I’ll call him Tony 57 year old man; executive in Oil and Gas with premium medical plan including bi-annual CT Scan Healthy and active with no concerns <10 pack year history of smoking having quit in late 20’s Goes for his annual medical Slide 7: CT Scan Slide 8: Referred to TOP clinic Slide 9: Algorithm for Lung Cancer Investigations: Bronch/EBUS PFT’s Felt likely to be a Stage 2 NSCLC given CT findings Other tests ordered to complete w/u Slide 10: Adenocarcinoma Slide 11: Bone Scan Solitary area of metastatic disease in ribs Slide 12: Tony Devastated 2nd opinion in US Incurable Tx intent is palliative Referred to TBCC Slide 13: Mgmt of Stage IV NSCLC Symptom focus Adeno o EGFR testing + Obviously, as a medical oncologist, this is the main way that I treat cancer. Chemotherapy is basically any medication used to stop/shrink cancer – whether that be with the intent to cure or to control (aka palliate) Traditional chemotherapy is considered to be cytotoxic – ie cell killing. While a lot of the newer agents are being called ‘targeted therapies’ (even though many still do kill cells) and typically target a specific abnormality in a person’s cancer. In NSCLC, the role of chemotherapy depends very much on the stage: o In resected early stage NSCLC, chemotherapy is used adjuvantly to increase the chance for cure in patients with node positive disease and/or a large primary tumor o In locally advanced NSCLC, chemotherapy is used as a radiosensitizer when radical dose radiation is given with curative intent o In incurable NSCLC, chemotherapy has a palliative role. This is where it is important to know the subtype, EGFR mutation status, and likely other mutations will be assessed in the future when other targeted agents become available Radiation is a focused treatment which plays a variety of roles in the management of lung cancer Regardless of the stage or treatment course, it is imperative to make sure that a patient is having their symptoms cared for in the best possible manner. This may include management of physical symptoms such as pain, nausea, cough, dyspnea. This also includes spiritual and psychological support, as well as financial support. You cannot underestimate the effect of not being able to work and the stress that results from this. So that would include filling out insurance forms and advocating for the patient to the best of your ability. Slide 14: Targeted therapies Afatinib - EGFR + Slide 15: Karen Slide 16/17: CXR Slide 18: CT Slide 19: Karen Slide 20: Pathology Slide 21: Staging Slide 22: Mgmt of SCLC Slide 23: Chemo and radiation Slide 24: post tx scans for Karen Slide 25: Thank you and Questions