Review 6
advertisement
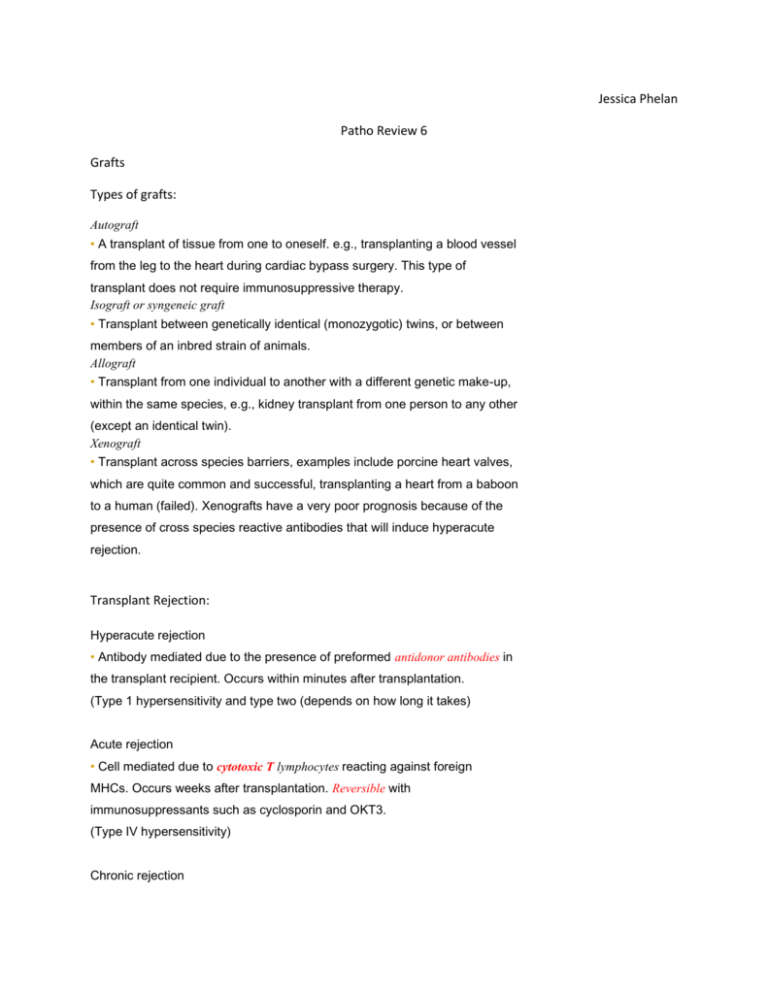
Jessica Phelan Patho Review 6 Grafts Types of grafts: Autograft • A transplant of tissue from one to oneself. e.g., transplanting a blood vessel from the leg to the heart during cardiac bypass surgery. This type of transplant does not require immunosuppressive therapy. Isograft or syngeneic graft • Transplant between genetically identical (monozygotic) twins, or between members of an inbred strain of animals. Allograft • Transplant from one individual to another with a different genetic make-up, within the same species, e.g., kidney transplant from one person to any other (except an identical twin). Xenograft • Transplant across species barriers, examples include porcine heart valves, which are quite common and successful, transplanting a heart from a baboon to a human (failed). Xenografts have a very poor prognosis because of the presence of cross species reactive antibodies that will induce hyperacute rejection. Transplant Rejection: Hyperacute rejection • Antibody mediated due to the presence of preformed antidonor antibodies in the transplant recipient. Occurs within minutes after transplantation. (Type 1 hypersensitivity and type two (depends on how long it takes) Acute rejection • Cell mediated due to cytotoxic T lymphocytes reacting against foreign MHCs. Occurs weeks after transplantation. Reversible with immunosuppressants such as cyclosporin and OKT3. (Type IV hypersensitivity) Chronic rejection • Antibody-mediated vascular damage (fibrinoid necrosis); occurs months to years after transplantation. Irreversible. (type III and type IV) Graft-versus-host disease • Is a common complication of allogeneic bone marrow transplantation • After bone marrow transplantation, T cells present in the graft and attack the tissues of the transplant recipient after perceiving host tissues as antigen • Major symptoms include a maculopapular rash, jaundice, hepatosplenomegaly, and diarrhea. (type IV hypersensitivity) Leukemia: Definition: is a cancer of the blood or bone marrow and is characterized by an abnormal proliferation of blood cells, usually white blood cells (leukocytes) General:↑ number of circulating leukocytes in blood; bone marrow infiltrates of leukemic cells; bone marrow failure can cause anemia (↓ RBCs), infections (↓ WBCs), and hemorrhage (↓ platelets); leukemic cell infiltrates in liver, spleen, and lymph nodes are common. ALL (acute lymphocytic leukemia) • Children(<14 yrs), most common leukemia in children, • Lymphoblasts; • Most responsive to therapy. • May spread to CNS and testes. AML (acute myelogenous leukemia) • Auer rods (peroxidase-positive cytoplasmic inclusions in granulocytes) • Adults (15~39 yrs) • Myeloblasts;. Primarily seen in acute promyelocytic leukemia (M3). • Treatment of AML M3 can release Auer rods → DIC. CML (chronic myelogenous leukemia) • Adults (40~60 yrs) • Most commonly associated with Philadelphia chromosome (t[9;22](translocation), bcr-abl) • Myeloid stem cell proliferation; • presents with ↑ neutrophils and metamyelocytes (kidney-shaped); splenomegaly; may accelerate to AML (“blast crisis”). • Very low leukocyte alkaline phosphatase (vs. leukemoid reaction). CLL (chronic lymphocytic leukemia) • Older adults ( > 60 yrs) • Lymphadenopathy; hepatosplenomegaly; few symptoms; slow course; • ↑ smudge cells in peripheral blood smear • Warm antibody autoimmune hemolytic anemia; • Very similar to ALL (small lymphocytic lymphoma) • Probably "incurable“, but a large group of CLL patients do not require Therapy Manifestations of Leukemias Acute leukemia (three months onset) • anemia; fatigue, pallor • thrombocytopenia; bleeding • neutropenia; infections • bone marrow involvement may cause bone tenderness and pain • CNS symptoms (leukemic cells cross blood-brain barrier) - headache, nausea, vomiting - nerve palsies - sometimes convulsions and coma • weight loss Leukostasis: Abnormal intravascular leukocyte aggregation and clumping often seen in leukemia patients • Describes extreme elevation (>200,000/μl) in circulating blast (immature) cells and impaired circulation. • It is dangerous because it can cause heart attacks and strokes by blocking the arteries. • Presents with headache, confusion, dyspnea • Medical emergency Hyperuricemia • elevated uric acid levels that result from increased proliferation and metabolic alterations of leukemic cells → stone formation or gout Diagnosis: • Based on blood and bone marrow studies • Acute vs. chronic - Acute leukemia is characterized by the rapid growth of immature blood cells - Chronic leukemia is distinguished by the excessive build up of relatively mature, but still abnormal, blood cells • Lymphoid vs. myeloid - It is called lymphocytic leukemia when leukemia affects lymphoid cells (lymphocytes and plasma cells). - It is called myelogenous leukemia when myeloid cells (eosinophils, neutrophils, and basophils) are affected. Treatment: • Chemotherapy • Sometimes bone marrow transplantation • CNS irradiation for "hidden cells" Multiple myeloma a. plasma cell cancer of osseous (bone) tissue, commomly in older persons b. characterized by uncontrolled proliferation of a abnormal clone of plasma cells, usually IgG or IgA type; suppress other Ig's. Shows an increase in IgG. Differential diagnosis- Waldenström’s macroglobulinemia → M spike = IgM (→hyperviscosity symptoms); no lytic bone lesions. c. abnormal immunoglobulin chains present in urine as Bence Jones proteins d. impaired blood cell production (RBC and WBC) and because of bone involvement, bone pain. plasma cells erode bone; "osteoporosis-like" e. treatment consists of chemotherapy and is largely palliative. CRAB – Calcium (elevated), Renal failure, Anemia, Bone lesions Introductory Concepts 1. The level of body water will affect the concentration of electrolytes, i.e. a decrease in body water (ml) will be accompanied by an increased concentration in body sodium (mg/ml). 2. Electrolytes are charged particles; cations (H+, K+, Na+, Mg++, Ca++) anions (HCO3,Cl-, HPO4, SO4). 3. In terms of electrical neutrality, cations must equal anions. 4. Electrolytes are normally expressed in milliequivalents or combining units, hence 1 mEq (1/2 mol) Ca++ will combine with 1 mEq (1 mol) C1- mEq/L = mg/100 ml x 10 x valence atomic weight Some agencies are using International System of Units which is expressed as mmol/l 5. Osmosis: Water moves down its concentration gradient across a semipermeable membrane. The movement of water is related to the number (not size) of nondiffusible particles. 6. Solutes move by diffusion from an area of higher concentration to one of lower concentration. 7. Cell membranes have active transport systems which control the movement of Na and K into and out of the cell. These ion exchange pumps utilize energy in the form of ATP. 8. Body water and electrolytes are distributed between three compartments a) Intracellular (IC) compartment b) Extracellular (EC) compartment --interstitial and intravascular, and the so called third space GI tract, subcutaneous spaces during injury, etc. Conditions which cause water or electrolytes to move into or out of the cell will cause immediate changes in the EC compartment. Likewise, trapping of water and electrolytes in the third space will decrease EC and eventually IC concentrations. 9. Serum levels of electrolytes represent intravascular concentrations and are considered to be representative of total body concentration. At times IC concentrations will differ from EC concentrations. Fluid Balance gains (1) oral intake 2,200 ml. (2) water of oxidation 300 ml. total 2,500 ml. b. losses (1) urine 1,200 ml. (2) insensible losses lungs 1150 ml. (3) feces 150 ml. total 2,500 ml.