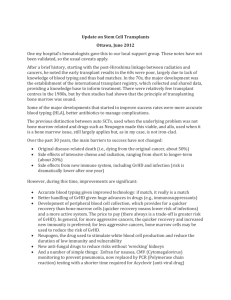
Law, Medicine and Bioethics, Case 6
advertisement
UNESCO Course on Benefit and Harm CASE STUDY: TRANSPLANTATIONS – BONE MARROW DONATION FROM A MINOR AB is a 3-year-old girl with an incurable disease known as Gaucher’s disease. This genetic disease results from an inborn enzyme deficiency. The symptoms in this patient include severe anemia and an enlarged liver and spleen, putting pressure on the lungs and causing breathing difficulties and a tendency to develop pneumonia. AB’s deteriorating medical condition was temporally relieved after a splenectomy performed two months ago. Nevertheless, AB’s condition continues to deteriorate day by day as her liver enlarges. Currently AB’s disabilities are affecting her mobility, causing her difficulty in standing and walking. Her condition is expected to deteriorate rapidly in the next few weeks. The only treatment likely to restore the missing enzyme and cure AB is a bone marrow transplant from a matching donor. If AB does not receive a bone marrow transplant, the disease will lead to her death within a short time. AB’s brother died of this disease at the age of one. CD, AB’s 8-year-old sister, was tested and found to be a tissue match for AB. There does not appear to be any other matching donor for AB. The risks to the donor are minimal. The only risk is from the anesthesia. Removing the bone marrow from CD’s body is a simple procedure, involving extracting an amount of bone marrow equal in volume to a unit of blood. Dr. S, a child psychiatrist, believes that extracting bone marrow from CD might be traumatic. He also believes she will be more traumatized if she must live with the feeling that she did not do everything she could have to save her sister’s life. This trauma will increase as she enters adolescence. Dr. S believes that it is in CD’s best emotional interests to donate bone marrow and recommends proceeding with the transplant. Should a bone marrow transplant from CD to her sister be allowed?