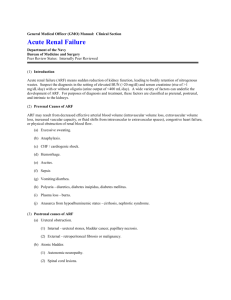
acute renal failure in critical illness and renal replacement therapy
advertisement

ACUTE RENAL FAILURE IN CRITICAL ILLNESS AND RENAL REPLACEMENT THERAPY ARF: Definition and Pathophysiology - Definition.: sudden, sustained decline in glomerular filtration rate, usually associated with azotemia and a fall in urine output (oliguria or anuria) - Problems with definition -- Incr BUN: seen with GI bleeding, severe catabolic states (infection), drugs (corticosteroids) -- Incr creatinine: seen in pts with large muscle mass -- Decr UOP: in pts with decr intake of solute (sodium) or protein, less urine will be requ’d for solute excretion so may have baseline decr UOP - Pathophysiology: 4 Factors -- Decreased glomerular capillary permeability (endoth cell swelling?) -- Back-leak of glomerular filtrate -- Tubular obstruction – debris in the tubules secondary to injured epithelial cells form casts that obstruct, increase intratubular pressure -- Hemodynamic abnormalities – particularly in hypoxic medulla -- obstruction of medullary capillaries -- intrarenal vasoconstriction (too much endothelin and TXA2, too little NO, PGE2 and PGI2); kidney attempts to preserve BP -- Acute Tubular Necrosis – (ATN) Condition characterized by tubular cell necrosis that occurs sec to hemodynamic instability (hypoxia, hypotension, etc.) Clinical Conditions Associated with ARF - Sepsis – Mediator-related renal hypoperfusion -- may be assoc with decreased systemic BP (however, RBF may not be affected by systemic blood vasodilation) -- elevated levels vasopressor, angiotensin II, norepi, etc -- endotoxin directly decreases GFR and increases afferent arteriolar resistance (which is different from other causes of ARF) -- TNF induces WBC release of toxins, local mediators of vascular tone -- Hepatorenal syndrome -- Definintion: clinical condition that occurs in patients with chronic liver disease and advanced hepatic failure characterized by impaired renal function and marked abnormalities in the arterial circulation and activity of the endogenous vasoactive systems. -- In the kidney there is marked renal vasoconstriction that results in low GFR. In the extrarenal circulation there is a predominance of arteriolar vasodilation that results in the reduction of total systemic vascular resistance and arterial hypotension -- occurs secdondary to local and systemic mediators: PG (act as impt renal vasodilators), R-A system, AVP, etc -- Risk factors; classical parameters of liver fx not prognostic -- clinical sx: Type I: rapid (days/weeks) incr in BUN, decr UOP, hyponatremia, hyperkalemia, rarely acidotic, occurs spontaneously but can be seen with SBP; survival in these patients < 2 weeks. Type II:less severe -- Diagnosis: Decreased GFR in the absence of other causes of ARF in patients with liver failure (Crs may be normal or low sec to low protein intake or decr production, and BUN may be high if bleeding) -- can determine GFR by finding resistive index by Doppler -- Management: Avoid low volume states during paracentesis, give prophylactic abx for pts at risk for spontaneous bacterial peritonitis, dialysis may not be helpful. -- Treat liver disease: peritoneovenous shunts, transjugular intrahepatic portasystemic shunt (TIPS), transplant (though CsA may hinder resolution of ARF) -- Heart failure Chronic Heart Failure -- Because of neurohumoral elements (PG, R-A, etc.), pts with low RBF still have preserved GFR and an increased filtration fraction -- this occurs secondary to increased efferent arteriolar resistance and glomerular hydrostatic pressures -- there is also enhanced sodium reabsorption in the Loop of Henle -- all of this ultimately leads to edema and cardiac dilatation -- The kidney’s goal : preservation of CO, BP, and GFR; so hypotension and things that alter the neurohumoral balance (NSAIDS) can precipitate renal failure Acute Heart Failure -- the major determinants of renal well-being are CO, renal perfusion pressure, and the adequacy of intravascular volume resuscitation -- labs typically abnormal 3 days after insult -- Hemolytic Uremic Syndrome -- Definition: Disease of non-immune hemolytic anemia, thrombocytopenia, and renal failure due to platelet thrombi and fibrin deposition in the microcirculation of the kidney -- occurs in kids between 1-10 yo (in the summer, can be in epidemics); usu presents with bloody diarrhea, fever, CNS involvement, etc. -- assoc with E. Coli 0157:H7- (verotoxin may be found in the stool) -- 5-10% mortality in the acute phase (nonrenal) -- Acute Renal Failure -- Decr UOP appears 2-14 days into illness, 60% of pts with HUS have ARF with oliguria -- Management: minimize fluid and Na and K intake, watch nutrition (pts usu catabolic), consider PD when anuric or severely oliguric, antihypertensives -- Abx don’t work; chromosorb in trials (binds to enteric toxins) -- Steroids, anticoagulants don’t work; may do plasma exchange if neurologically affected -- Prognosis: of pts requiring dialysis > 8 days, 60% recovered renal fx: pts requiring dialysis > 28 days, never recover. Associated abnormalities with acute renal failure -- Coagulopathy-- impaired platelet-vessel wall dysfx may be corrected with hemodialysis so uremia-related toxin may be impt -- Nutrition -- ICU pts with higher EE in the absence of ARF than in the presence (may be sec to metabolic demands of a healthier kidney) -- pts will have incr glycemia and insulin resistance -- pts have decr lipolytic activity (incr TG and cholesterol) but are a major source of fuel in pts with ARF -- pts have high protein turnover associated with a hypercatabolic state. -- pts have low vit D levels and low levels of antioxidants like vit E Diagnosis of acute renal failure -- Decrease or increase (change) in UOP, incr BUN/Cr in pts without other reasons -- Source of ARF -- FENa = UNa/SNa prerenal < 1 CANNOT BE ON DIURETICS UCr/SCr postrenal > 1 -- Prerenal failure: urine Na < 20, urine osmolarity > 500 Intrinsic/Postrenal failure: urine Na > 50, urine osmolarity < 300 -- Imaging techniques -- Ultrasound - kidneys usually normal size with prerenal failure and may be increased in size in pts with ATN and acute glomeular nephritis -- Doppler ultrasound – look at Resistive Index (RI) which provides functional information -- Prerenal – Normal RI -- ATN – increased RI -- Hepatorenal syndrome – may have elevated RI -- HUS – elevated RI, hyperechogenic cortex Management of acute renal failure -- Basic Management -- Normal hemodynamics, fluid status (insensibles + UOP), O2 delivery, good nutrition, etc -- maintain nl elytes (watch K+, acid/base, iCa, phosphorous, UA, etc) -- Fluid Management -- Must maintain adequate preload (intravascular volume) -- Diuretics -- Loop Diuretics: more effective and less toxic with continuous infusion vs bolus dosing; works better with combination tx (thiazides); decr tubular cell metabolic demand so is cytoprotective; consider giving albumin if level low. -- Mannitol: antioxidant, osmolar agent -- Inotropes: maintain BP; supplemental Dopamine may work in a pt but as a whole, it does not improve UOP Renal Replacement Therapy -- Indications -- anuric/oliguric failure -- need for more “vascular space” (HA, blood products) -- metabolic abnormalities -- intoxication -- experimental – SIRS, liver failure -- Relative Contraindications -- Active bleeding -- Recent cerebral hemorrhage -- Lack of access -- Hemodynamic instability -- Medical futility -- Physiology -- Diffusion: transmembrane solute movement in response to concentration gradient -- Convection: transmembrane solute movement in association with ultrafiltered plasma water (“solvent drag”); mass transfer rate determined by ultrafiltration rate (pressure gradient) and membrane sieving properties -- Hemodialysis -- Occurs using diffusion -- Hemofiltration -- Occurs using convection -- Allow transfer of small solutes (urea, creatinine, UA, K+, etc); no protein-bound substances are permeable -- Modalities -- SCUF = slow continuous ultrafiltration -- No replacement soln; no dialysate -- CVVH = continuous venovenous hemofiltration -- (+) replacement soln; no dialysate -- replacement fluid is added to prevent sludging post-filtration which can occure with filtration rate > 25% (see figure) -- CVVHD = continuous venovenous hemodialysis -- (+) dialysate; (-) replacement soln -- CVVHDF = cont. venovenous hemodiafiltration -- (+) dialysate and replacement soln -- Solute Clearance – determined by blood flow rate, dialysate/replacement fluid flow rate, and membrane properties -- Fluid Balance -- UFnet = pt removal set on machine – (total fluid in – UOP) -- Total fluid in excludes replacement fluid (which is accounted for in machine settings) -- Anticoagulation -- Adjust heparin to keep ACT (postfilter) 160-200 sec -- If pt coagulopathic, may not need heparin -- Complications -- Hypotension -- Bleeding/clotting -- Hemolysis -- Arrhythmia -- Infection -- Access/technical problems -- Anaphylaxis