Basic Concepts of Mechanical Ventilation
advertisement

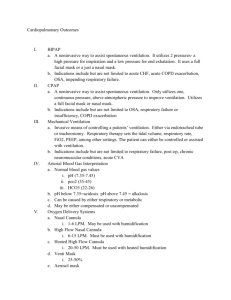
Introduction to Mechanical Ventilation Prepared by EK Buzbee 2/08 Revised 2/12/09 The need for mechanical ventilation Reading assignment: Chang, Mechanical Ventilation Ch. 1 Egan’s Fundamentals, Ch. 41 Basic definitions for mechanical ventilation: The need for mechanical ventilation Spontaneous breathing is the act of using the patient’s primary and accessory muscle of inspiration to create a driving pressure to move gas into the lungs. The intrapulmonary pressure will be less than zero and inspiration will be triggered by changes in the patient’s CSF pH or low Pa02 in the periphery. With normal compliance of 100 ml/cmH20 pressure and normal RAW of .5 to 2.5 cm H20/L/second the WOB is easy because the driving pressure is low. [Egan’s pp. 215] With lowered compliance or increased RAW, the driving pressure needed for adequate alveolar ventilation may rise to the point where the patient needs help. The RAW of the intubated patient rises to about 6 cm H20/L/second [Pilbeam pp. 21] Most [not all] forms of mechanical ventilation will result in the creation of positive pressure in the airway to create the driving pressure needed to move air along. This driving pressure will result in positive pressure inside the thorax for at least part of the breath in contrast to the negative intrathoracic pressures achieved by spontaneous breathing. The need for mechanical ventilation is usually due to a person’s problem with the ability of the patient to create the driving pressure required to move gas into the alveoli so that diffusion can occur. The driving pressure might be excessive due to decreased compliance or increased R AW, or the patient may lack the ventilatory muscles to initiate a normal driving pressure. The patient may lack the ventilatory drive so that changes in pH or Pa02 have little or no effect on the brain stem. In this unit we will discuss these problems with spontaneous ventilation. You may need to review your pathology notes for the specific effects of disease states on spontaneous breathing. Respiratory Failure [Egan’s pp.950-962 & Chang pp. 1-23] 1. Define respiratory failure [Egan’s pp. 950] Inability to oxygenate the tissues and/or to remove C02 Frequently both hypoxemia and hypercapnia are present, but we can have situations in which the patient’s problem is refractory hypoxemia without hypercapnia Specifically, if the Pa02 is less than 60 torr and/or the PaC02 is more than 50 torr in a healthy person breathing room air, we can have respiratory failure. A person with chronic hypercapnia can have both moderate hypoxemia and hypercapnia, but the pH will be WNL-thus this person is not in respiratory failure-- until the hypercapnia rises making the pH is only partially compensated. 2. List and differentiate the 3 different types of respiratory failure [Egan’s pp.950-962] Acute hypoxemic respiratory failure- Type I in which there is refractory hypoxemia secondary to a number of causes: shunts, V/Q mismatch, alveolar hypoventilation, diffusion issues and decreased Pi02 Acute hypercapnia respiratory failure- type II: in which the patient is having problems removing C02. This patient will have acute [uncompensated respiratory] acidosis. This can be due to a number of causes: decreased alveolar ventilation, increased VD ventilation [VD physiological], decreased ventilatory drive, respiratory fatigue & increased WOB. Fatigue and increased WOB can be due to compliance and/or RAW issues Chronic respiratory failure [hypoxemia and hypercapnia] - Type III, This person will have an acute onset on a chronic problem. They will have a baseline ABG that shows chronic moderate hypoxemia with compensated respiratory acidosis, but acute illness will drop the Pa02 and raise the C02 so that the pH is now partially compensated respiratory acidosis This patient could have increased RAW or compliance problems associated with a chronic problems such as COPD, chronic restrictive defects such as pulmonary fibrosis or neuromuscular or neurological disorder 3. Define the V/Q mismatch. [Egan’s pp. 950-951] One of the causes of acute hypoxemic respiratory failure. As we remember from A & P there are different zone of alveolar ventilation [V] and pulmonary perfusion [Q] in the normal lung. When there is low V/Q, we have low ventilation with good perfusion When there is high V/Q, we have good ventilation with poor perfusion A pathological V/Q mismatch can be due to decreased alveolar ventilation or decreased pulmonary capillary perfusion. Pathological V/Q mismatches could be due to airways issues, such as secretions or bronchospasm or they could be due to alveolar consolidation or inflammation resulting in decreased alveolar ventilation 4. Discuss the clinical s/s of a V/Q mismatch: [Egan’s pp. 950-951] Hypoxemia that will respond to increased Fi02 5. Define and discuss shunts and shunt like effects. [Egan’s pp.951-952] One of the causes of acute hypoxemic respiratory failure A shunt is an extreme form of V/Q mismatch in which the patient has [refractory] hypoxemia so that supplementary 02 will not raise the Pa02. A normal shunt is 2-3% and is due to the anatomical shunting of right-sided blood into the left side of the heart due to bronchial circulation and coronary blood return. A physiological shunt of less than 10% is considered normal A Pathological shunt is higher and may not actually be an interface between the right and left side of the heart. If enough alveoli are collapsed or filled with fluid, the capillaries going to these nonfunctional areas will be desaturated [right-sided blood.] i. 10-20% is mild ii. 20-30% is significant shunt iii. Over 30% shunt is critical shunt [Chang pp. 15] In these circumstances, merely giving supplementary 0 2 will not treat the hypoxemia because the alveoli are nonfunctional. A means of opening the alveoli is needed. We will discuss these techniques later. 6. Discuss decreased Pi02 as a cause of acute hypoxemic respiratory failure A rare cause of respiratory failure is the phenomenon of decreased Pi02 from situations such as high altitude barometric pressures, replacement of 02 by other gases [such as during a fire.] Obviously, if 02 is given soon enough, before the patient losses consciousness and the ability to protect his airway, the patient may not require ventilation. 7. Discuss the effect of diffusion problems in acute hypoxemic respiratory failure [Egan’s pp. 952] Based on Fick’s law of diffusion through a membrane, the rate of diffusion is inversely proportional to the thickness of the membrane. As the alveolar-capillary membrane is thickening from edema or scarring diffusion of 02 is affected adversely. As alveolar are destroyed by emphysema, the total surface area for gas exchange is decreased so that hypoxic respiratory failure can result 8. Using 02 indices to identify V/Q mismatches and shunts. [Egan’s pp.953-954] Compare the ratio of Pa02 current and Fi02 current to the Fi02 required to correct the Pa02. Is it possible to correct the Fi02? Use the a/A ratio to determine if there is refractory hypoxemia Is the Fi02 more than 50% with a Pa02 of less than 50 torr; if so there is refractory hypoxemia 9. Differentiate between alveolar hypoventilation and diffusion problems. [Egan’s pp.953-954] Both are causes of acute hypoxemic respiratory failure 10. Using 02 indices to differentiate between type I and type II respiratory failure [see mini-clinic Egan’s pp. 954] Look at ABG: is there hypercapnia? Is there respiratory acidosis? If so, then part [or all] of the patient’s problem can be solved by reversing the hypercapnia Calculate the P[A-a]D02: 1. if the patient is hypoxemic but the P[A-a]D02 is not elevated, the hypoxemia may only be due to the rise in alveolar C02 replacing the alveolar 02. Once we blow off the C02 with increased VE the PA02 thus the Pa02 will rise. 11. Discuss the effects of decreased ventilatory drive on respiratory failure. [Egan’s pp.955] Another cause of hypercapnia respiratory failure is decreased ventilatory drive due to abnormal brain stem action from neurological injury, or by CNS depressants. A person with chronic hypercapnia whose chronic hypoxia has been over-corrected by supplementary 02 is also suffering CNS depression “The clinical manifestations of acute hypercapnia are primarily neurological. Acute elevations of PaCO2 greater than 60 mm Hg cause confusion and headache. PaCO2 more than 70 mm Hg produces……CO2 narcosis manifesting as drowsiness, depressed consciousness, or coma. “ http://www.emedicine.com/PED/topic16.htm 12. Situations that contribute to respiratory failure. [Chang pp.1-23] Conditions that result in increased WOB due to need for excessive driving pressures i. increased RAW ii. decreased lung compliance iii. Persons at risk for muscle fatigue would be persons with long-term increased WOB, or persons who are malnourished iv. Persons with severe muscle fatigue need to rest on mechanical ventilation for 24 – 48 hours 2. V/Q mismatch: i. Can be corrected by increasing Fi02 3. Shunts: because the hypoxemia is unresponsive to Fi02, we may need to mechanically ventilate to increase alveolar ventilation or increase baseline pressure. This may or may not include intubation. i. Acute lung injury or ARDS ii. Shock or other severe decreased C 4. Situation that result in ineffective ventilator muscle action i. Dis-coordination / paralysis from neuromuscular or myopathic disorders VC of less than 20 ml/kg IBW requires some ventilator support. VC of less than 25 ml/kg IBW is associated with decreased ability to cough effectively. inspiratory max pressure measures weakness of inspiratory chest wall muscles and diaphragm. a need for mechanical ventilation is seen with a [PI max] less -30 cmH20 o expiratory max pressure measures weakness of the abdominal muscles. a need for mechanical ventilation is seen with a [PE max] less than + 40 cmH20 o be aware that facial weakness can result in false values for these two figures if the patient cannot seal properly—needless to say, that alone tells us we have problems ii. Chest trauma such as flail chest iii. Electrolyte imbalance such as hyperkalemia that affects muscle action: Go here for a cases study of a patient who suffered prolonged paralysis from hyperkalemia http://www.aana.com/uploadedFiles/Resources/Publications/AANA_Journal__Public/2005/December_2005/p437-441.pdf iv. High doses of steroids particularly with persons in sepsis, who have been sedated & paralyzed & ventilated for a period of time resulting in myopathy v. Persons at risk for muscle fatigue would be persons with long-term increased WOB, or persons who are malnourished. 5. Situations that result in increased VD ventilation i. anatomical VD 1. conducting airways. Comprises about 30% of the VD of the body. 2. is equal to 1 ml / pound of IBW 3. Is always present, but can be reduced by tracheostomy which bypasses upper airways 4. VD/VT ratio will change, as the patient’s VT varies but the VD will stay the same If the patient’s IBW is His VD anatomical is If his VT is his VD/VT ratio is 100/500 = .20 20% of his VT is VD 100 pounds 100 ml 500 88 pounds 600 135 pounds 800 180 pounds 900 ii. alveolar VD 1. when an alveoli gets ventilation but no perfusion, it is considered alveolar VD 2. as CO drops or there are problems with pulmonary blood flow the alveolar VD will rise above baseline iii. physiological VD 1. is the sum of the anatomical VD + the alveolar VD 2. VD /VT in normal circumstances, will be more or less equal to the anatomical VD/VT 3. rises in the physiological VD are usually due to rises in the alveolar V D 4. the normal VD /VT is about .3 or 30%. It is not uncommon for mechanically ventilated persons to have VD /VT of .6 and higher. 5. VT - VD = alveolar ventilation 6. Alveolar ventilation results in gas exchange 7. if physiological VD is excessive, we can increase the VT to get the alveolar ventilation back to an effective level 8. Failure to get the VD /VT below .6 will prevent successful weaning of a patient from mechanical ventilation. His VD anatomical is 50 ml 125 ml 88 ml 120 ml If his VT is 500 600 800 900 his VD/VT ratio is: Is this excessive? 50/500 = .10 13. Clinical signs and symptoms of respiratory failure in the adult patient. [Egan’s pp. 921-923] inadequate alveolar ventilation: decreased peripheral air movement, crackles, significant atelectasis or consolidation on X-ray inadequate lung expansion: poor chest movement; weak cough decreased peripheral air movement, crackles, significant atelectasis or consolidation on X-ray poor muscle strength: inability to cough or protect airway decreased peripheral air movement, crackles, significant atelectasis or consolidation on X-ray increased WOB: tachypnic, retractions, flaring, muscle tremor, altered LOC hypoxemic respiratory failure: s/s of hypoxemia, tachycardia, tachypnea, cyanosis, confusion 14. Parameters associated with a need for mechanical ventilation [Egan’s pp. 950-962] s/s of inadequate alveolar ventilation: hypercapnia above 55 torr & pH below 7.20 s/s of inadequate lung expansion: VT less than 5 ml/kg IBW, VC less than 10 ml/kg IBW requires full ventilator support, and RR over 35 bpm s/s poor muscle strength : MIP less than -20 cmH20, VC less than 10 ml/kg and MVV less than 2x VE s/s of increased WOB: VE more than 10 LPM & VD/VT more than .6 s/s hypoxemic respiratory failure: P(A-a)D02 on 100% more than 350 mmHg & Pa0 2/Fi02 less than 200. 15. Arterial blood gases associated with respiratory failure. [Egan’s pp. 950-952, 953, 955-956] Acute respiratory acidosis with moderate/severe hypoxemia Partially compensated respiratory acidosis with moderate / severe hypoxemia. Chronic patient is no longer compensating effectively. Panic values on ABG: hypercapnia above 55 torr & pH below 7.20 Serial ABG in which the trend is to see PaC02 rise each time 16. The effects of decreased compliance or increased RAW on the driving pressure required to ventilate the patient. [Chang’s pp. 3-10] Bedside measurement of the RAW RAW = P1 - P2 Flow rate in liters/second See page 8 Figure 1-2 and 1-3 of Chang. P1 on the mechanical ventilator is the PIP, while P2 is the P plateau When PIP is --cmH20 Pplateau is --cmH20 flow liter/sec 45 35 1 35 33 .83 35 18 RAW: When the machine delivers a VT, there is a peak pressure [PIP], when there is a breath-hold the pressure drops down to the Pplateau before finally returning to the baseline pressure [which may or may not be zero.] The flow rate is not necessarily the peak flow set by the machine, but the actual inspiratory flow rate read from the graphic Bedside measurement of the lung compliance Static C = corrected VT Pplateau – PEEP PEEP cmH20 Pplateau cmH20 corrected VT Static C 10 28 600 ml ml/cmH20 5 18 750 ml ml/cmH20 15 30 800 ml ml/cmH20 Basic definitions for mechanical ventilation: Mechanical ventilation: a machine that can perform bulk transfer of gas into the lung for a patient who cannot perform this task effectively enough to exchange gases. The ventilator works during inspiration, while exhalation is usually passive. Based on the mode of ventilation, these machines will have various parameters the RCP can set to get the required VE, changes in inspiratory time, baseline pressures and Fi02 to normalize ABG. While some use the term ‘respiratory’, a true respiratory would exchange gas molecules and no ventilator on the market can do anything but move bulk gases in and out of the lung. [Pilbeam pp. 16] Inspiratory phase: Breathing involves inspiration in which gas enters the lung. During the inspiratory phase, the machine’s settings and the status of the patient’s lungs will determine parameters such as inspiratory time [TI] and peak inspiratory airway pressures [PIP] inspiratory holds and flow patterns during the inspiratory phase. P R E S S U R E The TI is a function of the flow rate, the V T and the patient’s RAW TI TE T I M E Expiratory phase: the portion of the breath that is concerned with the passive flow of gas out of the lung. The inspiratory phase and the status of the patient’s lungs will determine the expiratory time [TE] The airway pressure during the expiratory phase will be a function of the patient’s RAW and the baseline pressure set on the mechanical ventilation. The TE will be a function of the TI, and to a great part to the patient’s RAW I:E ratio: comparisons of the TI to the TE. Due to the problems associated with positive pressure ventilation, the RCP spends a lot of time manipulating parameters to keep the I:E ratio at a reasonable level. P R E S S U R E TE = 1 second Ti = 1 second I:E ratio = 1:1 Normal I:E ratio during spontaneous breathing is 1:1.5, but to minimize some of the hazards of mechanical ventilation, with positive pressure ventilation, this ratio needs to be 1:2 or more. T I M E A patient with significant air-trapping may require much longer 1:E ratio such as 1:3, 1:4. Cycle time: the entire time of a full breath which include both TI & TE so the formula for cycle time = T I + TE Another formula for the cycle time is used when the RCP doesn’t know the I:E ratio. cycle time = 60 seconds/BPM Example60 second/12 BPM = 5 seconds cycle time If the respiratory rate is The cycle time is 15 8 6 Airway pressure: Pressures in cmH20 measured in the airways. Usually the pressure is actually measured at the outlet of the mechanical ventilator. Some may call this the trans-airway pressure PIP: peak inspiratory pressure is the highest pressure that is reached. Some ventilator parameters can be set so that the patient gets the same PIP with each breath, while other ventilators will give a uniform VT in which the PIP varies based on changes in the patient’s RAW PIP P R E S S U R e P Plateau baseline time or compliance. In the RAW formula, this PIP is the P1 P plateau: during a breath hold on positive pressure invasive ventilation, the airway pressure drops from the peak [PIP] down to this pressure. On a graphic, it looks like a flat plateau. This pressure is the P2 of the RAW formula and the Δ P of the static compliance formula Baseline pressure: After the positive pressure breath is given, the PIP is reached then the airway pressure returns to the baseline, which may be zero or a positive number. PEEP or CPAP are modes in which the baseline is raised over zero. The function of a raised baseline pressure is to increase alveolar pressure so that Pa02 can rise without increasing Fi02. PEEP or CPAP are both used to reverse refractory hypoxemia and are required in order to get toxic levels of Fi02 down. PAW: the “mean airway pressure” is the average airway pressure. It is a function of the inspiratory time, the PIP, the baseline pressure and the I:E ratio. There are two formulae for this parameter: PAW = [PIP ( TI)] + [PEEP (TE)] (TI + TE) this is the easiest to calculate, because the RT does not have to calculate the actual TI and TE: PAW = [PIP ( I )] + [PEEP (E)] [I + E] Example PAW = [10 ( 1 )] + [5 (2)] [1 + 2] PAW = [10 + 10] 3 PAW = 20/3 = 6.66 cmH20 If the PIP is I :E PEEP PAW 10 1:2 5 20 1:3 0 30 1:2 10 Positive pressure mechanical ventilation: mechanical ventilators that create positive airway pressure to create the required driving pressures to fill the alveoli. This can be invasive or non-invasive. Positive pressure ventilators generally send a flow rate of gas into the airways until a preset pressure or a preset VT has been reached. Negative pressure mechanical ventilation: mechanical ventilators that create negative pressure around the chest wall to create the driving pressure needed to ventilate the patient. Respiratory rates are set and negative pressures are selected to achieve the VE needed to normalize ABG. These forms of ventilation are considered non-invasive mechanical ventilation modes because they don’t need artificial airways. Fi02 adjustments are made by placing masks or nasal cannula on the patient’s face. Invasive mechanical ventilation: forms of positive pressure ventilation in which the patient must be intubated or has had a tracheostomy tube placed in order to create a patent airway so that gas can enter and leave the patient’s lungs. Non-invasive mechanical ventilation: many positive and negative pressure ventilators can be operated without the need for artificial airways. A face or nose mask is used to interface with the mechanical ventilator Ventilator modes: most modern positive pressure invasive mechanical ventilators have mode selection so that the clinician can select the level of support a given patient would need. Some modes such as Control or Assist/control modes are used for full ventilatory support, while other modes such as Intermittent Mandatory Ventilation [IMV/ SIMV] or are used for partial support. One can pick single modes or dual modes. Full-support mechanical ventilation: To rest a patient with respiratory fatigue, mechanical ventilation assumes all the WOB. This is usually done by positive pressure invasive mechanical ventilation. The patient is generally sedated, even paralyzed by drugs. Manipulation of the ventilator parameter will result in very specific, predictable changes in ABGs. Most fatigued patients need to be rested for 24-48 hours, but a serious complication of full-support is that after a few days, the patient’s respiratory muscles start to atrophy quickly. Partial-support mechanical ventilation: also called dual mode ventilation, in which the patient assumes some of the WOB. There are several types of dual mode ventilators for different needs. SIMV or IMV are examples of partial-support mechanical ventilation. Frequently patients are started on full support and are moved to partial support after the mandatory rest period. Spontaneous modes: When a patient is past the point of needing full or even partial support, we can challenge the patient by selection of various forms of low level Pressure support ventilation [PSV], or CPAP modes of ventilation in which the patient controls most, if not all of the parameters of ventilation with the machine acting only as a monitoring device with/without alarms and mechanical intervention in case of apnea or hypoventilation. Patients on spontaneous modes of ventilation must have an intact ventilatory drive, and must be able to maintain their PaC02 with little or no help from the machine. These modes of ventilation are used for hypoxemic respiratory failure type I. Frequently, non-invasive positive pressure ventilators are used in their spontaneous modes. Wave forms/graphics: electronic devices convert airway pressures, volumes or flows into a graphic with various parameters being on the x or on the y axis. Interpretation of these wave forms is complex and will be covered at a later date. Peak flows /flow rates: All modern positive pressure ventilators have peak flow rates. Some peak flows are selected while in some modes of ventilation, this parameter can be varied by the patient’s demand. The actual flow rate may not be the same all the way through the breath. Dependent on the mode selected or the type of ventilator used, the flow pattern may vary from the constant flow. Constant flow: The flow rate starts at peak flow and stays there until it drops to zero flow Descending ramp: the flow starts at the peak flow, and then as pressure rises in the system, it drops down gradually until zero flow is reached. F L Descending ramp Constant flow O W Sine wave Sine wave; the flow starts out slow and gradually rises to the peak flow then gradually TIME drops back to zero. The Sine wave is the closest to spontaneous breathing. VT To manipulate the ABG, we need a way to manipulate the V E, we can do this by selection of the respirator rate or by selection of the VT. Selection of the appropriate VT is determined by the patient’s disease state. We will go into this selection at great detail at a later date. Set VT Due to interaction between the patient airways & the ventilator’s circuit, the VT that we select on the dial may or may not be the same as the VT that the patient gets in his lungs Corrected VT : the circuit of the mechanical ventilator is a space that can accept a volume of gas and this circuit can swell in the face of high pressures so that even more volume can be compressed in the circuit. The more gas compressed into the circuit, the lower the actual VT that reaches the patient’s lungs. The corrected VT has been corrected for this compressible volume loss. We will discuss this in more detail at a later date. Summation There are many reasons why any patient goes on a ventilator. To optimize the effectiveness of our decision, we need to select the proper type of ventilation, the appropriate modes and settings that will optimize the patient’s oxygenation and ventilation while limiting the side effects. Reference: Boitano, L.J. Management of Airway Clearance in Neuromuscular Disease in Respiratory Care August 2006, vol 51 (8) pp. 913-921. Egan’s Fundamentals of Respiratory Care 9th edition David Chang Clinical Application of Mechanical Ventilation 3rd edition Susan Pilbeam & JM Cairo Mechanical Ventilation: physiology & Clinical Application. 4th edition