Pharmacology 17 – Treatment of Stomach and Duodenal
advertisement

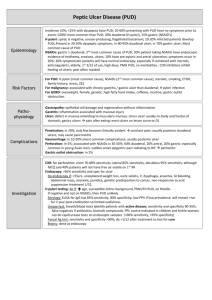
Pharmacology 17 - Treatment of Stomach and Duodenal Ulcers Anil Chopra 1. 2. 3. 4. 5. 6. 7. Describe the factors that impinge on the development of peptic ulcer disease. Explain why antibiotics feature prominently in the treatment of peptic ulcer disease. Using named examples, explain, with the use of a clearly labelled diagram, the mechanisms by which proton pump inhibitors and histamine (H2) receptor antagonists promote the healing of gastric ulcers Explain why misoprostol may be used in the treatment of iatrogenic peptic ulcer disease. Describe the mechanisms by which sucralphate and bismuth chelate are thought to be useful anti-ulcer drugs. Provide two examples of ‘triple therapy’ for peptic ulcer disease. What do you understand by the term ‘gastroesophageal reflux disease’ and how may it be treated? There are a number of different factors which protect the gastric and duodenal mucosa: - mucus produced in gastric and duodenal mucosa - HCO3- ions trapped in mucus generate a pH of 6-7 at mucosal surface - Prostaglandins stimulate the production of bicarbonate inhibit gastric secretion. The potential things that can degrade the mucosa include acid from the parietal cells and pepsinogen from the chief cells. When the processes are unbalanced then gastric and duodenal ulcers can form. Causes of Peptic Ulcer Disease Helicobacter pylori infection Increased acid secretion Reduced bicarbonate secretion Reduced thickness of the mucosal layer Increase in pepsin type 1 Decreased mucosal blood flow Risk factors: genetic predisposition, stress, smoking Prevalence: 1:10 of the population in developed countries Treatments Antibiotics Name – metronidazole, amoxicillin, clarithromycin, clarithromycin, bismuth Usage – to eliminate Helicobacter pylori (gram negative bacterium). The majority of patients with peptic ulcers are infected with the bacterium. A single antibiotic is not normally used – “triple therapy” is often adopted. Rationale for use: 50-80% of population chronically infected 10-20% of which go on to develop peptic ulcers or neoplasia 100% of patients with gastric cancer and 80-90% with ulcers are infected Routes of transmission of infection unsure – possibly animals/faeces or socioeconomic conditions Aim for 90% eradication in 7-14 days, eradication difficult – if part of treatment then recurrence falls from 80% to 5% Mode of Action & Side effects – see lecture on antibiotics Inhibitors Of Gastric Acid Secretion Proton Pump Inhibitors Name – omeprazole Usage – component of triple therapy used in peptic ulcers resistant to H2 antagonists as well as reflux oesophagitis Mode of Action – it inhibits gastric acid secretion by parietal cells by 90%. They are irreversible inhibitors of the H+/K+ ATPase and is inactive at a neutral pH. It accumulates in the canaliculi of the parietal cells which minimizes its effect on ion pumps elsewhere in the body. Side Effects & Pharmacokinetics - Orally active with few side effects. - Administered as enteric coated slow release formation. Histamine type 2 H2 receptor Antagonists Names - cimetidine, ranitidine Usage – gastric and duodenal ulcers Mode of Action – inhibit gastric acid secretion by 60%. They are antagonists at histamine type 2 receptors on parietal and chief cells. Side Effects and Pharmacokinetics - Orally active with few side effects although both inhibit P450 metabolism Antimuscarinics are also used. Cytoprotective Drugs Names – sucralphate Usage – gastric duodenal ulcers Mode of Action – it is a polymer containing aluminium hydroxide and sucrose octasulphate that acquires a strong negative charge in an acid environment which then binds to positively charged groups on proteins and polymers. This produces gel-like substances which coat and protect the ulcer and limit the pepsin degradation of mucus. It also increases prostaglandin, mucus and HCO3- secretion and reduces the number of H. pylori. Side Effects and Pharmacokinetics • Orally administered drug and therefore remains in G.I tract. • May cause constipation • Reduces absorption of some other drugs (e.g. antibiotics & digoxin) Names – bismuth chelate Usage – triple therapy Mode of Action & Side Effects and Pharmacokinetics -Same way as sucralphate Name - Misoprostol Usage – with NSAIDs when prescribed chronically & in gastric and duodenal ulcers. Mode of Action – it mimics the action of locally produced PG to maintain the gastroduodenal mucosal barrier. Side Effects - diarrhoea, abdominal cramps, uterine contractions. Do not use in pregnancy - Triple Therapy Triple therapy better than single drug therapy due to resistance: Example 1: o Metronidazole (useful against anerobic bacteria) or amoxycillin (broad spectrum) – depends on local pattern of resistance - - o Clarithromycin – antibiotic with macrolide structure, prevents translocations of bacterial tRNA o Proton Pump Inhibitor (PPI) – improves antibiotic efficiency by increasing gastric pH – improves stability and absorption Example 2: o H2 receptor antagonist o Clarithromycin o Bismuth Problems with triple therapy: Compliance Development of resistance Adverse response to alcohol –especially metronidazole (interferes with metabolism) Antacids Name – generally salts of magnesium Mg2+ and aluminium Al3+ Usage – non-ulcer dyspepsia, and GORD (gastro-oesophageal reflux disease) Mode of Action - neutralises acid, raises gastric pH, reduces pepsin activity GORD – gastroesophageal reflux disease Stomach and duodenal contents reflux into oesophagus Causes oesophagitis, chronically progressing to premalignant mucosal cells and potential oesophageal Adenocarcinoma Occasional and uncomplicated GORD: Heart burn May treat by self medication with antacids and H2 receptor antagonists Can also be treated with PPI’s Combine with drugs that increase gastric motility and stomach emptying – e.g. D2 receptor antagonists such as metaclopramide