Gastrointestinal drugs
advertisement

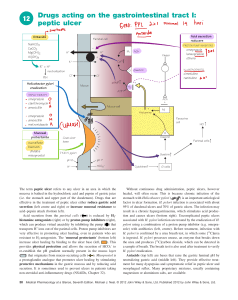
Gastrointestinal Drugs Part ⅠDrugs Used in Peptic Ulcer Ⅰ. peptic ulcer: [Symptoms and complications] [Pathogenesis]: the balance between muscosal defense and injury 1. Aggressive factors increased Helicobacter Pylori ( H. Pylori) and gastric acid and pepsin (1)Helicobacter Pylori ( H. Pylori) H. pylori is the most important pathogenic factor to peptic ulcer. “No H.P., no ulcer.” (2)gastric acid and pepsin:Pepsin can decompose protein molecule. Gastric acid is the key-factor of the formation of peptic ulcer. We also say that “No acid, no ulcer.” 2. Defensive factors decreased: mucus-bicarbonate barrier and prostaglandins (1)mucus-bicarbonate barrier: the epithelial layer of the mucosa is composed of tightly adjoined cells that are specialized for existence in an acid medium. Their tight junctions, synthesis of prostaglandins and secretion of mucus and bicarbonate all contribute to maintenance of the epithelial barrier. (2)prostaglandins: Prostaglandins also plays a major role in the maintenance of defensive mechanism. ⅡDrugs used to treat peptic ulcer include 1.eradicateing H. Pylori infection:Antimicrobial agents 2. reducing secretion of gastric acid or neutralizing the acid after it is released (1) H2-receptor antagonists (2) Antimuscarinic agents (3) Inhibitors of the proton pump (4) Antacids 3.providing agents that protect the gastric mucosa from damage (1)Prostaglandins (2)Mucosal protective agents 1. Antimicrobial agents : Optimal therapy of patients with peptic ulcer disease who are infected with H.Pylori requires antimicrobial treatment. Eradication of H.Pylori results in rapid healing of active peptic ulcers and low recurrence rates. Metronidazole, tetracycline, amoxiciliin, etc. Often combined with bismuth and omeprazole. 2. regulation of gastric acid secretion (1) H2-R(histamine H2 receptor) antagonists: cimetidine, ranitidine, famotidine and nizatidine [Actions] competitively block the binding of histamine to H2 receptor, completely inhibit gastric acid secretion induced by histamine [Clinical uses] ①peptic ulcers : effective. But after treatment is stopped, recurrence is common. ②Zollinger-Ellison syndrome : a fatal disorder in which a gastrin-producing tumor causes hypersecretion of gastric acid. H2 receptor antagonists can effectively keep the acid secretion to safe levels so as to control symptoms related to excess acid secretion. 1 ③gastroesophageal reflux disorder(GERD, heartburn): [Adverse reactions] 1. headache, dizziness, diarrhea and muscular pain; 2.CNS effects: occur primarily in elderly patients or after prolonged administration. (2)Antimuscarinic agents: muscarinic receptor stimulation increase gastrointestinal motility and secretory activity. So cholinergic antagonists can be used as adjuncts in the management of peptic ulcer disease and Zollinger-Ellison syndrome, particularly in patients refractory to standard therapies. Selective M1-receptor antagonist, Pirenzepine is a good choice as an antisecretory agent. 3.Inhibitors of the proton pump: Omeprazole(Lesec), lansoprazole, pantoprazole [pharmacological effects] Inhibits secreted gastric acid transporting to gastric lumen through the proton pump. [Clinical uses] ①peptic ulcer: superior to H2-R antagonists ②Zollinger-Ellison syndrome: ③gastroesophageal reflux disease:the most effective agents. [Adverse reactions] extremely safe. ①common side effects: diarrhea, headache, abdominal pain etc. ②overgrowth of bacteria: gastric acid is an important barrier to bacterial colonization of the stomach and small intestine. Increases in gastric bacterial concentrations are detected in patients taking proton pump inhibitors. 4. Antacids: weak bases : Mg(OH)2 , Al(OH)3 , CaCO3 , NaHCO3 actions: antiacids are weak bases that react with gastric hydrochloric acid to form a salt and water. Commonly used antiacids are salts of aluminum and magnesium, such as magnesium hydroxide and aluminum hydroxide, either alone or in combination. In some cases, we can also use sodium bicarbonate (baking soda) or calcium carbonate. 5. prostaglandins: prostaglandins E2 and I2, inhibit secretion of HCl and stimulate secretion of mucus and bicarbonate. A deficiency of prostaglandins is thought to be involved in the pathogenesis of peptic ulcers. Misoprostol: a stable analog of PGE2 6.Mucosal protective agents: these compounds, known as cytoprotective, have several actions that enhance mucosal protection mechanisms, thereby preventing mucosal injury, reducing inflammation and healing existing ulcers. Sucralfate:complex of aluminum hydroxide and sulfated sucrose Mechanism of effect: (1)it creates a physical barrier by forming complex gels with mucus. (2)It also stimulates prostaglandins release and mucus and bicarbonate output. colloidal bismuth [actions] 1) binds to an ulcer crater, coating it and protecting it from acid and pepsin. 2) Inhibits the activity of pepsin 3) increases mucous secretion 4) helps to eradicate H. pylori 2 PART 2 Antidiarrheals Antidiarrheals: increased motility of the gastrointestinal tract and decreased absorption of fluid are major factors in diarrhea. antimotility agents: diphenoxylate Opioids are the most effective agents for relief of diarrhea. Diphenoxylate is an analogue of meperidine and have opioid-like actions on the gut. 2.adsorbents: such as kaolin, pectin and activated charcoal are widely used to control diarrhea 3. agents that modify fluid and electrolyte transport: some NSAIDs such as aspirin and indomethacin are effective in controlling diarrhea. Part3 Laxatives Laxatives are commonly used to accelerate the movement of food though the gastrointestinal tract. These drugs can be classified on the basis of their mechanism of action as irritants or stimulants of the gut and bulking agents. 1. irritants or stimulants :castor oil, senna and aloe actions: is very irritating to the gut and promptly increase peristalsis 2. bulking agents: hydrophilic colloid from indigestible parts of fruits and vegetables actions: form gels in the large intestine, causing water retention and intestinal distension, thereby increasing peristaltic activity. 3