GF Tier II Eligibility Determination
advertisement

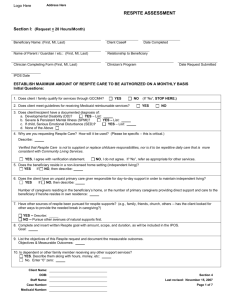
GF Enhanced Benefit Plan Tier II Determination Consumer: Primary Case Holder: Date of Review: Staff Completing Review: ___ Initial Determination Case Number: Program: Title: ___ Continuing Determination In order to determine consumer eligibility and authorization for services from the GF Enhanced Benefit Plan, the following criteria should be used: I. Medicaid (check or attach Medifax) Does Consumer have Medicaid? Yes No If Yes, the necessary supports/services are authorized through Medicaid plan. If no, Was Medicaid applied for? [ ]Yes [ ] No If Yes, When was it applied for and what is status? If applied for and denied what is the reason for denial? If No, an application will be submitted by: II. Other Insurance/Third Party Payors 1. Does Consumer have other insurance/third party payors? (BCBS/Medicare/private insurance) Yes No If yes, the necessary supports/services are authorized through that benefit plan III. Alternative Supports/Services 1. What alternative supports/services have been accessed? List sources accessed and rationale for denial: IV. Hospitalization/More Restrictive Placement 1. Is there imminent risk of hospitalization if services are denied? Explain: Yes No 2. Is there imminent risk for more restrictive placement if services are denied? Yes No Explain: V. Medical Necessity/Amount/Scope/Duration 1. What are the types of services being requested? GF Enhanced Benefit Plan Tier II Determination Page 2 of 3 2. What is the amount of services? (number of units) What is the scope of services? (who/how/where)? What is the duration of services? (length of time to be provided) 3. Are these services consistent with the Diagnosis, symptoms, functional impairment and necessary to meet the needs of the consumer? Yes No Explain: 4 Are these services the most cost effective? Explain: Yes No 5. Are these services provided in the least restrictive environment? Explain: 6. Are these services consistent with clinical standards of care? Explain: Yes Yes No No 7. What is the criteria for discharge or to transition to less intensive supports and services? VI. Frequency of Evaluation 1. At what frequency will this plan be evaluated for continuation of GF Enhanced services? If over or under utilization of authorized services occurs, how will this be reviewed? Include rationale for time frame.: Primary Caseholder Signature VII. Date: Determination/Authorization 1. Eligible for GF Enhanced Benefit Plan? Yes No 2 Approve of Services Requested (including Amount, Scope, and Duration) [If plan includes Trained Respite Sitter or Family Friend Respite, must complete Section VIII] Yes No Form #021 Reference: General Fund Specialty Services Plan Rev: 12/05 D:\106735607.doc GF Enhanced Benefit Plan Tier II Determination Page 3 of 3 If No, explain specific services (including amount, scope, and duration), that will be approved: 3. If approving children’s group home or any child or adult partial hospitalization other than LADT, has the required approval from the Medical Director (or designee) been obtained? Yes No Next Review Date: (Must review within 90 days) Supervisor signature: VIII. Date Respite: Does this plan include: 1. Family Friend Respite at a level that would project to 100 hours or more annually? Yes No 2. Trained Respite Sitter services that would project to 180 hours or more annually? Yes No If yes to either or both, approval signature is required below: Family Friend Respite Plan: Approved Denied N/A Trained Respite Sitter Plan: Approved Denied N/A Division Director/Assistant Division Director/ Contract Manager Date Note: This form must be filed in the case record with the appropriate IPOS/Periodic Review/Amendment Service Authorization Summary. Form #021 Reference: General Fund Specialty Services Plan Rev: 12/05 D:\106735607.doc