Retropharyngeal abscess : Guideline
advertisement

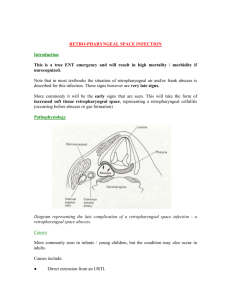
Retropharyngeal abscess : Guideline See Also Neck Lump Guide Line *Prior to reading this guideline* Any neck lump associated with any respiratory symptoms need URGENT ENT review Definition Retropharyngeal abscess is a collection of pus in the deep tissues in the back of the throat. Background Retropharyngeal abscess generally affects children under age 5. Retropharyngeal abscess (RPA) occurs much less commonly today than in the past because of the widespread use of antibiotics for suppurative upper respiratory infections. RPA, once almost exclusively a disease of children, is observed with increasing frequency in adults. RPA poses a diagnostic challenge because of its rare occurrence and variable presentation. Early recognition and aggressive management of RPA are essential because RPA still carries significant morbidity and mortality The retropharyngeal space can become infected in 2 ways. Either infection spreads from a contiguous area or the space is inoculated directly secondary to penetrating trauma. Pathophysiology: The retropharyngeal space is posterior to the pharynx, bound by the buccopharyngeal fascia anteriorly, the prevertebral fascia posteriorly, and the carotid sheaths laterally. It extends superiorly to the base of the skull and inferiorly to the mediastinum. The high mortality rate of RPA is owing to its association with airway obstruction, mediastinitis, aspiration pneumonia, epidural abscess, jugular venous thrombosis, and erosion into the carotid artery. Causes : Infection : Typically, an upper respiratory infection (URI) causes spread to retropharyngeal lymph nodes, which form chains in the retropharyngeal space on either side of the superior constrictor muscle. Sources of infection can include pharyngitis, tonsillitis, adenitis, otitis, sinusitis, and other infections (ie, nasal, salivary, dental). Infectious sources (eg, osteomyelitis of the spine) also can spread anteriorly from the prevertebral space. Abscesses in this space can be caused by the following organisms: Aerobic organisms, such as beta-hemolytic streptococci and Staphylococcus aureus Anaerobic organisms, such as species of Bacteroides and Veillonella Gram-negative respiratory organisms, such as Haemophilus influenzae Trauma : Penetrating trauma is involved prominently in retropharyngeal space infection. Accidental lacerations are not uncommon in children who run and fall down after they have placed an object (eg, toy, stick, frozen popsicle, lollipop, toothbrush) in their mouths. Foreign bodies (eg, fishbones) also have been implicated in penetrating trauma to the retropharyngeal space. Iatrogenic causes of inoculation to this space include instrumentation with laryngoscopy, endotracheal intubation, surgery, endoscopy, feeding tube placement, and dental injections and procedures. Assessment 1. Clinical History History is variable, depending on the age group. Symptoms are different for young adults, children, and infants Patients with retropharyngeal abscess present with constitutional complaints such as fever, chills, malaise, decreased appetite, and irritability. Patients may complain of sore throat, difficulty swallowing (dysphagia), pain on swallowing (odynophagia), jaw stiffness (trismus), or neck stiffness (torticollis), head hanging to one side. Patients also may complain of muffled voice, the sensation of a lump in the throat, and/or pain in the back and shoulders upon swallowing. Difficulty breathing is an ominous complaint that signifies impending airway obstruction. (usually a late sign) Patient history is not always straightforward. Symptoms in young adults Sore throat Fever Dysphagia Odynophagia Neck pain Dyspnea Symptoms in children older than 1 year Sore throat (84%) Fever Neck stiffness Odynophagia Cough Symptoms in infants Fever (85%) Neck swelling (97%) Poor oral intake (55%) Rhinorrhea (55%) Lethargy (38%) Cough (33%) 2. Physical Symptoms Most patients with retropharyngeal abscess are febrile. Some appear toxic and irritable. Cervical lymphadenopathy, usually unilateral, is the most common physical finding in these patients. Patients may have decreased or painful range of motion of their necks or jaws. A neck mass or tenderness may be appreciated Dysphonia Patients in respiratory distress or those who present with stridor or drooling have potential airway compromise. These patients prefer to lie supine with their necks extended, maximizing their airway patency. Sitting up or flexing their necks worsens their respiratory distress. Physical signs in young adults Cervical lymphadenopathy Nuchal rigidity Posterior pharyngeal oedema (37%) Fever Drooling Stridor Physical signs in infants and children Cervical lymphadenopathy (83%) Retropharyngeal bulge (43%; do not palpate in children) Fever (86%) Stridor (3%) Torticollis (18%) Neck stiffness (59%) Drooling (22%) Agitation (43%) Neck mass (91%) Lethargy (42%) Respiratory distress (4%) Associated signs including tonsillitis, peritonsillitis, pharyngitis, and otitis media Investigations Consider the following : However if airway compromise get help and do investigations in a controlled environment. 1. FBC CRP Blood Culture, Throat Swab 2. Lateral Chest X ray 3. CT Neck Management Stay calm (you and the patient) If Retropharyngeal abscess suspected ask for senior help. URGENT ENT review Will need Neck imaging Do Not examine throat If airway compromise urgently contact ENT, Anaesthetics and Paediatric consultants on call. IV access and start antibiotics on the ward if no airway compromise If Airway compromise IV access should be obtained in theatre with ENT team avaliable Notify PICU Once the airway has been secured surgical drainage of the collection needs to be considered- send pus for urgent microscopy and culture if collection drained Antibiotic choice.: IV Cefuroxime and Metronidazole (if anaphylasis with penicllins or cephalosporin allergy discuss with the on-call medical microbiologist) For doses see BNF for children Complications 1. 2. 3. 4. 5. 6. 7. 8. 9. Airway obstruction Mediastinitis Pleural involvement Atlantooccipital dislocation Epidural abscess Sepsis Adult respiratory distress syndrome (ARDS) Erosion of the second and third cervical vertebrae Cranial nerve deficits (cranial nerves IX-XII are contained in the cervical fascia) 10. Septic thrombosis of jugular vein or hemorrhage secondary to erosion into carotid artery. Prognosis: Prognosis generally is good if RPA is identified early, managed aggressively, and complications do not occur. The mortality rate may be as high as 40-50% in patients in whom serious complications develop References www.emedicine.com/emerg/topic506.htm http://www.emedicine.com/ped/topic2682.htm www.nlm.nih.gov/medlineplus/ency/article/000984.htm