Stridor and Upper Airway Obstruction
advertisement
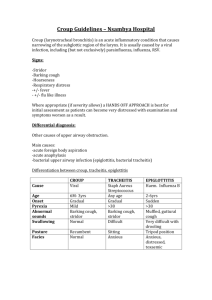
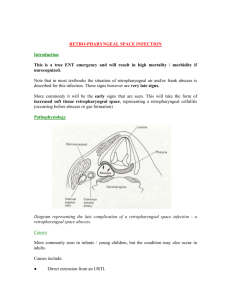
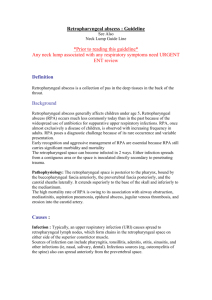
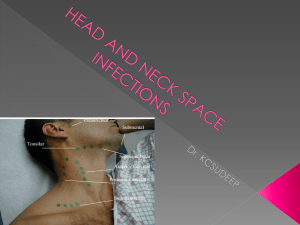
Stridor and Upper Airway Obstruction Kevin R Schwartz Massachusetts General Hospital Department of Pediatrics Stridor: Definition Extrathoracic obstruction: -Supraglottic: epiglottitis, retropharyngeal abscess, diptheria, anaphylaxis -Glottic/Subglottic: croup, laryngomalacia, vocal cord paralysis Intrathoracic obstruction: -foreign body aspiration, compression by lymph nodes or tumor, vascular wings/webs Stridor: Differential Diagnosis • State the main ideas you’ll be talking about Viral Croup • Pathophysiology: viral infection with measles, parainfluenza type I and 3, influenza A/B, RSV or metapneumovirus causeslaryngo tracheobronchitis. Edema in the subglottic region, which is bound by the cricoid cartilage causes upper airway narrowing. • Epidemiology: Mainly affects children aged 6mos to 3yrs with peak incidence in second year of life. Boys>girls. Viral Croup • Clinical Presentation: Often antecedent URI symptoms x12-48 hours followed by onset of “barky” characteristic cough, hoarse voice, stridor and respiratory distress, may be accompanied by fever as high as 40 C but patient should NOT drool or appear toxic • Physical Examination Findings: Observe pt’s positioning (?sniffing position), mental status, retractions/flaring, cyanosis, stridor at rest vs. w/ agitation, hydration status, Viral Croup • Labs/Studies: Labs uneccessary for diagnsosis and obtaining bloodwork may be distressing to patient, worsening condition. AP and lateral neck radiographs: Viral Croup: Treatment Viral Croup: Treatment Viral Croup: Treatment Bjornson, CL et al. Croup. The Lancet 2008;371:329339 d/c home admit Diptheria: Pathophysiology and Epidemiology • Pathophysiology: Corynebacterium diptheriae(gram-positive pleomorphic bacillus) infects upper respiratory tract and, after 2-4 days incubation, elaborates a toxin which causes necrosis of mucous membranes and formation of pseudomembranes. The toxin may also affect heart, nerves and kidneys. • Epidemiology: endemic in Africa, Asia, South America. V. rare in immunized populations, mostly affecting children <15y/o Diptheria: Clinical Presentation • Nasal Diptheria(most often in infants): mild rhinorrhea which progresses to malodorous, mucopurulent drainage • Tonsillar/Pharyngeal Diptheria: begins w/ malaise, low-grade fever and pharyngitis. Membrane appears within 1-2 days with cervical lymphadeneitis and edema • Laryngeal Diptheria: often an extension of pharyngeal infection, presents similar to croup. • Complications: - Neuro: paralysis of soft palate or diaphragm, peripheral neuropathies, loss of DTRs. -Cardiac: myocarditis may occur anywhere from 1st to 6th week of illness, usually transient Diptheria: Clinical Presentation In general, attempts to remove the membrane result in bleeding. Diptheria: Treatment Diptheria: Treatment - If signs of incipient airway obstruction, tracheostomy should be performed. Orotracheal intubation is an alternative BUT may dislodge the pseudomembrane and fail to relieve the obstruction. Diptheria: Complications and Public Health Measures Foreign Body • Epidemiology: Seen in children > 6m/o, with incidence peaking ~2-3 y/o • Clinical Presentation: Acute onset of stridor in the child with no antecedent illness or fever of the appropriate age group. • Labs/Studies: Radio opaque objects may be visible on X ray. Retropharyngeal Abscess: Pathophysiology and Epidemiology • Usually an antecedent pharyngitis causes suppuration of retropharyngeal lymph nodes with subsequent abscess formation in the retropharyngeal space. • Occur most commonly in children aged 2 to 4y/o, majority of cases occur in children <6y/o • Microbiology includes: Strep pyogenes, Staph aureus, Haemophilus, and respiratory anaerobes. Retropharyngeal Abscess: Clinical Presentation • Clinical Presentation: Fever, dysphagia, drooling, odynophagia, stridor. Often with unwillingness to move the neck, trismus is unusual. A fluctuant mass may be palpable in posterior pharyngeal wall. Retropharyngeal Abscess: Imaging • Lateral neck film: Should be obtained with neck in extension during inspiration. • Retropharyngeal space considered widened if wider than adjacent vertebral body or greater than 7mm at C2 or 14mm at C6 Retropharyngeal Abscess: Management • Antibiotics: -Ampicillin/Sulbactam 50mg/kg IV q6 until afebrile then Amox/Clav 45mg/kg PO q12 or clindamycin 13mg/kg q8 x 14days total. • Surgery: -indicated for large abscesses and those which do not respond to antibiotics alone. Peritonsillar Abscess: Pathophysiology and Epidemiology • Antecedent pharyngitis progresses to abscess formation in superior pole of tonsil. Microbiology is the same as that for retropharyngeal abscess. • May occur at any age but most common in young teenagers Peritonsillar Abscess: Clinical Presentation • Typical presentation is severe sore throat, fever and a muffled “hot potato” voice. Drooling may be present, trismus is common • Physical Examination: Unilateral tonsil swelling or visible abscess in tonsil with uvular deviation to the other side, exam often limited by trismus. Peritonsillar Abscess: Management • Antibiotics: Same as for retropharyngeal abscess • Surgery: Older more cooperative child may be able to undergo needle aspiration or simple I and D as an outpatient. Younger children unable to cooperate require drainage in the OR. • If there have been prior episodes of abscess or recurrent pharyngitis, a quinsy tonsillectomy is indicated. • Antibiotics alone usually inadequate treatment, however a 24 hour admission for antibiotics, hydration and analgesia may be trialled if the patient’s airway is not compromised. Complications of Deep Neck Infections • • • • • • Airway obstruction Septicemia Thrombosis of the internal jugular vein Mediastinitis Carotid artery rupture Lemierre’s Syndrome (infection of vessels of carotid sheath causing bacteremia and metastatic spread of infection to lungs and mediastinum.) Epiglottitis: Epidemiology and Pathophysiology • Pathophysiology: Cellulitis of the epiglottis and aryepiglottic folds with edema causing obtruction of airflow during inspiration. Most cases 2/2 H. flu type B, other pathogens include: H. flu other, Strep pneumo, Staph aureus, Strep pyogenes • Most cases occur in children 1-5y/o with a peak at 3y/o. Hib vaccine has dramatically reduced incidence. Epiglottitis • Clinical Presentation: ABRUPT onset of high fever(>38.8), severe sore throat, dysphagia and drooling. Child generally appears toxic and generally sits with neck hyperextended and chin thrust forward. • Physical Exam: stridor not generally present or not prominent, increase WOB not apparent, but inspiratory distress. Generally, direct visualization of throat is contraindicated as this may cause agitation precipitating complete airway obstruction. Leukocytosis >20K generally present on CBC with left shift. Epiglottitis: Imaging Lateral neck film shows “thumb sign” Epiglottitis: Management • 1) Airway – Patient should be nasotracheally intubated in an OR setting with a team standing by who can perform tracheostomy. Usually patient remains intubated x 2-3 days. • 2) Antibiotics: Oxacillin/Nafcillin(50mg/kg IV Q6) AND Ceftriaxone 50mg/kg IV QD x7-10 days. References • Wald, E et al. Peritonsillar and Retropharyngeal Abscess in Children. www.uptodate.com 2008 • Woods, C et al. Epiglottitis. www.uptodate.com 2008 • Quintero, D et al. Assesment of stridor in children. www.uptodate.com 2008 • Pocket Book of Hospital Care for Children, WHO 2005 • Schwartz, W The 5-Minute Pediatric Consult. Philadelphia: Lipincott William and Wilkins 2005