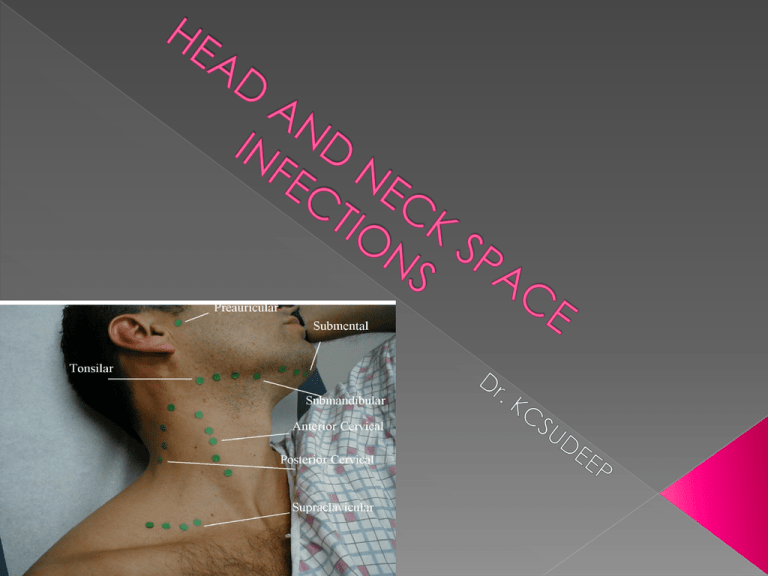
HEAD AND NECK SPACE INFECTIONS
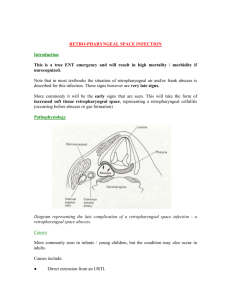
advertisement
PERITONSILLAR ABSCESS(QUINSY) It is a collection of pus in the peritonsillar space which lies between capsule of tonsil and the superior constrictor muscle. AETIOLOGY: Usually follows acute tonsillitis or denovo without history of sore throat. First crypta magna get infected and sealed off . Which forms the intratonsillar abscess which then brust through tonsillar capsule causing peritonsillitis and then abscess. CLINICAL FEATURES: Peritonsillar abscess mostly affects adults and rarely children. Usually it is unilateral. Clinical features are divided into : A)General: they are due to septicaemia .they include fever chills and rigors, general malaise , body aches, headache, nausea and constipation. B) Local: Severe pain in throat usually unilateral. Marked odynophagia. Patient is usually dehaydrated. Muffled and thick speech, often called “ hot potato voice” Foul breath due to sepsis in oral cavity and poor hygiene. Ipsilateral earache.( ref pain via CN IX which supplies both tonsil and ear. Trismus due to spasm of pterygoid muscles . EXAMINATION: 1) Tonsil, pillars and soft palate on involved side are swollen and congested. Tonsil itself may not appear enlarged as it gets buried in the oedematous pillars. 2) Uvula is swollen and oedematous and pushed to opposite side. 3)Bulging of soft palate and anterior pillar above tonsil. 4)Mucopus may be seen covering the tonsillar region. 5) Cervical lymphadenopathy. Involves jugulodiagastric nodes. 6)Torticollis– to the side of the abscess INVESTIGATION SWAB CULTURE : GROWTH OF Strep pyogenes, Staph. Aureus or anaerobic organisms. More often the growth is mixed, with both aerobic and anaerobic organism. TREATMENT: Hospitalisation Intravenous fluids for dehydration. IV Antibiotics covering both aerobic and anaerobic Analgesics Oral hygiene. If frank abscess has formed incision and drainage should be done. Interval tonsillectomy: tonsils are removed 4-6 weeks following an attack. Abscess or hot tonsillectomy. COMPLICATIONS: Parapharyngeal abscess Oedema of larynx Septicaemia Pneumonitis or lung abscess Jugular vein thrombosis. Spontaneous haemorrhage from carotid artery or jugular vein. APPLIED ANATOMY: It lies behind the pharynx between the buccopharyngeal fascia covering phayngeal constrictor muscles and prevertebral fascia. It extends from base of skull up to bifurcation of trachea. This space is divided into two lateral compartment by fibrous raphe. Retropharyngeal space infection can pass down behind oesophagus into mediastinum. PREVERTEBRAL SPACE: It lies between the vertebral bodies posteriorly and prevertebral fascia anteriorly. It extends from base of skull to coccyx. Infection of this space usually comes from caries of spine. Abscess of this space produces midline bulge. ACUTE RETROPHARYNGEAL ABSCESS Aetiology: Commonly seen in child below 3 yrs. It result from suppuration of retropharyngeal lymphnodes. In adult it may result from penetrating injury of posterior pharyngeal wall or cervical oesophagus. CLINICAL FEATURES: Dysphagia and difficulty in breathing are prominent symptoms. Stridor and croupy cough may be present Torticollis. Bulge in posterior pharyngeal wall usually seen on one side of midline. X-ray soft tissue neck lateral view show widening of prevertebral shadow. TREATMENT: Incision and drainage of abscess. Systemic antibiotics. Tracheostomy. CHRONIC RETROPHARYNGEAL ABSCESS AETIOLOGY: It is tubercular in nature and is the result of 1.Caries of cervical spine 2.TB infection of retropharyngeal lymphnodes secondary to TB of deep cervical nodes. The former presents centrally behind the prevertebral fascia while the latter is limited to one side of midline as in true retropharyngeal abscess CLINICAL FEATURES: Discomfort in throat. Dysphagia but not marked. Posterior pharyngeal wall shows a fluctuant swelling centrally or on one side of midline. Neck may show TB lymphnodes. TREATMENT: Incision and drainage: Can be done through a vertical incision along the anterior border of sternomastoid or along its posterior border. Full course of antitubercular therapy should be given. PARAPHARYNGEAL ABSCESS Also known as pharyngomaxillary or lateral pharyngeal space. APPLIED ANATOMY: Parapharyngeal space is pyramidal in shape with its base at the base of skull and its apex at hyoid bone. MEDIAL: buccopharyngeal fascia covering the constrictor muscles. POSTERIOR: prevertebral fascia . LATERAL: medial pterygoid muscle, mandible and deep surface of parotid gland. Styloid process and muscles attached to it divide parapharyngeal space into anterior and posterior compartments. Anterior compartment is related to tonsillar fossa. Posterior compartment is related to post part of lat. Pharyngeal wall medially and parotid gland laterally. Through post. Compartment pass the carotid artery, jugular vein, IX,X,XI,XII th cranial nerves and sympathetic trunk. Infection of parapahryngeal space can occur from: Pharynx Teeth Ear Other spaces like infection of parotid, retropharyngeal and submaxillary spaces. External trauma. CLINICAL FEATURES: It depends upon compartment involved. Anterior compartment: Prolapse of tonsil and tonsillar fossa. Trismus due to spasm of medial pterygoid muscle. External swelling behind the angle of jaw. Marked odynophagia. Posterior compartment: Bulge of pharynx behind the posterior pillars. Paralysis of CN IX, X, XI,XII and sympathetic chain Swelling of parotid region. There is minimal trismus or tonsillar prolapse. Fever , odynophagia, sore throat, torticollis and sign of toxaemia are common to both compartments. TREATMENT: Systemic antibiotics. Drainage of abscess. COMPLICATIONS: Acute edema of larynx with respiratory obstruction. Thrombophlebitis of jugular vein with septcaemia. Spread of infection to retropharyngeal space. Spread of infections to mediastinum along carotid space. Mycotic aneurysm of carotid artey. Carotid blow out with massive haemorrhage. Caused due to elongated styloid process or calcification of stylohyoid ligament. Patient complains of pain in tonsillar fossa and upper neck which radiates to the ipsilateral ear. It gets aggaravated on swallowing Diagnosis can be made by transoral palpation of the styloid process in the tonsillar fossa and by a radiograph such as anteroposteror view with open mouth or lateral view of skull. Many persons may have elongated styloid process but remain asymptomatic and do not need treatment Symptomatic styloid process can be excised by transoral or cervical approach. PBL Case 34: A 25 year old farmer has been complaining of nasal obstruction, greenish nasal discharge and nasal deformity of one year duration. On examination the nose was broad and contained a lobulated firm mass that may bleed on touch. Also, there was a hard swelling below the medial canthus of the right eye. One week ago, he noticed a change in his voice that was followed by respiratory distress. On examination there was marked stridor and laryngeal examination showed a subglottic laryngeal web.