Deep neck space abscesses
advertisement

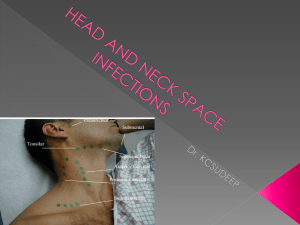
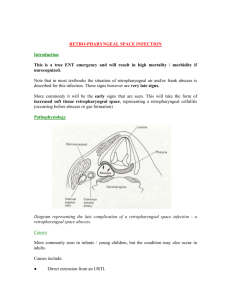
Deep neck space infections fascial compartments of the neck Superficial cervical fascia Deep cervical fascia superficial, middle, and deep layers. The superficial (investing) layer of the deep cervical fascia invests the sternocleidomastoid, trapezius, strap muscles, parotid and submandibular The middle (visceral) layer surrounds the thyroid gland, esophagus and trachea. The deep layer of the deep cervical fascia splits into prevertebral and alar layers. The prevertebral layer lies immediately adjacent to the vertebral bodies . All contribute to the carotid sheath so that infection of any layer may spread directly to involve the great vessels of the neck, which have direct communication to the chest. catastrophy Carotid artery rupture has a 20-40% mortality rate. Jugular vein thrombosis had a mortality rate of 60% prior to the use of antibiotics. Identifying this complication is essential. Osteomyelitis and vertebral erosion can cause subluxation and subsequent spinal cord injury. In older children and adults, the disease spreads directly into the fascial planes and is a more deadly Mediastinitis has a 40-50% mortality rate secondary to sepsis. Acute necrotizing mediastinitis and purulent pericarditis with tamponade also can be fatal. Anatomic Considerations The most common sources of life-threatening soft tissue infections of the head and neck are the dentition and tonsils. Most infections are polymicrobial and the responsible bacteria are often normal flora (Bacteroides, Peptostreptococcus, Actimomyces, Fusobacterium etc). that become virulent and invasive when normal barriers are broken (ie. tonsillitis, dental abscess, trauma). Obligate anaerobes frequently outnumber the anaerobes. iatrogenic Deep space infections can be secondary to instrumentation of the upper respiratory tract. Laryngoscopy Endoscopy Feeding tube insertion Endotracheal intubation Head and neck surgery Dental procedures Injections parapharyngeal space This space (also called the lateral pharyngeal space or pharyngomaxillary space) occupies a critical area in the neck, as it communicates with all other fascial spaces. It sits as an inverted cone with its base at the base of skull and apex at the hyoid bone. It can be divided into anterior (prestyloid) and posterior (retrostyloid) compartments by the styloid process. The anterior compartment contains only fat, lymph nodes and muscle. The posterior compartment contains the carotid and internal jugular vessels, as well as cranial nerves IX through XII. Parapharyngeal space Laterally Medially parotid gland,parotid fascia, medial pterygoid,mandible pharynx separated by sup.cons Posteriorly communicates with retropharyngeal space Superiorly base of skull, Inferiorly sub mandibular gland fascia Parapharyngeal space infection/abscess It can spread from Tonsillitis ,post tonsillectomy 60% Dental infections lower last molars 35 % Trauma Communication with peritonsillar,retropharyngeal or submandibular space causes Tonsillitis Peritonsillar abscess Dental infections Mastoiditis rarely via petrous apex,digastric muscle sheath Pharyngeal F.B Clinical features Pain throat,difficult swallowing Trismus , spasm of pterygoids Pyrexia,malaise, Painful external swelling in neck at the posterior part of middle third of sternomastoid Swelling in retromolar region Tonsil pushed medially Last cranial nerves palsies Parotid pushed laterally CT scanning is the imaging modality of choice and is helpful in confirming which compartments are involved. Treatment Systemic antibiotic In complicated cases such as septic jugular vein thrombosis, several weeks of intravenous antibiotics may be required. Incision and drainage Vertical incision at the ant.border of scm tracheostomy Complications Acute laryngeal oedema Septecimia and ijv thrombophelibitis Mediastinitis Spread to other spaces of neck Retropharyngeal space Lies between prevertebral and buccopharyngeal fascia Extending from skull base to tracheal bifurcation Continous below with sup.mediastinum and laterally with parapharyngeal space Retropharyngeal space infection/abscess Acute in infants more than 50% due to lymphadinitis secondary to URTI high grade temp sore throat head extension and neck stiffness respiratory & feeding problems Retropharyngeal space infection/abscess Croupy cough Muffled voice Cervical lymphadenopathy Smooth swelling on one side of post.ph.wall with airway impairement May obstruct post.nares May push the palate down Infant spine short and larynx high Causes: predisposing infections pharyngitis, tonsillitis, otitis, adenitis, sinusitis, and nasal, salivary, and dental infections. from contiguous spaces, such as the parapharyngeal space (eg, abscesses), submandibular space (eg, Ludwig angina), or prevertebral space (eg, osteomyelitis, diskitis). secondary to penetrating trauma. Running and falling down after putting something in their mouths (eg, toy, stick, popsicle, lollipop, toothbrush) is not unusual in children. Because parents may be unaware of these predisposing events Age Almost exclusively a pediatric diagnosis. Most incidents occur in children aged 6 months to 6 years, with a mean age of 3-4 years. Other deep neck abscesses (eg, parapharyngeal, peritonsillar) are observed more frequently in adults and older children. Physical Most patients are febrile. Some appear toxic and irritable. Cervical lymphadenopathy, usually unilateral, most common decreased or painful range of motion of their necks or jaws. A neck mass or tenderness may be appreciated. may present with a muffled "hot potato" voice (ie, dysphonia) or with a voice that sounds like a duck quack (ie, cri du canard). may be able to appreciate a mass in the posterior pharyngeal wall. As many as 30% of patients have this mass This is not midline,. "Tracheal rock sign" elicits pain Physical Patients in respiratory distress or those who present with stridor or drooling have potential airway compromise. These patients prefer to lie supine with their necks extended, maximizing their airway patency.. Address vascular complications in the physical examination. Jugular vein thrombophlebitis may manifest as tender induration at the anterior sternocleidomastoid border, vocal cord paralysis, or sepsis of an unknown source. Carotid artery rupture can be heralded by sentinel bleeding from the ear, nose, or mouth. In Adults Likely to be due to tuberculous infection of the cervical spine Slow onset Pharyngeal discomfort,some dysphagia Cervical spine radiography Look for associated infections Imaging Studies A lateral soft tissue neck x-ray is helpful . An abscess occupies the soft tissue space, which can be observed between the radiolucent airway (ie, pharynx, trachea) and the spine. Widening of these soft tissues is pathologic until proven otherwise. Ultrasound An imaging modality that is gaining popularity. It is safer than CT scan, since it is portable and does not use radiation. Ultrasound is also less traumatic to children, requiring less frequent use of sedation. CT scanning is currently the imaging modality of choice.. can be used to determine the presence of an abscess and help distinguish it from cellulitis (an abscess has a central area of lucency). also can assist in determining the location of the abscess, extent of abscess spread, and presence of any complications. CT scan can be more than 90% sensitive. MRI produces superior images , used when the abscess has spread to the CNS. this requires a period of time when the patient is in an unmonitored setting. Children usually require sedation for this test, which is also dangerous in any patient with a potentially unstable airway. Needle aspiration of a suspected abscess Aspiration can help determine the presence of an abscess and help distinguish it from cellulitis. It can be diagnostic and therapeutic. An intraoral route usually is indicated, except when an abscess is isolated lateral to the carotid sheath. In this case, an external approach can be used. CT scan or ultrasound can help guide the aspiration. With an abscess involving multiple spaces, perform needle aspiration with an open external approach. Complications of retropharyngeal abscesses are secondary to mass effect, rupture of the abscess, or spread of infection. Rupture of the abscess can cause aspiration of pus, resulting in asphyxiation or pneumonia.. Spread of the infection to the mediastinum can result in mediastinitis, purulent pericarditis ,etc. Spread of the infection laterally can involve the carotid sheath and cause jugular vein thrombosis or carotid artery rupture. Posterior spread of infection can result in osteomyelitis and erosion of the spinal column, causing subluxation and spinal injury. It can evolve into necrotizing fasciitis, sepsis, and death Treatment Incision and drainage Limitation of GA Infant wrapped and held upright Abscess incised with a gaurded knife Sinus forceps plunged into it and open Copious flow of pus Baby face turned down to allow escape Immediate relief Antibiotics Treatment Incision and drainage over the post.border of scm vertical incision Abscess is sought for by dissection between the carotid sheath and the prevertebral muscles and is drained from the neck Tracheostomy Anti TB regimes Submandibular Space The submandibular space extends from the hyoid bone to the mucosa of the floor of the mouth. It is bound anteriorly and laterally by the mandible and inferiorly by the superficial layer of the deep cervical fascia. The mylohyoid muscle acts as a sling across the mandible and divides the submandibular space into sublingual and submylohyoid spaces. Ludwig angina The infection of this space was described by Ludwig in 1836. He described a gangrenous infection of the neck with woody cellulitis without suppuration and insidious asphyxiation Cellulitis involving fascial spaces between muscles and other structures of the posterior floor of the mouth that can compromise the airway. Clinical presentation Most patients are young, healthy adults with an odontogenic infection. Usually present with mouth pain, dysphagia, drooling and stiff neck. In the case of Ludwigs angina, massive tongue and floor of mouth edema can rapidly lead to posterior and superior displacement of the tongue as well as anterior displacement out the mouth. The patient often maintains the neck in an extended position and may have a muffled or "hot potato" voice. The neck shows a characteristic erythematous woody swelling but fluctuance is usually absent. Asphyxia The most common cause of death in Ludwigs angina is asphyxia. Airway control is the first priority of treatment, followed by intravenous antibiotics and timely surgical drainage. Tracheotomy is still the most widely used method of airway control but some authors feel the risk of aspiration pneumonia Cricothyroidotomy is usually not a good option with in patients with massive neck edema. Treatment Closely monitor patients with airway compromise and do not allow these patients to leave the acute care area. Sedation and paralytics can relax airway muscles, leading to complete obstruction. Endotracheal intubation is dangerous unless performed under direct visualization. consider fiberoptic intubation or a surgical airway (eg, cricothyroidotomy, tracheotomy Antibiotic therapy Broad-spectrum coverage is indicated. Clindamycin is first-line treatment,initiated alone or in combination with cefoxitin or a beta-lactamase– resistant penicillin, such as ticarcillin/clavulanate, piperacillin/tazobactam, or ampicillin/sulbactam. Patients with cellulitis can be treated with parenteral antibiotics alone. Closely observe these patients for development of an abscess. Surgical Care: Surgical airway control may be necessary in patients whose airways are difficult to visualize or are obstructed completely. Depending on the age of the patient and the experience of the physician, perform needle cricothyroidostomy or cricothyroidotomy only if the child cannot be transported to the operating room safely or quickly. Alternatively perform a tracheotomy. Pharyngeal Pouches Acquired protrusion of mucosa through the muscle layers of the wall of an organ Congenital covered by all the muscle layers of the e.g Meckels diverticulum Pharyngeal pouch three inherent areas of weakness inferior border of the cricopharyngea with the superior oblique fibers of the esophagus. This is referred to as Laimer's triangle. A second inherent weak point is between the oblique and the transverse fibers of the cricopharyngeus muscle: this is referred to as the Killian-Jamieson area, where lateral or Killian-Jamieson diverticula can form. Then, finally, the most significant area is the Killian's triangle, which is formed by the inferior-most fibers of the inferior constrictor muscle with the superior border of the cricopharyngea, and this is thought to be where the Zenker's diverticulum develops. theories One of the primary theories is pharyngoesophageal incoordination , an incoordination between the opening of the cricopharyngeus and the peristaltic contractions propagating the bolus through the hypopharynx. Another theory of the development of Zenker's is that of cricopharyngeal spasm, and that likely in response to stimulation by reflux - the cricopharyngeus muscle simply spasms down. Zenker's diverticulum 1877 .the German pathologist, Zenker, described that traction diverticulum is formed due to external traction on the wall of the digestive tract resulting in the pouch formation, whereas the pulsion diverticulum is formed because of an imbalance of intraluminal force combined with the strength of the digestive tract wall. Foregut diverticula can also be classified based on their anatomic location, one of which is the midesophageal diverticulum, another described as the epiphrenic diverticulum. There are small transitory diverticula which appear throughout the swallowing cycle and then disappear; and then, of course, the hypopharyngeal diverticulum or Zenker's diverticulum. Zenker's It is typically in the seventh and eighth decades. It is predominantly in males . Now the incidence varies depending on the region that you are in. In the United Kingdom, which has the highest incidence, it is about 2:100,000 people per year. Clinical features Commonest symptoms are dysphagia, regurgitation and cough Recurrent aspiration can result in pulmonary complications A carcinoma can develop within the pouch Clinical signs are often absent A cervical lump may be present that gurgles on palpation Zenker's present with dysphagia, between 80% and 90%. regurgitation of undigested food. The combination of regurgitation of undigested food with cervical borborygmi is almost pathognomonic of Zenker's diverticulum. 30 to 40% will present with aspiration and a chronic cough, and up to 15% of these total patients will actually have episodes of aspiration pneumonia diagnostic evaluation consists of primarily the barium swallow, which shows, as in our patient, a posterior pharyngeal diverticulum with pooling of contrast. The swallow can also offer other clues. Treatment Depends on size of pouch and age of patient Options include: Diverticulectomy Dohlman's procedure Diverticulectomy Fascia at anterior border of sternomastoid is divided Pouch is identified anterior to prevertebral fascia Pouch is then excised an defect closed Cricopharyngeal myotomy is performed to prevent recurrence Patient should be feed via a nasogastric tube for a week postoperatively Complications include: Recurrent laryngeal nerve palsy Cervical emphysema Mediastinitis Cutaneous fistula endoscopic diverticulectomy reintroduced in 1960 by Dohlman with no more mortality and only a 7% recurrence rate. In 1993, Collard introduced the next major breakthrough in using the endoscopic GIA staple-assisted diverticulectomy. Other methods that have been used are KTP lasers, CO 2 lasers, and flexible endoscopy with electrocautery. Dohlman's procedure Is an endoscopic procedure A double-lipped oesophagoscope is used Wall between the diverticulum and oesophageal wall is exposed Hypopharyngeal bar divided with diathermy or laser Minimally invasive techniques allow: Shorter duration of anaesthesia More rapid resumption of oral intake Shorter hospital stay Quicker recovery thanks