Imaging of Pediatric Head and Neck Emergencies
advertisement

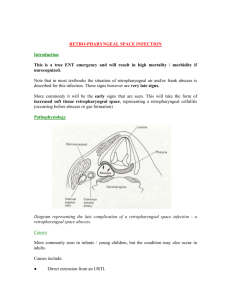
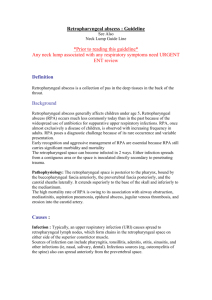
Imaging of Pediatric Head and Neck Emergencies Adam Schneider1, Wilson Altmeyer1, Bundhit Tantiwongkosi1, Yutaka Sato2, Achint K Singh1 1. 2. University of Texas Health Science Center at San Antonio University of Iowa Hospitals and Clinics Disclosure Statement • We have no financial relationships to disclose that may have a direct or indirect interest in the content. Purpose •Detail the spectrum of non-traumatic pediatric head and neck pathologies seen in an emergency room setting and review critical findings that radiologists must convey to clinicians which can directly influence patient treatment and outcomes. Introduction •Head and neck emergencies are less common in the pediatric age group with often non-specific signs and symptoms •Imaging plays an important role in the timely diagnosis of these conditions and is necessary for effective management Table of contents Airway Emergencies Deep Neck Infections Orbital Emergencies Temporal Bone/Ear Emergencies Sinonasal Disease Complications of Neoplasms Home Airway Emergencies Croup Epiglottitis Foreign Body Home Croup (Laryngotracheobronchitis) Frontal radiograph shows straightening of the normally convex subglottic airway with narrowing “steeple sign” Normal “shouldering” of the subglottic airway for comparison Home Croup (Laryngotracheobronchitis) • Clinical: Stridor, barking cough, fever – Peak incidence 6 mo to 3 yr • Etiology: Viral • Imaging – Frontal radiograph: loss of the normal shoulders at subglottic airway with narrowing Frontal radiograph shows straightening of the normally convex subglottic airway with narrowing “steeple sign” • Differentials – Normal epiglottis and prevertebral space helps in excluding epiglottitis and retropharyngeal abscess Epiglottitis Lateral radiograph of the neck demonstrates thickening of the epiglottis (“thumb sign”) and aryepiglottic folds Home Normal epiglottis for comparison Epiglottitis Home • Clinical: Fever, stridor, dysphagia, respiratory distress • Etiology: – Most common pathogen is H. influenzae (decreasing incidence due to vaccination) • Imaging – Lateral radiograph shows enlargement of the epiglottis and aryepiglottic folds Lateral radiograph of the neck demonstrates thickening of the epiglottis (“thumb sign”) and aryepiglottic folds • Differential – Croup: diffuse narrowing of the subglottic airway – Retropharyngeal abscess: widening of the prevertebral soft tissue Foreign body aspiration Home • Clinical: Cough, respiratory distress • Etiology: – Most common at ages 1-3 yr – Typically lodges in the right main stem bronchus Foreign body aspiration Home • Imaging – Majority (80%) of aspirated FB radiolucent -> CXR may appear normal – Air trapping may be seen on expiratory or lateral decubitus views • Differentials – Asthma and viral respiratory tract infections typically result in symmetric lung volumes – Swyer-James syndrome: lucent lung may be smaller – Congenital lobar emphysema: confined to a single lobe Home Foreign Body Aspiration Right lateral decubitus Left lateral decubitus Lateral decubitus chest radiographs of a patient with confirmed right main stem bronchus foreign body demonstrate persistent asymmetric lucency of the right lung consistent with air trapping Home Deep Neck Infections Tonsillar Disease Retropharyngeal Abscess Odontogenic Infection Home Tonsillar Disease • Clinical: Fever, sore throat, dysphagia • Imaging • Tonsillitis: Enlargement and enhancement of the tonsil • Peritonsillar abscess: Rimenhancing fluid collection between the tonsillar pillar and capsule • Differentials • Retropharyngeal abscess: Rim enhancing fluid in the retropharyngeal space • Branchial cleft cyst: typical location in the lateral neck but rare cases of type II may have inner opening in the palatine tonsil Home Peritonsillar Abscess Coronal, sagittal, and axial contrast enhanced CT images show enlargement of the right palatine tonsil with associated rimenhancing fluid collection Home Retropharyngeal Abscess • Clinical: Sudden onset of fever, stiff neck, dysphagia • Imaging – Lateral radiograph: thickening of retropharyngeal soft tissues +/- gas – CT: Rim enhancing fluid collection in retropharyngeal space • Differential – Diagnosis based on location and presence of fluid collection with rim enhancement Axial CT shows fluid/thickening in the retropharyngeal space with small rim-enhancing collection Home Odontogenic Infection • Clinical: Tooth pain, fever, facial swelling, dysphagia • Imaging – Empty socket or lucency about the tooth root with focal cortical break or fistula – Adjacent rim enhancing fluid collection • Differential – Inflammatory changes associated with dental disease is characteristic Home Odontogenic Infection Coronal and axial contrast enhanced CT images show periapical lucency at a right maxillary molar with focal cortical defect communicating with a rim-enhancing abscess and adjacent inflammatory stranding Home Orbital Emergencies Orbital Infections Optic Neuritis Home Orbital Cellulitis • Clinical: Periorbital swelling, erythema, proptosis • Etiology: Most commonly 2° to sinusitis • Complications: • Cavernous sinus thrombosis, meningitis, intracranial abscess • Imaging: Sinus disease, retrobulbar stranding, extraconal fluid collection • Look for non opacification of the cavernous sinus • Imaging plays an important role in the differentiation of preseptal vs postseptal cellulitis Preseptal cellulitis: Limited to soft tissues anterior to orbital septum Post septal cellulitis Home Orbital Abscess with Cavernous Sinus Thrombosis * Contrast enhanced axial CT images demonstrate ethmoid sinusitis, subperiosteal-orbital abscess, and nonopacified cavernous sinus Home Optic Neuritis • Clinical: Eye pain, monocular vision loss, relative afferent pupillary defect (RAPD)and visual field defect • Etiology: MS, sarcoidosis, SLE, syphilis, Lyme dz, viral, etc • Imaging (MR is the modality of choice): • Optic nerve size normal to mildly enlarged with increased signal on T2 and enhancement • Diffusion restriction can be seen (rare) • Differentials • Acute onset makes glioma less likely • Meningioma involves the optic nerve sheath • Sarcoidosis typically involve the lacrimal gland and extraocular muscles with optic nerve Home Optic Neuritis secondary to Lyme Disease T2 DWI T1 post gad MR images (T2, DWI and post gad T1) demonstrate T2 hyperintense signal, diffusion restriction, and enhancement of the right optic nerve Home Temporal Bone/Ear Emergencies Otomastoiditis Acute labrynthitis Otomastoiditis Home • Clinical: Otorrhea, retro-auricular pain, swelling, erythema • Complications: • • • • • Labyrinthitis Facial nerve paralysis Meningitis Dural venous thrombosis Epidural and subperiosteal abscess • Imaging: Fluid opacification of middle ear and mastoid air cells with destruction of mastoid septations • Differentials • Petrous apicitis: Fluid filled petrous apex with surrounding enhancement • Cholesteatoma: Itself does not enhance but can coexist with mastoiditis • Otitis externa has predominant involvement of the EAC Mastoiditis complicated by epidural abscess Home Mastoiditis with Bezold Abscess • Bezold abscess develops when pus erodes the cortex of mastoid bone and extends medial to the attachment of the SCM muscle and spreads along the SCM Fluid opacification of the left middle ear and mastoid air cells with overlying rim-enhancing fluid collection Home Acute Labyrinthitis • Clinical: Sudden onset of hearing loss and/or vertigo • Etiologies: Viral (typically unilateral), bacterial (may be bilateral from meningitis), idiopathic, autoimmune MR axial and coronal post gad T1 images demonstrate enhancement of cochlea, vestibule and lateral semicircular canal Home Acute Labyrinthitis • Imaging: Contrast enhancement of the normally non-enhancing fluid filled spaces of the labyrinth • Differentials • Schwannoma: more focal, intense enhancement • Labyrinthine ossificans: chronic complication of meningitis, shows loss of T2 hyperintensity and ossification rather than enhancement as acute labyrinthitis MR axial and coronal post gad T1 images demonstrate enhancement of cochlea, vestibule and lateral semicircular canal Home Sinonasal Disease Sinusitis and associated complications Sinusitis • Clinical: URI symptoms, nasal discharge, fever • Complications: Orbital cellulitis, osteomyelitis, intracranial abscess, Pott puffy tumor, mucocele • Imaging: Mucosal thickening/enhancement, sinus opacification, air-fluid levels • Look for intracranial and intraorbital extension for early complication detection • Differentials • Allergic fungal sinusitis: Typical appearance is hypointense signal on T2 • Mucocele: expanded sinus Home Home Sinusitis with Epidural Abscess T2 T1 post gad T1 post gad MR images show fluid signal intensity and enhancement in the left maxillary, ethmoid, and frontal sinuses with underlying pachymeningeal enhancement and rim-enhancing epidural abscess along the anterior frontal convexity Home Pott’s Puffy Tumor CT images show fluid opacification of the frontal sinuses with fluid and air containing abscess in the overlying soft tissues. Home Complications of Neoplasms • Neoplasms can result in a variety of secondary complications which may present in the emergency setting • The following cases are illustrative examples including epistaxis, proptosis, and airway compromise Epistaxis: Juvenile Nasopharyngeal Angiofibroma Home • Clinical: Adolescent males, recurrent atraumatic epistaxis, nasal obstruction • Imaging • Avidly enhancing mass centered in SPF • Flow voids can be seen on MR • Classically involves PPF • Osseous erosion nasal cavity, hard palate, pterygoid plates common • Differential • SCC: rare in children • Mucocele: Expanded paranasal sinus • Typical imaging features, age, sex and clinical history make JNA most likely Soft tissue mass involving PPF with associated osseous erosion Home Juvenile Nasopharyngeal Angiofibroma T1 post gad T2 DSA • MR images show an avidly enhancing mass with flow voids centered in the left pterygopalatine fossa extending to the nasopharynx • DSA shows a vascular mass supplied by branches of the ECA Home Proptosis: Bone Metastasis • Clinical: Depends on location, pain, fracture • In children, neuroblastoma and leukemia/lymphoma most common • Imaging: Enhancing mass with aggressive periosteal reaction • Differentials • Fibrous dysplasia: Ground glass, benign appearance • Meningioma: Benign appearance, dense sclerosis • Osteomyelitis: Clinical history and location/association with soft tissue changes may be helpful Axial CT shows aggressive lesion involving the right sphenoid wing/zygoma with “sunburst” periosteal reaction resulting in proptosis Home Neuroblastoma Metastasis Axial CTlesion from involving the same the patient an Axial contrast CT showsenhanced aggressive rightshows sphenoid enhancing left suprarenal mass extending the resulting midline with wing/zygoma with “sunburst” periostealacross reaction in associated vascular encasement proptosis Airway compromise: Venolymphatic Malformation • Clinical: Most present early in life, if large can produce airway compromise • Location: Neck (75%), axilla (25%) • Imaging – Trans-spatial extension – Macrocystic/mixed/microcystic: macrocystic type responds best to sclerosing Rx – Thickened septa contain venous component – Hemorrhage into the cyst forms fluid-fluid levels • Differentials – Thyroglossal duct cyst is usually midline and uncommon at this age – Branchial cleft cyst has cystic contents, different location (depending on the types) and typically seen in young adults – Rhabdomyosarcoma is a reasonable choice but age and fluid-fluid levels argue against it Home Home Venolymphatic Malformation • Frontal radiograph: Soft tissue mass at the left lateral neck with rightward deviation of the trachea • US: Mixed cystic/solid mass with internal vascularity • T2W MR: Large mass with fluid-fluid levels Summary •A wide variety of pediatric head and neck pathologies can present in the emergency room setting •Being familiar with the typical imaging findings of these common entities is important for providing timely and accurate diagnoses References • Donnelly, Lane. Pediatric Imaging: The Fundamentals. Philadelphia: Saunders, 2008. • Ludwig et al. Diagnostic imaging in nontraumatic pediatric head and neck emergencies. Radiographics. 2010 May;30(3):781-99. • Yousem, DM and RI Grossman. Neuroradiology: The Requisites. Philadelphia: Mosby, 2010. • www.statdx.com. THANK YOU FOR VIEWING OUR PRESENTATION Please send questions or comments to: adamjschneider@gmail.com