Russell_Langan_SSAT_readmission_FINAL
advertisement
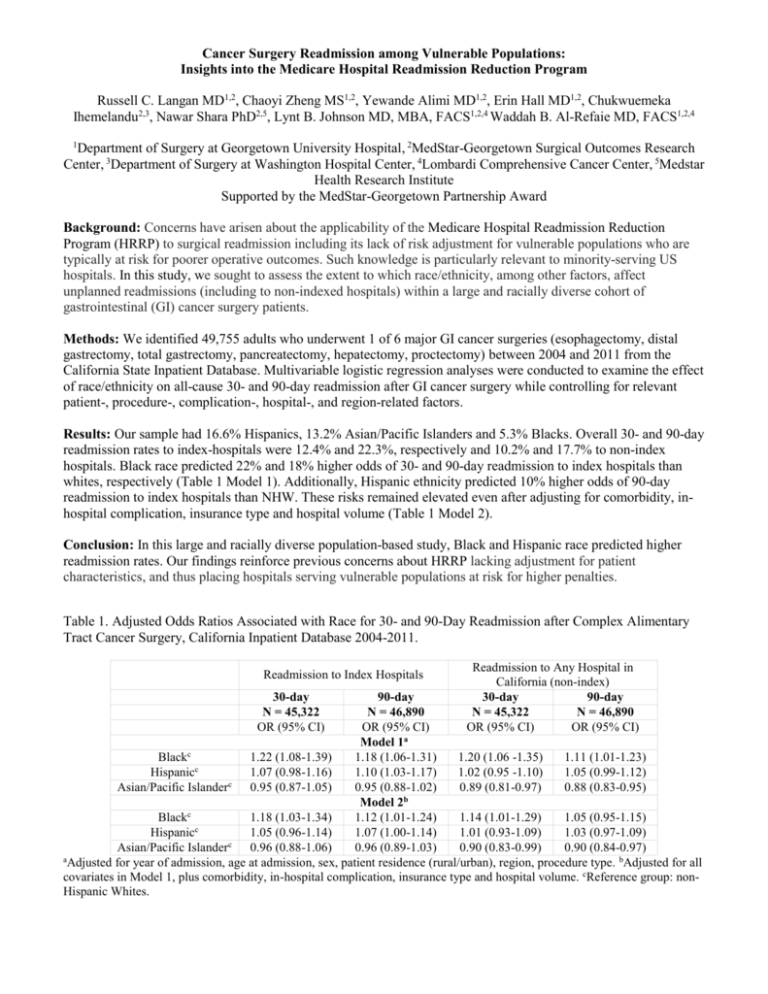
Cancer Surgery Readmission among Vulnerable Populations: Insights into the Medicare Hospital Readmission Reduction Program Russell C. Langan MD1,2, Chaoyi Zheng MS1,2, Yewande Alimi MD1,2, Erin Hall MD1,2, Chukwuemeka Ihemelandu2,3, Nawar Shara PhD2,5, Lynt B. Johnson MD, MBA, FACS1,2,4 Waddah B. Al-Refaie MD, FACS1,2,4 1 Department of Surgery at Georgetown University Hospital, 2MedStar-Georgetown Surgical Outcomes Research Center, 3Department of Surgery at Washington Hospital Center, 4Lombardi Comprehensive Cancer Center, 5Medstar Health Research Institute Supported by the MedStar-Georgetown Partnership Award Background: Concerns have arisen about the applicability of the Medicare Hospital Readmission Reduction Program (HRRP) to surgical readmission including its lack of risk adjustment for vulnerable populations who are typically at risk for poorer operative outcomes. Such knowledge is particularly relevant to minority-serving US hospitals. In this study, we sought to assess the extent to which race/ethnicity, among other factors, affect unplanned readmissions (including to non-indexed hospitals) within a large and racially diverse cohort of gastrointestinal (GI) cancer surgery patients. Methods: We identified 49,755 adults who underwent 1 of 6 major GI cancer surgeries (esophagectomy, distal gastrectomy, total gastrectomy, pancreatectomy, hepatectomy, proctectomy) between 2004 and 2011 from the California State Inpatient Database. Multivariable logistic regression analyses were conducted to examine the effect of race/ethnicity on all-cause 30- and 90-day readmission after GI cancer surgery while controlling for relevant patient-, procedure-, complication-, hospital-, and region-related factors. Results: Our sample had 16.6% Hispanics, 13.2% Asian/Pacific Islanders and 5.3% Blacks. Overall 30- and 90-day readmission rates to index-hospitals were 12.4% and 22.3%, respectively and 10.2% and 17.7% to non-index hospitals. Black race predicted 22% and 18% higher odds of 30- and 90-day readmission to index hospitals than whites, respectively (Table 1 Model 1). Additionally, Hispanic ethnicity predicted 10% higher odds of 90-day readmission to index hospitals than NHW. These risks remained elevated even after adjusting for comorbidity, inhospital complication, insurance type and hospital volume (Table 1 Model 2). Conclusion: In this large and racially diverse population-based study, Black and Hispanic race predicted higher readmission rates. Our findings reinforce previous concerns about HRRP lacking adjustment for patient characteristics, and thus placing hospitals serving vulnerable populations at risk for higher penalties. Table 1. Adjusted Odds Ratios Associated with Race for 30- and 90-Day Readmission after Complex Alimentary Tract Cancer Surgery, California Inpatient Database 2004-2011. Readmission to Index Hospitals 30-day N = 45,322 OR (95% CI) Readmission to Any Hospital in California (non-index) 30-day 90-day N = 45,322 N = 46,890 OR (95% CI) OR (95% CI) 90-day N = 46,890 OR (95% CI) Model 1a Blackc 1.22 (1.08-1.39) 1.18 (1.06-1.31) 1.20 (1.06 -1.35) 1.11 (1.01-1.23) Hispanicc 1.07 (0.98-1.16) 1.10 (1.03-1.17) 1.02 (0.95 -1.10) 1.05 (0.99-1.12) Asian/Pacific Islanderc 0.95 (0.87-1.05) 0.95 (0.88-1.02) 0.89 (0.81-0.97) 0.88 (0.83-0.95) Model 2b Blackc 1.18 (1.03-1.34) 1.12 (1.01-1.24) 1.14 (1.01-1.29) 1.05 (0.95-1.15) Hispanicc 1.05 (0.96-1.14) 1.07 (1.00-1.14) 1.01 (0.93-1.09) 1.03 (0.97-1.09) Asian/Pacific Islanderc 0.96 (0.88-1.06) 0.96 (0.89-1.03) 0.90 (0.83-0.99) 0.90 (0.84-0.97) a Adjusted for year of admission, age at admission, sex, patient residence (rural/urban), region, procedure type. bAdjusted for all covariates in Model 1, plus comorbidity, in-hospital complication, insurance type and hospital volume. cReference group: nonHispanic Whites.