Urine Pregnancy Enzyme Immunoassay Test
advertisement

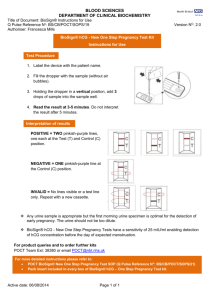
MLAB 1335 Immunology Laboratory Exercise 3 Urine Pregnancy Enzyme Immunoassay Test Objectives 1. Define human chorionic gonadotropin (hCG) and state its function. 2. State the principle of the enzyme immunoassay procedure for the detection of hCG. 3. Differentiate between a qualitative and quantitative assay. 4. State when the urine sample for pregnancy testing should be collected. 5. State the time and temperature for an hCG sample storage. 6. Perform urine pregnancy testing on controls and patient specimens with 100% accuracy. 7. Evaluate reagent package inserts to determine the significance of abnormal results, limitations of the procedure, and troubleshooting procedures when control results are unacceptable. 8. Appropriately record and report results as instructed. 9. State whether the results can be reported to the physician. 10. List 8 conditions, other than pregnancy, for which hCG levels may be ordered. Introduction Human chorionic gonadotropin (hCG) is a glycoprotein hormone secreted by the developing placenta shortly after fertilization. The role of hCG is to prevent the disintegration of the corpus luteum. In normal pregnancy, the hCG hormone can be found in detectable amounts in serum and urine of pregnant women 7-10 days following fertilization. The concentration of hCG doubles every 36 - 48 hours during the early weeks, frequently exceeding 100 mlU/ml by the first missed menstrual period. Human chorionic gonadotropin peaks in the range of 30,000- 200,000 mlU/ml by 10-12 weeks of pregnancy (end of first trimester). During the second and third trimesters, the hCG levels fall to plateau at approximately 1/6 of the peak level. Following delivery, the hCG hormone is rapidly cleared from the blood and pregnancy tests become negative in three to four days. The appearance of hCG in urine soon after conception and its subsequent rise in concentration during early gestational growth provides an excellent marker for the early detection of pregnancy. Principle Modern pregnancy tests use monoclonal antibodies selective for the beta area of the hCG molecule. Most of the urine test systems incorporate monoclonal anti-hCG antibody which after binding with the hCG migrate along a membrane to an area where the molecules become bound to a “fixed” anti-hCG. The fixed anti-hCG is complexed with an enzyme or other color producing molecule. The result will be the production of a visible marker. This type of test is considered a “qualitative” test. The result is either positive or negative. There can be no determination of the amount of hCG present with a qualitative test; it simply indicates the presence or absence of hCG in the sample being tested. There are times when a physician wants a “quantitative” result which is the actual amount of hCG present. This requires a serum sample and an instrument set up to determine the actual concentration of hCG. Quantitative hCG levels assist the physician in determining the actual gestational age of the fetus or may also indicate that this is a multiple pregnancy, i.e., twins, triplets, etc. Specimen Requirements Specimen requirements may be and/or serum and urine. Read the instructions carefully to determine acceptable sample types. All samples must reach room temperature prior to testing. Random urine specimen is appropriate for hCG testing, but the first morning urine is optimal because it generally contains the highest concentration of hCG. Urine specimens should be collected in any clean, dry, plastic container. Refer to the package insert for specific sample storage requirements. When performing a procedure for the first time carefully review the sample storage requirements, length of time for storage, and other manufacturer’s allowable storage requirements. Exercise 3 Pregnancy Test Enzyme Immunoassay Page 1 Revised 10/2014 Quality Control Serum and urine qualitative immunoassay tests have built in controls. The “C” is the internal procedural control and must produce a colored line. It confirms sufficient specimen volume and correct procedural technique. The background of the cassette serves as the negative background control and must remain colorless. If the control line does NOT produce a colored line OR if the white background produces color the test is invalid. When invalid results are obtained the first course of action should be to repeat the test. If another kit is available repeat patient testing on the new kit. If the same invalid result is obtained, discuss with the supervisor. The manufacturer may need to be contacted. It is recommended that external quality control (QC) solutions known to be positive and negative for hCG be evaluated to verify proper test performance. This is a requirement at most facilities which perform pregnancy tests. When kits with new lot numbers are received two devices are used to test with the positive and negative external controls to validate the kit. Facilities which perform large numbers of pregnancy tests will order large volumes of kits with the same lot numbers as this type of quality control only needs to be performed once per lot number. It is crucial that when a new kit is opened that the individual performing the test verify that the QC has been performed. If it has not then the external QC solutions must be tested prior to performing testing on patient samples. Results A positive result usually indicates that a woman is pregnant, but may have had a miscarriage or therapeutic abortion. A confirmed diagnosis of pregnancy should be made by a physician after evaluating all clinical and laboratory findings. False positive and false negative results can occur. A “false positive” is a test result which is positive but the woman is not or has not been recently pregnant. Certain types of tumors or malignancies can produce hCG such as choriocarcinoma, hydatidiform mole, testicular and prostate tumors. The following medications contain hCG and may cause a false positive: Pregnyl, Profasi, Pergonal and APL. These are used in the treatment of infertility. A “false negative” is a test result which is negative but the woman is pregnant. The most common reason for a false negative is that a first morning sample was not used and the amount of hCG is too small to be detected by the test. Technical errors can lead to erroneous results and include: Insufficient sample used Incorrect timing Misinterpretation of the results Clinical Indications While confirmation to diagnose pregnancy is the most common reason a pregnancy test is ordered there are many other conditions which may warrant this test: 1. Suspected choriocarcinoma 2. Suspected hydatidiform mole 3. Suspected molar pregnancy. 4. Testicular tumors 5. Prostatic cancer 6. Breast cancer 7. Lung cancer 8. Pre-surgical procedures 9. Pre-X-ray and radioisotopic procedures Exercise 3 Pregnancy Test Enzyme Immunoassay Page 2 Revised 10/2014 All gestational trophoblastic tumors produce hCG. This hormone is a valuable marker for these tumors. The level correlates with tumor mass and has prognostic value. hCG is extremely sensitive, being elevated in women with minute amounts of tumor. The patient is followed weekly during treatment. At the completion of treatment indefinite follow up is advised to detect recurrence. Quantitative β-hCG levels are used for male patients, along with other tests, to diagnose certain cancers, determine the stage of the cancer, evaluate response to therapy and monitor early detection of relapse. Reference levels in normal pregnancy for a quantitative β-hCG The following is a list of serum β-hCG levels. (LMP is the last menstrual period dated from the first day of the last period.) The levels grow exponentially after conception and implantation. Weeks since LMP mIU/mL 3 5 – 50 4 5 – 426 5 18 – 7,340 6 1,080 – 56,500 7–8 7,650 – 229,000 9 – 12 25,700 – 288,000 13 – 16 13,300 – 254,000 17 – 24 4,060 – 165,400 25 – 40 3,640 – 117,000 Non-pregnant females <5.0 Postmenopausal females <9.5 Exercise 3 Pregnancy Test Enzyme Immunoassay Page 3 Revised 10/2014 Lab (30) SQ (15) Total (45) MLAB 1335 Immunology Laboratory Exercise 3 Urine Pregnancy Enzyme Immunoassay Test Name Date ____________________ Procedure Points ___________/30 Kit Information – USE KIT OR PACKAGE INSERT Test Kit Name Manufacturer Lot Number Expiration Date Storage Temperature Points 1 1 1 1 1 Sample Information Points 1 2 2 Type(s) of samples which may be used. Storage Temperature (list each one) Length of time of storage Refer to the package insert as to the terminology used to report out the results and to answer the following questions. Each of the following items in the chart is worth 2 points (16 total). Points will be deducted for unacceptable correction of errors. Patient Name ID Number Patient Result Positive Control Line Result Background Result 1. 2. Validity of Results Can these results be reported out? Check ONE If “No”, explain: Test Completion Information Initials of individual performing test (Tech) Date of completion Time of completion Exercise 3 Pregnancy Test Enzyme Immunoassay Yes No Point 1 Points 1 1 1 Page 4 Revised 10/2014 MLAB 1335 IMMUNOLOGY/SEROLOGY EXERCISE 3: Urine Pregnancy Enzyme Immunoassay Test Study Questions Name __________________ Date ________ Points _______/15 Refer to the course laboratory materials to answer the following questions. 1. What substance is being detected in the pregnancy test? No abbreviations. (1 point) 2. State the principle of pregnancy tests which use monoclonal antibodies. (2 points) 3. The immunoassay pregnancy test has built in controls. (2 points) a. State the purpose of the “C” area and the expected result. b. 4. State the purpose of the background and the expected result. List and describe two limitations of the procedure. (2 points) a. b. 5. If a refrigerated sample is used, what must be done first prior to performing the test? (2 points) 6. Define “false positive” and give one example. (2 point) 7. Define “false negative” and give one example. (2 point) 8. List 4 conditions other than pregnancy or pregnancy related conditions in which hCG may be detected. (2 points) a. b. c. d. Exercise 3 Pregnancy Test Enzyme Immunoassay Page 5 Revised 10/2014