EARLY PREGNANCY PAIN AND BLEEDING
advertisement
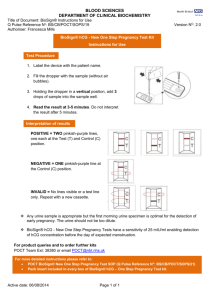
Part 1 Cornerstones of diagnosis are: history and examination hCG transvaginal ultrasound Glycoprotein with and sub-units linked by disulfide bond ( same in all glycoprotein hormones inc. FSH, LH, TSH; subunit confers unique biological activity and specificity in radioimmunoassays) Secreted by syncytiotrophoblast of the chorion Prevents degradation of the corpus luteum (Corpus luteum produces progesterone and some oestrogen which causes the endometrial glands to prepare for implantation of the blastocyst) Initially rises exponentially and after 6 weeks (>6000-10000 mIU/mL) more slowly “Doubling time” useful in first 6 weeks 66% considered to be minimal rise in 48 hours for normal intrauterine pregnancy (85% confidence interval ie. 15% normal pregnancies have less than this rise & 15% ectopics have this rise) Plateauing hCG suggests ectopic Falling hCG - rate important Half life less than 1.4 days – rarely ectopic Half life more than 7 days – most predictive of ectopic Single level – useful only as indication for expected ultrasound findings (depending on quality of ultrasound service) 3-100 x higher than normal pregnancy levels in gestational trophoblastic disease 25-29 days (from LNMP) Intradecidual sac sign (small gestational sac in decidua) (only 50% early pregnancies) Double sac sign (decidua and membranes) 34 days (earliest) Usual 37-38 days Gestational sac (hCG 1000- 36 days (earliest) Usual 42 days Yolk sac 43 days (earliest) Usual 45 days Embryo 43 days (earliest) Usual 45 days Embryonic cardiac activity 1500 = discriminatory zone. 6000 on T/A scan) (CRL >5mm, hCG >25000) Gestational sac >13mm without yolk sac or >17mm without embryo means a non-viable pregnancy Not very useful >25ng/mL – likely viable intra-uterine pregnancy <5 ng/mL – abnormal pregnancy but don’t know if intra- or extrauterine Most between 10 and 20 with early pregnancy bleeding/pain Differential diagnosis: Miscarriage/abortion (intra-uterine pregnancy) Ectopic pregnancy Other – cervical polyps, vaginitis, trauma, foreign body, cervical carcinoma, gestational trophoblastic disease (molar pregnancy) Spontaneous: 20-30% of all known pregnancies (80% in 1st trimester). If pregnancy failure has occurred, usually before 8 weeks Threatened: 30-40% all pregnancies Small PV loss Uterine size =dates Os closed Fetal heart seen or too early to be seen Missed: Uterine size < dates Os closed May not have bleeding at first Fetal pole with no fetal heart Inevitable: Heavy PV loss, usually clots Cervix open Initially no products passed Incomplete: < 6 weeks usually fetus and placental tissue passed together vs >6 weeks Blighted ovum (fertilised but anembryonic) Chromosomal anomalies Embryonic anomalies Uterine anomalies IUD Teratogens (any agent which affects the developing embryo) Mutagens (any agent which changes the DNA of germ cells) Maternal disease Placental abnormalities Trauma History and examination hCG +/- ultrasound (ALWAYS DO A PREGNANCY TEST FOR BLEEDING FEMALE IN REPRODUCTIVE AGE GROUP) ALWAYS THINK ABOUT ECTOPIC ALWAYS CHECK BLOOD GROUP Threatened – observe Missed – suction curettage Inevitable or incomplete – expectant if stable or suction curettage or misoprostil Next week…