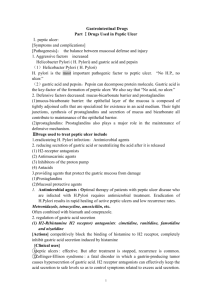
12 Drugs acting on the gastrointestinal tract I: hari minimal 2x 14 peptic ulcer FERD PII " : f. simethicme Anhlsida Antacids NaHCO3 CaCO3 Mg(OH)2 AI(OH)3 R– PROTON PUMP INHIBITORS – M1 H+ H+ ACh Vagus + Ca2+ K+ + H+ Cl– Helicobacter pylori eradication }2H - cimetidine ranitidine Cl– 2 X ' + cAMP Mucus omeprazole lansoprazole I others H2-ANTAGONISTS G Gastrin neutralization RH Acid secretion reducers - Parietal cell H2 ATP TRIPLE THERAPY o . • • . • omeprazole O clarithromycin C A amoxicillin ACh + Mucus cell 0 omeprazole M amoxicillin metronidazole A Mucosal protectants sucralfate bismuth chelate misoprostol M1 Paracrine cell (urease) HCl G Gastrin Coat ulcer base Parietal cells ? Kill H. pylori Gastrin pH 2 pH 7 H+ HCO3– The term peptic ulcer refers to any ulcer in an area in which the mucosa is bathed in the hydrochloric acid and pepsin of gastric juice (i.e. the stomach and upper part of the duodenum). Drugs that are effective in the treatment of peptic ulcer either reduce gastric acid secretion (left centre and right) or increase mucosal resistance to acid–pepsin attack (bottom left). Acid secretion from the parietal cells ( ) is reduced by H2histamine antagonists (right) or by proton pump inhibitors (right), which can produce virtual anacidity by inhibiting the pump ( ) that transports H+ ions out of the parietal cells. Proton pump inhibitors are very effective in promoting ulcer healing, even in patients who are resistant to H2-antagonists. The ‘mucosal protectants’ (bottom left) ). This increase ulcer healing by binding to the ulcer base (left, provides physical protection and allows the secretion of HCO3− to re-establish the pH gradient normally present in the mucus layer ) that originates from mucus-secreting cells ( ). Misoprostol is ( a prostaglandin analogue that promotes ulcer healing by stimulating protective mechanisms in the gastric mucosa and by reducing acid secretion. It is sometimes used to prevent ulcers in patients taking non-steroidal anti-inflammatory drugs (NSAIDs, Chapter 32). 30 + Histamine Cytokines? G-cells Without continuous drug administration, peptic ulcers, however healed, will often recur. This is because chronic infection of the ) is an important aetiological stomach with Helicobacter pylori ( factor in ulcer formation. H. pylori infection is associated with about 95% of duodenal ulcers and 70% of gastric ulcers. The infection may result in a chronic hypergastrinaemia, which stimulates acid production and causes ulcers (bottom right). Uncomplicated peptic ulcers associated with H. pylori infection are treated by the eradication of H. pylori using a combination of a proton pump inhibitor (e.g. omeprazole) with antibiotics (left, centre). Before treatment, infection with H. pylori is confirmed by a urea breath test, in which some [13C]urea is ingested. H. pylori possesses urease, an enzyme that breaks down the urea and produces [13C]carbon dioxide, which can be detected in a sample of breath. The breath test is also used after treatment to verify H. pylori eradication. Antacids (top left) are bases that raise the gastric luminal pH by neutralizing gastric acid (middle left). They provide effective treatment for many dyspepsias and symptomatic relief in peptic ulcer and oesophageal reflux. Many proprietary mixtures, usually containing magnesium or aluminium salts, are available. Medical Pharmacology at a Glance, Seventh Edition. Michael J. Neal. © 2012 John Wiley & Sons, Ltd. Published 2012 by John Wiley & Sons, Ltd. Drugs acting on the gastrointestinal tract II: motility and secretions 13 Drugs used in inflammatory bowel disease Anti-inflammatory drugs Dissolve gallstones Liver BILE ACIDS ursodeoxycholic acid CORTICOSTEROIDS hydrocortisone prednisolone (suppositories, enemas, foam) oral prednisolone Bile duct Gall bladder Gut lumen Aminosalicylates sulfasalazine mesalazine Antispasmodics MUSCARINIC ANTAGONISTS Pancreatic supplements pancreatin Pancreas atropine propantheline dicycloverine Stretch receptor ACh + -0 Bulk Laxatives ACh + bran ispaghula OSMOTIC - MgSO4 lactulose – - FAECAL SOFTENERS (docusate) arachis oil (enema) O ACh Motility stimulants - metoclopramide domperidone = Muscular contractions of the gut and secretion of acid and enzymes are under autonomic control. The enteric part of the autonomic nervous ) with complex intersystem consists of ganglionated plexuses ( connections supplying the smooth muscle, mucosa and blood vessels. ) (parasympathetic) receive extrinsic excitatory The ganglia ( fibres from the vagus and inhibitory sympathetic fibres. Other transmitters in the gut include 5-hydroxytryptamine (5HT), adenosine triphosphate (ATP), nitric oxide and neuropeptide-Y. Cholinomimetic drugs (e.g. neostigmine) increase motility and may cause colic and diarrhoea. They are very occasionally used in the treatment of paralytic ileus (Chapter 8). More useful motility stimulants (bottom middle) facilitate acetylcholine release from the myenteric plexus and are used in the treatment of oesophageal reflux and gastric stasis. Laxatives (bottom left) are drugs used to increase the ) motility of the gut and encourage defaecation. Bulk laxatives ( stimulate stretch receptors in the mucosa. Stimulant laxatives stimulate the myenteric plexus, and some drugs act as lubricants 32 Antimotility drugs Myenteric plexus + STIMULANT senna bisacodyl docusate glycerol suppositories gdiare Submucous plexus BULK ① pwudlmpahl ' ACh Longitudinal muscle Circular muscle Submucosa Mucosa MORPHINE-LIKE AGENTS morphine codeine diphenoxylate loperamide fatal wat damn . Has ). Muscarinic antagonists (top right) reduce gastrointestinal ( motility and are used to reduce spasm in irritable bowel syndrome (antispasmodics). Antidiarrhoeal drugs include antimotility drugs (bottom right), but replacement of water and electrolyte loss is generally more important than drug treatment, especially in infants and in infectious diarrhoea. Anti-inflammatory corticosteroids and aminosalicylates (top left) are used in ulcerative colitis and Crohn’s disease. To reduce the need for systemic steroids, it is usual to add azathioprine, an immunosuppressant (Chapter 43). In the duodenum, bile from the liver (top right) and pancreatic ) enter ( ) usually through juice from the pancreas (right, a common opening that is restricted by the sphincter of Oddi. Bile acids (top middle) are sometimes used to dissolve cholesterol gallstones ( ). Pancreatic supplements (left middle) are given orally when the secretion of pancreatic juice is absent or reduced. Medical Pharmacology at a Glance, Seventh Edition. Michael J. Neal. © 2012 John Wiley & Sons, Ltd. Published 2012 by John Wiley & Sons, Ltd. 30 Drugs used in nausea and vertigo (antiemetics) Cannabinoids nabilone Circulating emetic agents e.g. toxins, opioids, apomorphine Dopamine antagonists prochlorperazine metoclopramide domperidone – Yang } Substance P antagonist + – Ooo aprepitant CTZ (D2, 5HT3 receptors) m - Antimuscarinic drugs - hyoscine EPI : gerda kehumngan dopamine Antihistamines Vomiting centre (M, H, receptors) TRAP - - O 5HT3 antagonists X ondansetron granisetron motion cinnarizine promethazine cyclizine Dimenhydrinate X Irritants e.g. ipecacuanha 5HT – Nausea and vomiting have many causes, including drugs (e.g. cytotoxic agents, opioids, anaesthetics, digoxin), vestibular disease, provocative movement (e.g. seasickness), migraine and pregnancy. Vomiting is much easier to prevent than to stop once it has started. Therefore, if possible, antiemetics should be given well before the emetic stimulus is expected. Antiemetics should not be given before the diagnosis is known because identification of the underlying cause may be delayed. Emesis is coordinated by the vomiting centre ( ) in the medulla (upper figure). An important source of stimulation of the vomiting centre is the chemoreceptor trigger zone (CTZ, ) in the area postrema. Because the CTZ is not protected by the blood–brain barrier (it is part of the circumventricular system), it can be stimulated by circulating toxins or drugs (top). The CTZ possesses many dopamine (D2) receptors, which explains why dopaminergic drugs used in the treatment of Parkinson’s disease frequently cause nausea and vomiting. However, dopamine receptor antagonists are antiemetics (upper left) and are used to reduce nausea and vomiting associated with the administration of emetogenic drugs (e.g. many cytotoxic anticancer agents). 66 The CTZ also possesses 5HT3 receptors, and 5HT3 antagonists (e.g. ondansetron, left lower) are effective antiemetics. Because they have fewer unwanted actions, they are widely used to prevent or reduce the nausea and vomiting associated with cancer chemotherapy and general anaesthesia. In some cases, it is uncertain how 5HT3 antagonists produce their antiemetic effects. There is a high concentration of 5HT3 receptors in the CTZ, but a peripheral action may also be important. Many cytotoxic drugs (and Xrays) cause the release of 5HT from enterochromaffin cells ( ) in the gut, and this activates 5HT3 receptors on vagal sensory fibres ( ) (lower figure). Stimulation of sensory fibres in the stomach by irritants (e.g. ipecacuanha, bacterial toxins) causes ‘reflex’ nausea and vomiting. Dopamine antagonists and 5HT3 antagonists are ineffective in reducing the nausea and vomiting of0 motion sickness. Antimuscarinic drugs or antihistamines (right), which act directly on the vomiting centre, may be effective, although side-effects are common. Vertigo and vomiting associated with vestibular disease are treated with antihistamines (e.g. promethazine, cinnarizine), phenothiazines or betahistine. Medical Pharmacology at a Glance, Seventh Edition. Michael J. Neal. © 2012 John Wiley & Sons, Ltd. Published 2012 by John Wiley & Sons, Ltd.