Anesthesia, cecal ligation and puncture (CLP)
advertisement

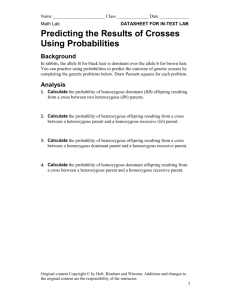
Effect of SOD-1 over-expression on myocardial function during resuscitated murine septic shock Katja Baumgart1,a, Vladislava Simkova1,2,a, Florian Wagner1,a, Sandra Weber1, Michael Georgieff1, Peter Radermacher1, Gerd Albuszies1, Eberhard Barth1 1 Sektion Anästhesiologische Pathophysiologie und Verfahrensentwicklung, 2 Anesteziologicko-resuscitacni klinika, FN u sv. Anny, Brno, Czech Republic, a K.B., V.S. and F.W. equally contributed to this study Institution at which the work was performed: Animal research laboratory of the Department of Anesthesia at the University Medical School Financial support: Supported by the Research Award of European Society of Anaesthesiology 2005 (Eberhard Barth) Financial disclosure: The authors have not disclosed any potential conflicts of interest. Address for correspondence: Peter Radermacher Sektion Anästhesiologische Pathophysiologie und Verfahrensentwicklung Universitätsklinikum Parkstrasse 11 D-89073 Ulm Telephone: 49 731 500 60160 Fax: 49 731 500 60162 e-mail: peter.radermacher@uni-ulm.deAnesthesia, cecal ligation and puncture (CLP) Electronic Supplement Material and Methods: Wild type and both heterozygous and homozygous SOD-1 over-expressing C57BL/6TG(SOD1)3Cje/J mice (Jackson Laboratories, Bar Harbour, ME, age 10–16 wks, body weight 25–33 g) of either gender were randomly allocated to sham operation (controls: wild type: 5 males, 4 females; heterozygous: 6 males, 6 females; homozygous: 4 males, 3 female) and animals rendered septic (wild type: 4 males, 3 females; heterozygous: 5 males, 4 females; homozygous: 4 males, 2 females) [1]). A pressure-conductance catheter was introduced into the carotid artery and advanced into the heart across the aortic valve under the guidance of the online pressure signal in order to assess left heart pressure-volume relationships together with systemic hemodynamics as described in detail previously [2]. The catheter was interfaced with a pressure-volume analog signal amplifier. Real time conductance and pressure data were collected with an analogue-to-digital converter. In brief, changes in the electric field generated by one pair of electrodes during chamber filling and ejection are sensed as a change in voltage in the other pair of sensing electrodes. Due to conductive tissues and fluids surrounding the left ventricular cavity (e.g. the myocardial wall), the measured conductance and therefore the conductance-derived volume differ from the true left ventricular volume. To account for this component of the conductance signal that is not dependent on chamber dimension and “called parallel conductance”, 10 μL of 10 % saline were given i.v. via central venous catheter before the first measuring time point. The highly conductive saline transiently changes the conductivity of the blood, practically without affecting parallel conductance. This change in conductivity allows separation of the left ventricular blood volume from the parallel conductance. In addition to determining parallel conductance, we calibrated and analyzed the measured conductance signals via generating a regression equation for conductance as a function of a defined volume over a range of different hematocrit values using an in vitro volumetric model [3]. This volumetric model contains six cylindrical holes ranging from 13.2 to 172.3 μL, which were filled with fresh heparinized mouse blood diluted with the hydroxyethylstarch solution to obtain the same range of hematocrit values (21 – 38 %) as measured in vivo. The conductance of each cylinder containing the known volume was measured with the conductance catheter at 37°C. From the measured raw conductance signals, the relationship of the known cylinder volumes as a function of the conductance was plotted, and the regression equation for the known volume of the calibrate cuvette V was calculated: The regression equation for the mean hematocrit of 0.29 was V = 4.7·G 19, where G is the measured signal of conductance. Before implantation, a strict setup and calibration procedure of the catheter was performed to prevent influences of ambient conditions such as temperature, composition, and viscosity of surrounding fluids. The catheter was presoaked for 30 min in 37° C warm saline, and immediately before implantation the bridge amplifier was balanced and calibrated using the built-in electronic calibration feature of the Millar control unit [4]. After the surgical instrumentation, a recovery period of one hour was allowed to establish steady-state conditions. Thereafter, the following hemodynamic variables were recorded over a period of 6 hours: heart rate, blood pressure, stroke volume, cardiac output, ejection fraction, left ventricular end-diastolic and –systolic pressure and volume (i.e. the maximum and minimum volumes, respectively [5]), maximal contraction (dp/dtmax) and relaxation (dp/dtmin) as pressure development during isovolumetric contraction and relaxation, τWeiss as an index for left ventricular relaxation [6]. Based on the median of end-systolic and enddiastolic pressure and volume relationships left ventricular pressure volume loops were calculated. Our closed-chest approach, constructing pressure–volume loops based on subsequent made preload-controlled measurements impossible. Consequently, single-beat analyses were used assuming linear end-systolic and end-diastolic pressure-volume relations with a fixed zero-volume and –pressure intercept [7]. To assess myocardial SOD and catalase enzymatic activities, the heart was removed immediately at the end of the observational period, frozen in liquid nitrogen and stored at –70 °C. A 100 mg tissue aliquot was homogenized in 500 μL of chilled sucrose puffer (0.25M Sucrose, 10mM Tris, 1mM EDTA), centrifuged at 13,000 g for 5 minutes, and the SOD and catalase activities were assessed in 100μL supernatant aliquots using commercial kits (SOD Assay Kit – WST, Dojindo Molecular Technologies, Inc., Kumamoto, Japan, with Superoxide Dismutase from bovine erythrocytes, 3K, Sigma as standard and BIOXYTECH® Catalase520TM, Oxis Research, Portland, OR). The enzyme activities are expressed as Umg-1 protein (DC Protein Assay, Bio-Rad Laboratories, Hercules, CA). Statistical analysis All data are presented as median and range unless otherwise stated. After exclusion of normal distribution using the Kolmogorov-Smirnov-test, time-dependent changes within each group were tested using a Friedman ANOVA on ranks for repeated measurements and a subsequent Dunn’s test for multiple comparisons. Differences between groups were analyzed by the Mann-Whitney rank sum test for unpaired samples. In all cases, p<0.05 was regarded as significant. Results: Table 1. Parameters of systemic hemodynamics and left heart function in the sham-operated mice. dP/dtmax maximal systolic contraction, dP/dtmin maximal diastolic relaxation TauWeiss diastolic relaxation time. All data are median, range, # depicts p<0.05 vs. wild type controls, * p<0.05 vs. 18 hours post sham-operation. 18h post laparotomy 21h post laparotomy 24h post laparotomy Heart rate Wild type 396 (341;555) 362 (325;396) 370 (183;554) [min-1] Heterozygous 410 (346;591) 386 (319;478) 392 (322;644) Homozygous 426 (374;543) 408 (359;521) 392 (359;466) Mean arterial Wild type 78 (63;109) 70 (50;83) 63 (51;82) * pressure Heterozygous 83 (65;105) 72 (61;88) 68 (51;77) * [mmHg] Homozygous 84 (73;93) 74 (59;93) 65 (50;68) * Stroke Wild type 21 (12;30) 28 (23;44) 34 (29;47) * volume Heterozygous 23 (12;54) 34 (18;66) 44 (20;60) * [µl] Homozygous 27 (22;34) 37 (22;45) 40 (24;62) * Cardiac Wild type 7.6 (6.8;14.2) 9.7 (7.9;16.3) 12.3 (8.8;21.8) * output Heterozygous 9.6 (4.3;31.7) 13.5 (6.5;25.8) 18.0 (7.1;37.1) * [mL·min-1] Homozygous 14.0 (9.4;16.1) 16.3 (9.4;19.3) 15.4 (9.4;24.5) Enddiastolic Wild type 38 (28;62) 59 (50;91) 89 (78;106) * volume Heterozygous 45 (36;90) 71 (45;110) 108 (70;140) * [µl] Homozygous 63 (45;76) # 78 (69;101) 103 (84;125) * Enddiastolic Wild type 16 (9;18) 17 (10;20) 17 (9;19) pressure Heterozygous 15 (7;24) 16 (7;26) 15 (11;21) [mmHg] Homozygous 14 (8;19) 13 (7;17) 13 (8;18) Endsystolic Wild type 22 (16;33) 32 (24;57) 52 (49;66) * volume Heterozygous 23 (16;57) 34 (26;66) 57 (44;96) * [µl] Homozygous 44 (25;66) # 46 (30;58) 57 (45;87) * Endsystolic Wild type 114 (89;140) 93 (87;109) * 89 (75;107) * pressure Heterozygous 110 (87;132) 93 (73;114) * 92 (79;108) * [mmHg] Homozygous 113 (91;130) 92 (73;110) * 86 (66;102) * Ejection Wild type 48 (44;70) 47 (37;58) 40 (37;49) fraction Heterozygous 56 (32;70) 50 (35;66) 51 (23;60) [%] Homozygous 44 (34;57) 43 (32;60) 41 (29;58) dP/dtmax Wild type 8111 (6942;10437) 7000 (6000;7485) * 6879 (5000;8091) * [mmHg·sec-1] Heterozygous 8315 (5682;10310) 7198 (5363;7709) * 6767 (5360;9624) * Homozygous 8300 (6192;10154) 6655 (5139;7796) * 6001 (4867;8251) * -7000 (-10358;-6304) -6192 (-7358;-5091) -6240 (-7134;-5000) [mmHg·sec-1] Heterozygous -7645 (-9480;-4948) -6001 (-7182;-4836) -5841 (-7821;-4932) Homozygous -7820 (-8705;-5554) -6193 (-7415;-4612) -5617 (-6975;-4373) dP/dtmin Wild type Wild type 6.8 (5.8;7.8) 7.2 (6.0;8.2) 7.2 (4.7;7.7) [msec] Heterozygous 6.8 (5.2;9.3) 6.9 (5.3;10.0) 7.0 (5.2;7.6) Homozygous 5.9 (5.1;8.5) 6.5 (5.9;7.2) 6.8 (6.1;7.4) Table 2. Parameters of systemic hemodynamics and left heart function in the CLP mice. dP/dtmax maximal systolic contraction, dP/dtmin maximal diastolic relaxation TauWeiss diastolic relaxation time. All data are median, range, # depicts p<0.05 vs. wild type controls, * p<0.05 vs. 18 hours post CLP, § p<0.05 vs sham-operated mice. 18h post CLP 21h post CLP 24h post CLP Heart rate Wild type 384 (366;560) 524 (405;584) § 492 (379;560) § [min-1] Heterozygous 445 (369;547) 539 (452;598) § 525 (398;550) § Homozygous 543 (412;558) 498 (410;553) 518 (412;615) § Mean arterial Wild type 72 (62;93) 77 (68;97) 72 (60;88) pressure Heterozygous 72 (50;110) 83 (69;96) 67 (56;84) [mmHg] Homozygous 79 (62;116) 76 (64;91) 68 (65;76) Stroke Wild type 24 (18;31) 30 (18;58) 34 (24;68) * volume Heterozygous 24 (19;33) 37 (21;43) 29 (26;54) * [µl] Homozygous 25 (20;27) 29 (27;34) 38 (30;44) * Cardiac Wild type 9.3 (7.1;17.1) 15.4 (7.6;30.3) 16.7 (8.9;33.1) * output Heterozygous 10.9 (9.2;15.6) 22.0 (9.4;41.8) 14.5 (9.1;29.2) * [mL·min-1] Homozygous 10.1 (9.9;12.0) § 15.0 (11.1;18.4) 21.1 (12.5;23.5) * Enddiastolic Wild type 68 (35;90) 82 (36;115) 100 (58;133)* volume Heterozygous 56 (35;89) 83 (56;126) 104 (70;125)* [µl] Homozygous 66 (53;78) 63 (54;84) 92 (69;110)* Enddiastolic Wild type 18 (8;20) 15 (12;19) 15 (11;18) pressure Heterozygous 12 (9;19) 11 (8;23) 16 (9;22) [mmHg] Homozygous 12 (10;19) 10 (8;13) 13 (7;18) Endsystolic Wild type 43 (26;64) § 58 (43;76) § 73 (43;110)* volume Heterozygous 29 (16;61) 44 (23;75) 71 (41;90)* [µl] Homozygous 29 (20;50) 35 (26;52) 57 (30;72) Endsystolic Wild type 98 (86;108) 103 (90;132) 99 (90;125) pressure Heterozygous 103 (81;145) 111 (100;134) § 105 (97;115) [mmHg] Homozygous 109 (82;116) 110 (84;131) 104 (91;125) § Ejection Wild type 42 (29;64) 40 (31;50) 42 (18;48) fraction Heterozygous 47 (31;57) 49 (22;64) 36 (21;43) [%] Homozygous 45 (35;67) 45 (38;56) 38 (33;57) dP/dtmax Wild type 7622 (7083;8857) [mmHg·sec-1] Heterozygous 7916 (5560;11555) Homozygous 10677 (7000;12895)# § dP/dtmin Wild type -7267 (-8522;6000) [mmHg·sec-1] Heterozygous -7755 (-11443;-5347) Homozygous -9480 (-12401;-6000) Wild type [msec] 8690 (7182;11443) § 8506 (5218;10501) § 10003 (9209;13677) # § 9863 (5277;10581) § 9623 (9432;9975) § 9400 (8857;10000) § -8102 (-11235-;7000) § -7918 (-10549;-5809) § -9676 (-10693;-8398) § -8491 (-9462;-6130) § -8634 (-9640;-7309) § -8000 (-8889;-5905) § 6.3 (5.3;6.8) 5.4 (4.4;5.8) § 5.3 (4.8;6.4) § Heterozygous 5.7 (4.9;6.4) § 4.7 (4.3;5.7) § 5.0 (4.6;7.3) § Homozygous 5.5 (5.1;6.5) 4.6 (4.4;5.4) § 4.8 (4.4;5.4) § References: 1. Simkova V, Baumgart K, Vogt J, Wachter U, Weber S, Gröger M, Speit G, Radermacher P, Albuszies G, Barth E (2008) The effect of superoxide dismutase overexpression on hepatic gluconeogenesis and whole-body glucose oxidation during resuscitated normotensive murine septic shock. Shock epub ahead of print 10.1097/SHK.0b013e31816a6e0f 2. Barth E, Radermacher P, Thiemermann C, Weber S, Georgieff M, Albuszies G (2006) Role of inducible nitric oxide synthase in the reduced responsiveness of the myocardium to catecholamines in a hyperdynamic, murine model of septic shock. Crit Care Med 34:307-313 3. Yang B, Larson DF, Beischel J, Kelly R, Shi J, Watson RR (2001) Validation of conductance catheter system for quantification of murine pressure-volume loops. J Invest Surg 14:341-355 4. Lorenz JN (2002) A practical guide to evaluating cardiovascular, renal, and pulmonary function in mice. Am J Physiol Regul Integr Comp Physiol 282:R1565-R1582 5. Nielsen JM, Kristiansen SB, Ringgaard S, Nielsen TT, Flyvbjerg A, Redington AN, Bøtker HE (2007) Left ventricular volume measurement in mice by conductance catheter: evaluation and optimization of calibration. Am J Physiol Heart Circ Physiol 293:H534-H540 6. Weiss JL, Frederiksen JW, Weisfeldt ML (1976) Hemodynamic determinants of the timecourse of fall in canine left ventricular pressure. J Clin Invest 58:751-760 7. Steendijk P (2006) The role of inducible nitric oxide synthase in the evolution of myocardial (dys)function during resuscitated septic shock: the missing loop. Crit Care Med 34:545-547