Teaching Patient Safety Abstract
advertisement

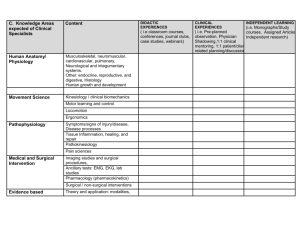
A FRESH LOOK AT HOW TO TEACH PATIENT SAFETY UTILIZING STRUCTURED REVIEW OF MEDICAL ERRORS 1) Ethan Cumbler M.D. Jeffrey J Glasheen M.D. University of Colorado at Denver and Health Sciences Center. Denver, Colorado Background- Educating the next generation of physicians on the elements of patient safety provides a challenge for residency programs. Post-graduate medical education has historically lacked an emphasis on prevention of medical error. The traditional forum for discussion of medical mistakes has been in the morbidity and mortality (M+M) conference. Perhaps due to institutional discomfort of close examination of actual mistakes, it does not appear that error itself is discussed in many M+M conferences. A 2003 study found that only one third of internal medicine M+M conferences involved a true adverse event, and in only 18% did a medical error cause the adverse event. In less than half of the cases involving a medical error was this error discussed, suggesting that traditional internal medicine M+M conferences miss many opportunities to teach residents about medical error. M+M conferences also have a tendency to attribute error exclusively to individual judgment or knowledge failures and not pursue the underlying latent systematic pressures or flaws that are at the heart of a mistake. When errors occur, residents are poorly trained on the appropriate response. One study found that only 50% of housestaff involved in a serious error discussed this error with any colleague, and only 25% had disclosed the error to the patient. Further, 90% of physicians report need for improved education on the management of medical error. Aim- To incorporate a new structured model for analyzing medical error into the housestaff training program that emphasizes the role of systems as well as human psychology and creates an awareness of the factors that predispose to medical misadventures before they begin. Methods- A three module comprehensive approach to medical error education covering systems pressures, latent flaws, and psychological tendencies that predispose to individual mistakes. This is paired with instruction on disclosure of and appropriate response to medical error in the medico-legal context. The program combines each didactic subject with interactive case-based analysis of adverse events using a novel structured form to guide discussion. Results- This program was able to increase resident understanding of the facts of medical error 32% and change physician attitudes about contributions and response to error. After the curriculum, 91% of residents report being more likely to disclose medical error to patients, and 72% report interest in pursuing quality improvement projects. Conclusion- This pilot program demonstrates an effective structure for teaching patient safety via combining short didactic sessions with a structured analysis of medical error.