Case reports
advertisement

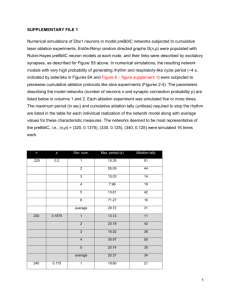
Appendix 2. Case reports Case #5 Reis-Buckler dystrophy and secondary steep central island A 69 year old Asian female presented with a history of poor vision and recurrent corneal erosions since childhood. She was diagnosed as having Reis-Buckler corneal dystrophy (Figure 3). She had a baseline UDVA of 20/100 and CDVA of 20/80 in the right eye, and preoperatively refraction was -0.25 -1.25 x 180. Preoperative Sim-K was 45.8/42.6@001. Preoperative OCT measurement showed that a central ablation depth of 149µm would remove the central superficial stromal opacity. The OCT epithelial thickness was 51.5 µm centrally and 47.8 µm peripherally. The transepithelial laser ablation included 130 µm in PTK mode (6.5mm/0.5mm optical zone/transitional zone diameter), followed by myopic astigmatism ablation of -1.25 -1.25 x 180 (6 x 4.5mm area, 19µm nominal ablation depth). This was followed by a hyperopic astigmatism ablation (to neutralize some of the induced hyperopia) of +6.00 +1.25 x 90, (5.5 x 9.0mm area, 91µm nominal ablation depth). The astigmatism correction was set between the refractive and keratometric magnitude and split between the hyperopic and myopic ablations. Three months postoperatively, right eye CDVA was limited to 20/100 with refraction +0.25 + 4.00 x 145, due to the presence of corneal haze (Figure 4A), and a central island which was detected on the Orbscan axial power map (Figure 4B). Based on Orbscan measurements, the magnitude of the central island was calculated to be 43 µm using the Munnerlyn formula (8.0 D at 4.0 mm diameter). The central island was not directly visible on the OCT pachymetry map (Figure 4C), but its presence was revealed by subtracting the best-fit underlying sphere from the OCT pachymetry map (Figure 4D). Using OCT measurements the central island was 37 µm in magnitude and deviated from the pupil center by 1 mm at 25 degrees (Figure 4D). The epithelial thickness was 22 µm over the apex of the central island and averaged 43 µm along a circle 2.0 mm from the island apex. This indicated that 19 µm of the steep central island was masked by epithelial smoothing – about half as much as the component manifest on the anterior surface (37 µm by OCT and 43 µm by Orbscan). Transepithelial PTK was planned based on the OCT and topography measurements. A 5 mm diameter PTK ablation was set at 43µm to remove the epithelium (epithelial thickness was measured at the edge of the island on the 8 OCT cross-sectional images in the pachymetry scan) and the masked portion of the central island. This was followed by a total of 39 µm of anti-central island ablation, 22 µm at 4 mm diameter (0.5 mm TZ) and 17 µm at 3 mm diameter (0.5 mm TZ) to remove the manifest component of the central island. In order to correspond with the location of the central island, the ablation center was shifted by 1.00 mm at 25 degrees from the pupil center. Four months after repeat PTK treatment the UDVA was 20/50, and CDVA of 20/40 was achieved with a refractive correction of +4.50 +2.00 x 90. Case #6 Granular Dystrophy A 47 year old male presented with history of granular dystrophy. UDVA in the right eye was 20/80 and CDVA was 20/50. Preoperative manifest refraction was -0.75 2.25 x 10. Preoperative Sim-K was 44.8/42.2@008. Simulated ablation based on preoperative OCT imaging showed that an ablation depth of 84µm would remove the superficial layer of corneal opacity centrally (Figure 5). The transepithelial laser ablation included 64 µm in PTK mode (6 mm diameter), followed by myopic astigmatism ablation of -0.80 -2.10 x 10 (6 x 4.5mm area, 20µm nominal central depth). Three months postoperatively, UDVA was 20/50, and CDVA was 20/25, with refraction +0.75 +2.25 x 100.