Supplemental Content - JACC: Clinical Electrophysiology
advertisement

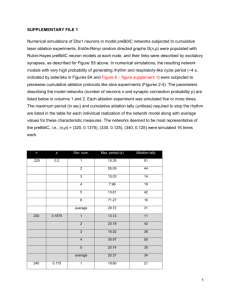
Baldinger et al.; Pulmonary Vein Unexcitability during Isolation Procedures Supplemental Methods Periprocedural management Antiarrhythmic drugs were discontinued ≥5 half-lives prior to ablation, except for amiodarone. All patients received oral anticoagulants for at least 1 month prior to the procedure. Transesophageal echocardiography, when deemed appropriate, was performed within 5 days of the procedure. Vitamin K antagonists were continued uninterrupted; the last dose of novel anticoagulants was given the day before the procedure and resumed the night of the procedure. Mapping and ablation As previously described.1 PVI was performed under general anesthesia and heparin was administered to maintain an activated clotting time of >350 seconds. Intracardiac ultrasound (Cartosound, Biosense-Webster, Diamond Bar, CA, USA) was used for visualizing transseptal punctures and improving catheter contact. A duodecapolar catheter (LiveWire, St Jude Medical, St. Paul, MN, USA) was looped into the coronary sinus (CS) and onto the lateral wall of the right atrium (RA). Deflectable (Agilis, St Jude Medical) and fixedcurve (SR0, St Jude Medical) transseptal vascular sheaths were inserted into the LA using separate transseptal punctures. Using the CARTO 3 (Biosense Webster), electroanatomical mapping system (EAMS) a detailed fast anatomical map was generated for LA anatomy by using a multipolar, multispline diagnostic catheter (Pentaray NAV, Biosense-Webster). A threedimensional model of the LA was used as a reference in 26 of 30 patients, by using the “CARTO-Merge” feature. Electroanatomic points were acquired in all regions of the LA and within PVs. Bipolar voltage was considered abnormal when it measured less than 0.5mV.2 Depth of circumferential normal voltage within the PV-sleeves at baseline was measured using the measuring tool in the EAMS software. Ablation and pacing were performed using a 3.5-mm-tip catheter (ThermoCool SF or ThermoCool SmartTouch, Biosense Webster). RF energy was delivered using a generator (Stockert GmbH, Freiburg, Germany) in a power-controlled mode at 20–30W at an irrigation rate of 17– 30mL/min with the goal of achieving a catheter tip temperature of <45°C. Goals for individual lesions included average contact force >10 grams (25/30 cases) and impedance decrease of 10Ω or greater, except when any esophageal heating occurred as judged by an esophageal temperature probe (Vital-Temp, Vital Signs Inc, Engelwood, CO, USA) at the level of the ablation catheter tip. Additional endpoints of the procedure were electrical isolation of all PVs by antral ablation without carinal lesions, anatomical completion of the RFA-line with less than 5mm gaps between the center of lesion markers, electrical unexcitability of the RFA-line3 and lack of dormant conduction following 12mg of intravenous adenosine.4 Additional ablation at sites of complex fractionated electrograms and application of LA lines was at the discretion of the operator. 1. 2. 3. 4. Michaud GF, John R. Percutaneous pulmonary vein isolation for atrial fibrillation ablation. Circulation. 2011;123:e596-601 Stiles MK, John B, Wong CX, Kuklik P, Brooks AG, Lau DH, Dimitri H, Roberts-Thomson KC, Wilson L, De Sciscio P, Young GD, Sanders P. Paroxysmal lone atrial fibrillation is associated with an abnormal atrial substrate: Characterizing the "second factor". Journal of the American College of Cardiology. 2009;53:1182-1191 Steven D, Sultan A, Reddy V, Luker J, Altenburg M, Hoffmann B, Rostock T, Servatius H, Stevenson WG, Willems S, Michaud GF. Benefit of pulmonary vein isolation guided by loss of pace capture on the ablation line: Results from a prospective 2-center randomized trial. Journal of the American College of Cardiology. 2013;62:44-50 Arentz T, Macle L, Kalusche D, Hocini M, Jais P, Shah D, Haissaguerre M. "Dormant" pulmonary vein conduction revealed by adenosine after ostial radiofrequency catheter ablation. Journal of cardiovascular electrophysiology. 2004;15:1041-1047 Supplemental Figure Supplemental Figure: Theoretical contributions of PV unexcitability to entrance- and exit block A) Both PV sleeves show entrance block and capture with exit block due to a complete antral RFA-line. B) Both PVs show entrance block and capture with exit block despite an incomplete RFA-line. C) one or D) both PV-sleeves unexcitable with incomplete antral RFA-line. + : excitable to pacing; - : unexcitable to pacing