Study Guide for Drugs
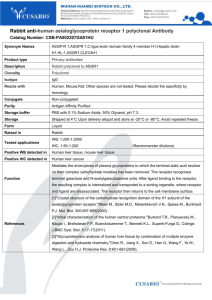
advertisement

Introduction to Pharmacology Listed below are some of the terms you should be familiar with for the exam. The list concentrates on the drugs and drug categories that will be covered on the exam. I have tried to categorize the drugs according to the diseases that they are prescribed for, and which systems the diseases affect. However, many drugs can be prescribed for completely different diseases. For example, many anti-cancer drugs are really antibiotic or antiviral. I have done the best that I can to organize these for you, and where there are clearly more than one use, I have put them in the “other” category. Remember that you will also need to know the names of hormones, neurotransmitters and other compounds in the body that these drugs work on that are not on this list. NEURO DRUGS FOR MOVEMENT DISORDERS Leva-dopa (L-Dopa): commonly used for Parkinson’s disease; a chemically modified form of dopamine that can cross the blood brain barrier where it converts to dopamine then goes to the basal ganglia. L-dopa converts quickly into dopamine prior to entering the brain, so high doses are required for therapeutic effect, may be neuroprotective Carbidopa: when combined with Leva-dopa (combo called Sinamet), it prevents the conversion of L-dopa into dopamine so more L-dopa reaches the brain; allows lower doses of L-dopa and less side effects Sinemet: combination of Leva-dopa and Carbidopa (refer to two drugs); Major side effects include nausea, abnormal muscle tone, tremors, confusion, hallucinations, cardiac arrhythmias, hypotension and dyskinesia (PD) Amantadine: Parkinson’s; usually given with L-Dopa to facilitate release of endogenous dopamine (other drugs like it bromocriptine aka parlodel, pergolide aka permax); side effects include: orthostatic hypotension, depression, hallucinations, nausea, vomiting, confusion and insomnia Selegiline (Deprenyl): antioxidant used for Parkinson’s; inhibit monoamine oxidase, preventing the breakdown of dopamine; limit the level of free radicals in the area, may be neuroprotective Rasagiline: antioxidant used for Parkinson’s disease; approved by FDA in 2008 DRUGS FOR EPILEPSY Barbiturates (ex. phenobarbital): used to treat epilepsy, anxiety, insomnia; bind to the GABA receptor to open chloride channels (decrease neuronal firing); main side effect is sense of sedation and may cause uncoordinated movements; very low therapeutic index; best used for partial and generalized tonic-clonic seizures Phenobarbital: barbiturate prescribed for all seizure types. Primidone is converted into phenobarbital. See barbiturates Benzodiazepine (ex. Diazepam aka Valium, Klonopin): drug of choice for antianxiety drugs (also insomnia, epilepsy); potentiate the effects of GABA; inhibitory drug that hyperpolarizes the neuronal membrane; side effects: sedation, ataxia, behavioral changes; drug dependence; safer than barbiturates; only metabolized in the liver; signs of overdose: sleepiness, confusion, dizziness, loss of memory Dilantin: non-sedative anti-epileptic drug on market; drug interferes with movement of sodium across the membrane (stabilized membrane – lower neuron firing); most effective against partial and generalized tonic clonic seizures; side effects: dizziness, drowsiness, uncoordinated movement, blurred vision, anemia, water retention, cardiac arrhythmias, CHF; bind quickly to albumin; only metabolized in the liver; signs of overdose: sleepiness, confusion, blurred vision, ataxia Carbamazepine: used to treat epilepsy and depression; one of the tricyclic compounds; works through sodium channels and acts on the presynaptic neuron to inhibit synaptic transmission Vigabatrin: designed to enhance the natural effect of GABA; used to treat partial seizures; signs of toxicity: drowsiness, dizziness, weight gain Ethosuximide: used for absence seizures; succinimide drug; acts on the calcium channels and on the sodium-potassium ATPase; side effects: gastric issues, headaches, dizziness, euphoria Valproic acid: free fatty acid that blocks high frequency brain activity; effective with absence and generalized tonic-clonic seizures; side effects: nausea, vomiting, GI complaints DRUGS FOR MULTIPLE SCLEROSIS Betaseron: interferon best prescribed for the early diagnosed person with a form of relapsing-remitting Multiple Sclerosis; molecule thought to inhibit immune system from attacking itself; decreases the number and frequency of exacerbations; injected Novantrone (Mitoxantrone): immunosuppressant approved for relapsing-remitting MS getting progressively worse (secondary-progressive MS); most effective in reducing number of lesion forms on nerves; side effects: heart damage; injected DRUGS FOR ANXIETY Luvox, Praxil, Prozac, Zoloft: drugs prescribed for panic disorders (generalized panic disorder and PTSD); serotonin reuptake inhibitors (block reuptake of serotonin) Prozac, Zoloft: see above; these can also be used as antidepressants in bipolar disorder DRUGS FOR INSOMNIA Ambien: treat insomnia without harsh side effects; nonbenzodiazepine: acts on benzodiazepine receptor (not whole receptor); affect wear off over time Estorra: see Ambien; stays in bloodstream 6-7 hours so it is good when people have difficulty staying asleep Indiplon: nonbenzodiazepine used for insomnia; works fast and does not induce sleepiness during the day ANTI-PSYCHOTIC DRUGS Phenothiazines, Thioxanthenes: 2 of 5 anti-psychotic classifications; block dopamine receptors but are not specific to the limbic system alone; side effects: tardive dyskinesia, pseudo Parkinson’s, akathisia, dyskinesia Haldol (Haloperidol): in a different antipsychotic classification; see above; can treat manic phase of bipolar disorder ANTIDEPRESSANTS Tricyclic Antidepressants: impair the reuptake of amine transmitters back into the presynaptic terminal; neurotransmitter in the synapse longer and overstimulation of the post-synaptic neuron; side effects: sedation, confusion, delirium, tachycardia, dry mouth, urinary retention MAO inhibitors: antidepressants that act on the enzymes that normally degrade amine neurotransmitters and remove it from the synaptic cleft; allows more neurotransmitter to remain; side effects: restlessness, irritability, agitation, insomnia, hypertension DRUGS FOR ALZHEIMER’S DISEASE Aricept, Exelon, Reminyl: these help relieve cognitive symptoms of Alzheimer’s disease; cholinesterase inhibitors prevent breakdown of acetylcholine (important in memory and reasoning); rare side effects: nausea, vomiting, loss of appetite, diarrhea Memantine: treatment for AD; drug is an antagonist of the NMDA receptor on the post-synaptic neuron. Blocks excessive glutamate (which uses NMDA receptor); neuroprotective; moderate to severe AD; side effects: hallucinations, confusion, dizziness and headaches DRUGS FOR BIPOLAR DISORDER Lithium: treatment for bipolar disorder; ion that enters the cell through neuronal sodium channels, but doesn’t have a specific target; may decrease release of amine neurotransmitters, increase their reuptake, or reduce production of another messenger; side effects: metallic taste, resting hand tremor, diarrhea, nausea/vomiting, slurred speech, dizziness, increased muscle tone, confusion Depakote: an anticonvulsant that helps bipolar disorder, specifically the manic phase; side effects: nausea, dizziness, vomiting, stomach pain, rash CARDIOVASCULAR DRUGS ACTING ON THE AUTONOMIC NERVOUS SYSTEM Beta blockers (ex Labetolol (G), Zebeta (T), Cargard (T), Inderal (T)): block the binding of norepinephrine to the beta adrenergic receptors (G protein) of the heart and thus they slow the heart beat and force of contraction (antagonist to block sympathetic activity); this also blocks the G proteins cascade of ionotropic (K+ channels) and chronotropic (Ca+ channels) activation; only metabolized in the liver; signs of overdose: hypotension, slowed HR; treatment: HTN, cardiac arrhythmias; side effects: fatigue, hypotension, excessive slow heart rate and contractility; possible increase in lipid profile and promotion of insulin resistance/glucose intolerance; class II anti-arrhythmia drug Labetalol: see above; has both beta blocking and alpha adrenergic-blocking effects; decreases HR and contractility (beta) and decreases peripheral vascular resistance (alpha) Alpha-1 Blocker (ex. Cardura (T)): binds to and blocks alpha adrenergic receptors of the sympathetic NS, primarily on cells of the vasculature, resulting in increased blood flow and decreased BP; for severe or advanced stages of HTN; positive effect on glucose and lipid metabolism unlike beta blocker; side effects: generalized hypotension, orthostatic hypotension and reflex tachycardia DRUGS THAT ACT DIRECTLY ON HEART AND VASCULAR SMOOTH MUSCLE CELLS Calcium Channel Blockers (ex. Diltiazem (G) aka Cardizem (T), Nicardipine (G), Verapamil (G), Procardia (T)): block the voltage-gated Ca+ channels in smooth muscle cells to allow relaxation of vessels and increase in blood flow, decrease in BP; also blocks Ca in muscle cell so decreases chance of contraction; similar negative iontropic effects to beta-blockers; side effects: swelling in feet/ankles, orthostatic hypotension, headaches, nausea; should be avoided by people with SA or AV abnormalities; can be used for certain cardiac arrhythmias (especially Diltiazem and Verapamil); class IV anti-arrhythmia drugs Sodium Channel Blockers (ex Lidocaine (G) aka Xylocaine (T), Norpace (T), Tambocor (T), Quinidine (G)): first class of drugs used to treat arrhythmias; treat atrial fibrillation or flutter, ventricular tachycardia, paroxysmal supraventricular tachycardia; decrease membrane automaticity, slow impulse conduction through myocardium and prolong refractory period Potassium Channel Blockers (ex. Amidarone (G) aka Cordarone (T)): class III anti-arrhythmia drugs; treat atrial fibrillation or flutter, paroxysmal supraventricular tachycardia and ventricular tachycardia Digitalis (Digoxin (G) aka Lanoxin (T)): drug prescribed for heart failure; increases myocardial contractility by blocking the Na/K pump which drives the Na/Ca exchange so more Ca is brought into the cell and force of contraction is increased; slows HR and normalizes autonomic influence (decrease sympathetic, increase parasympathetic); don’t use in combo with Ca Channel Blockers; low therapeutic index (small margin of safety) so toxicity is common; improves left ventricular performance during exercise (higher ejection fraction and systolic BP) Nitroglycerine: organic nitrate that is used for angina pectoris; it dilates coronary arteries, ameliorates myocardial ischemia, minimizes left ventricular remodeling and reduces mortality in patients with acute MI; decrease myocardial oxygen demand; metabolized into NO which is a vascular smooth muscle relaxant that dilates vessels; sublingual or patches; side effects: headaches, dizziness, orthostatic hypotension; possible tolerance; onset of action 10-45 min lasting 4-6 hours DRUGS FOR THE RENAL SYSTEM Diuretic: can increase the excretion of Na+ and water by the kidneys, producing a decrease in blood volume; decrease in fluid improves dyspnea and alleviates swelling; also reduces resistance in peripheral vessels secondary to vasodilation; treat HTN; potential hypokalemia so take potassium supplements; 3 categories: thiazides, loop diuretic, and K-sparing agents; side effects: fluid and electrolyte imbalance, may effect glucose intolerance and insulin resistance K+-sparing (ex. Aldactone (T)): work at the distal tubule Loop diuretics (ex. Bumex (T), Lasix (T)): work at the thick ascending limb of the Loop of Henle Thiazides (ex. Diuril (T)): work at the distal tubule Angiotensin-converting enzyme (ACE) inhibitors (ex. Lotensin (T), Vasotec (T), Altace (T)): powerful drugs, most preferred for cardiac problems; prevent the conversion of angiotensin I to angiotensin II and increases serum aldosterone levels, results in sodium retention; decreases blood pressure and peripheral resistance; they prevent or may reverse structural changes in large and small vessels throughout the vascular system, leading to improved vascular compliance; can cause allergic reaction (skin rash) or persistent dry cough Avapro (T): like ACE inhibitor but block the receptor that angiotensin II normally would bind; still inhibits vasoconstriction Angiotensinogen: hormone secreted in the liver that converts to angiotensin I Angiotensin I: molecule travels to the lungs where it meets with ACE and converts into Angiotensin II Angiotensin II: powerful constrictor; travels to the kidneys causing water and Na retention and vasoconstriction of vessels Angiotensinogen Angiotensin I Angiotensin II Vasoconstriction of vessel Renin ACE DRUGS ACTING ON BLOOD AND BLOOD PRODUCTS Thrombolytic agents Streptokinase (G), Tissue plasminogen activator (G) aka Activase (T): facilitate breakdown of clots that have been formed; intravenously administered; convert plasminogen to plasmin; side effect: may cause hemorrhage elsewhere; contraindicated for internal bleeding; usually for ischemic stroke, not hemorrhagic; have 3-6 hours to administer before major cell death from ischemia Tissue Plasminogen activator (tPA) (G): see above; first to hit the market from Genetech and reduced mortality of pts having MI; tPA is endogenous to the body, cloned version is activase; Streptokinase (G): see above; bacterial protein (streptococci) not chemically similar to tPA, but same final effect; cost way less than tPA; more adverse reactions with this than tPA Heparin: Anticoagulant that is naturally made in our body by mast cells; heparin works with antithrombin III to inhibit thrombin for clot formation; given parenterally; side effects (dose dependent): prolonged bleeding; Aspirin: see musculoskeletal section; works through the arachidonic pathway to block the works of platelets (responsible for thromboxane A2 production); result is a blood thinner Lipid-lowering drugs Statins (ex. Lipitor (T), Crestor (T), Lovastatin (G), Zocor (T)): inhibit cholesterol biosynthesis in the liver; decrease serum LDL and total triglyceride levels and increase HDL; block Hydroxyl-methylglutayl-coenzyme A reductase (HMG-CoA reductase) enzyme responsible for making cholesterol; used to prevent MI or stroke; contraindications: combo with certain antibiotics, calcium channel blockers and protease inhibitors; side effects: unbalance in liver enzymes, muscle aches Caduet: combination of amlodipine (a calcium channel blocker) and atorvastatin aka Lipitor (HMG CoA reductase inhibitor); reduces LDL and triglycerides in the blood and increase HDL; treat HTN or angina Questran (T): bile acid sequestrant originally designed for obstructive liver disease; drug works in the liver to block resorption of bile and promote excretion of bile acid (conversion of cholesterol to bile acid); also block the HMG CoA reductase activity; little side effect Niaspan (T), Simcor (T): extended release form of niacin (Nicotinic acid, B3 vitamin); commonly used to increase the levels of HDL’s; inhibits the synthesis of precursors for LDL’s; side effects: flushing or itching of skin, vomiting, diarrhea, dry skin, increase plasma glucose MUSCULOSKELETAL ANALGESICS Opiate Drugs: five classes of receptors (mu, kappa, delta, epsilon, sigma) each distributed differently in the body and various affinities; predominately receptors in limbic system; work in CNS and GI tract; side effects: sedation, lethargy, inability to concentrate, mood swings, orthostatic hypotension, cough suppression, decrease respiratory rate; good for moderate to severe pain, constant in nature; used on schedule rather than when feel pain; tolerance and physical dependence can occur Morphine (G): opiate; most common strong agonist; restricted by federal govt because of high rate of abuse Demerol (T): synthetic opioid analgesic; strong agonist; risk for patients with renal impairment, toxic metabolite stays in the body for long periods of time, high levels cause seizures and convulsions. Fentanyl (G): opiate, strong agonist; 100x stronger than morphine; slow acting form; patches or lozenge Codeine (G): chemically modified from morphine; 1/6 as potent as morphine; mild to moderate opiate agonist; body converts it into morphine when administered; Oxycontin (T) aka Oxycodone (G): mild to moderate opiate agonist; frequently abused; oxycontin is slow acting form Percodan: combination of oxycodone and aspirin; mild to moderate opiate agonist; Hydrocodone (G), Darvon (T): other mild to moderate opiate agonists Nalbuphine (G): mixed agonist/antagonist opiate; kappa receptor active/mu receptors inactive; less side effects, do not depress respiration Naloxone (G), Naltrexone (G): these drugs block the effect of opiates; used at antidote for opioid overdose or recover from depressed respiration from opioids Dynorphin: opioid peptide NSAIDS (Non-steroidal anti-inflammatory drugs): common actions: antiinflammatory, anti-pyretic (fever reducer), analgesic, anti-coagulating; should be taken short term; potent inhibiters of enzyme cyclooxygenase which blocks the conversion of arachadonic acid into prostaglandins and thromboxanes; asthmatics shouldn’t take because of broncho-constriction; may increase blood pressure; block bone healing Aspirin (G): acetylsalicylic acid (ASA); most widely used NSAID; inhibits the synthesis of prostaglandins; potent and effective drug; founded by Bayer in 1800’s, traditional headaches and muscle pain; effective for OA and RA; also used for anti-coagulant effects; side effects: gastric issues due to prostaglandin blocking which protects stomach from gastric acid, long term use causes liver toxicity and kidney disorders; children with flu or chicken pox taking this could get Reye’s Syndrome Advil (T) aka Ibuprofen (G) Fenoprofen (G) Naproxen (G) aka Alleve: study showed risk of cardiovascular events Celebrex (T), Vioxx (T): COX-2 inhibitors (class of NSAID) that are specific to COX-2 subtype enzyme; great anti-inflammatory drugs; side effects: abdominal pain, tenderness and discomfort, nausea, blood in vomit, bloody stools, unexplained weight loss/gain, water retention, cardiac events, protect GI tract (unlike aspirin) Vioxx: have a significantly higher change of cardiovascular disease if on the drug; approved for colon cancer Thromboxanes: one of the end products of arachadonic acid that causes platelet aggregation; NSAIDS will block the cellular pathway to inhibit thrombus formation Acetaminophen (G) aka Tylenol: not a NSAID, no anti-inflammatory or anticoagulant effects; no stomach irritation or Reye’s syndrome; may cause liver damage with long term use; absorbed rapidly in upper GI tract, has a half-life of 2 hours LOCAL ANESTHETICS Lidocaine (G) aka Xylocaine (T), Novacaine (T), Benzocaine (G): block the neuronal action potential by blocking the Na+ channel on the neuron causing pain relief; block sensation to particular area; lots of applications ANTI-INFLAMMATORY DRUGS Corticosteroids: common for musculoskeletal problems; drug of choice to reduce inflammatory signals; can be used for MS; side effects: muscle wasting, abdominal adipose tissue, decrease in cognitive function, break-down of muscle, tendon and bone; careful administration to RA and skeletal muscle disease; see endocrine section for more on corticosteroids Leukotrienes: signals inflammatory process SKELETAL MUSCLE RELAXANTS Baclofen: muscle relaxant; binds to GABA-b receptors in the CNS; useful for MS and SCI spasticity; allows better bladder control; has a greater effect when placed in the subarachnoid space (intrathecally: baclofen pump); side effect: weakness, transient drowsiness, orthostatic hypotension, confusion (stroke/elderly) Barbiturates: may reduce muscle spasm or tone; act on GABA receptor; antagonistic effect on postsynaptic receptors, see Neuro section for more Benzodiazepines: increase general CNS inhibition through GABA; low doses of Valium can reduce muscle tone without sedation; see Neuro section Dantrolene: commonly used and only muscle relaxant that acts directly on skeletal muscle; binds to skeletal muscle intracellular calcium release channel, blocking the release of calcium; side effect: muscle weakness, drowsiness, dizziness, fatigue, diarrhea; cleared by liver, so may have some liver damage Tizanidine: used to treat chronic spasticity associate with illness or injury (MS or SCI); no drug dependence; can be used in combo with Dantrolene or baclofen Botulinum Toxin (Botox): impairs the release of acetylcholine at the neuromuscular junction; decreases spasticity if injected into the affected muscle; side effects: food poisoning, irritation at injection site, anti-body production to botulinum toxin; not good long term alternative ENDOCRINE ADRENOCORTICOSTEROIDS: produced by the adrenal cortex Glucocorticoids: involved in control of glucose metabolism; decrease inflammation and suppress immune system; intracellular receptors in cytoplasm then translocated to the nucleus; used as 1.) replacement therapy (Addison’s disease, Cushing’s syndrome), 2.) anti-inflammatory effect (inhibit enzyme phospholipase A which blocks production of leukotrienes and other proinflammatory substances and mediators; arthritis, ulcerative colitis, Crohn’s, systemic lupus, allergic reactions, asthma) and/or 3.) immunosuppression (hypersensitivity to cell-mediated allergic reactions, transplant pts, leukemia, lymphoma, autoimmune hemolytic anemia) Cortisol (aka hydrocortisone): primary glucocorticoid in body; provides negative feedback to hypothalamus and pituitary gland to reduce release of hormone that stimulates cortisol synthesis and release; released in response to stress (fight of flight); when enters mm cell, it decreases glucose uptake and increases protein breakdown; systemically increases blood glucose and liver glycogen Corticosteroids (ex. Prednisone (G), Prednisolone (G), Dexamethasone (G) aka Decadron (T), Kenacort (T): drugs that are synthetic cortisol; no cure, treat symptoms; become active in the liver, so people with liver disease may have trouble using; side effects: no normal production of glucocorticoids (dependent), Cushing’s syndrome, break-down of support tissue (bone, muscle, connective tissue), nervousness and jitteriness Mineralcorticoids: maintain fluid and electrolyte balance; primary one is aldosterone; respond to decrease in BP and works on kidneys (increasing sodium reabsorption); bind cortisol at low affinity THYROID: temp regulation, growth/development, cardio & metabolic effects Drugs for Hyperthyroidism Iodine: will completely stop thyroid hormone production; good short term to decrease feedback mechanism; replaced by beta blockers Iodotope (T): also for thyroid cancer Tapazole (T) Drugs for Hypothyroidism Triostat (T), Synthroid (T): drugs that increase thyroid hormone (synthetic forms of T3 and T4, respectively) PARATHYROID: control calcium concentrations; PTH causes bone breakdown Calcitonin: secreted by cells in the thyroid gland; antagonist to parathyroid hormone (PTH); stimulates bone formation and increases calcium into skeletal storage PANCREAS: endocrine/exocrine; responsible for glucose control Insulin: 51 amino acid peptide that binds to insulin receptor (tyrosine kinase receptor – alpha subunit) and moves glucose into cell; exogenous insulin used for DM Type I; bovine, porcine or human insulin can be used; intramuscular injections; rapid-, intermediate-, and long-acting forms of insulin; common problem is hypoglycemia when too much insulin injected Exubra: inhaled insulin (human form); main problem is dosing (ex. upper respiratory tract infection); may replace injections Oral Hypoglycemic Drugs: for type II DM; induce the release of insulin from pancreas and increase sensitivity of peripheral tissues to insulin; side effects: hypoglycemia, heart burn, nausea, vomiting, diarrhea, headaches, dizziness, skin rashes, leukopenia Diabinese (T), Glucamide (T): peak effect 3-6 hrs; duration 24-48 hrs Glipizide (G): peak 1-3 hrs; duration 12-24 hrs Glyburide (G): peak 4 hrs; duration 24 hrs Metformin (G) aka Glucaphage (T): peak 4-8 hrs; duration 12-24hrs Orinase (T): peak 1-3 hrs; duration 6-12 hrs GPL-1 (glucagon-like peptide 1): hormone in the stomach and intestines that is known to stimulate insulin secretion and decrease glucagon secretion; trying to use this to develop a new drug to improve glycemic control for Type II DM Liraglutide (G): peak 2-13 hrs; duration 24 hrs; mimic GLP1; could cause significant increase in hypoglycemic events Exenatide (G) aka Byetta (T): peak 2 hrs; duration 10 hrs; mimic GLP1; could cause significant increase in hypoglycemic events Sitagliptin (G) aka Januvia (T): peak 1-4 hrs; duration 12.4 hrs; inhibits the enzyme that destroys GLP1; preserve islet mass and increase the average size of islet; increase insulin secretion PULMONARY DRUGS FOR ASHTMA Bronchodilators: can be used for asthma, COPD, infections and other respiratory conditions Albuterol (G): adrenergic bronchodilator; quick acting; for acute asthma; beta agonist used to stimulate respiratory portion of SNS through cAMP (promotes smooth muscle relaxation, inhibits mast cell degranulation through G protein receptor) and cGMP (promotes smooth muscle contraction and enhance mast cell release of histamine); assists in preventing asthma attacks from exercise; too much can increase asthma symptoms; no depression of inflammation; inhaler Formoterol (G), Salbutamol (T): slow acting bronchodilator; also beta agonist (see above); prevent attacks from happening, not for acute asthma; need 12 hours to take effect; no depression of inflammation; inhaler Glucocorticoids (ex. Beclovent (T), Budenoside (G), Cortone (T), Dexamethasone (G), Prednisolone (G), Hydrocortisone (G)): reduce airway inflammation and swelling, decrease chance of asthma attack; preferred long term control mild to mod asthma; inhaler or oral; risk for OP, slow healing wounds, muscle wasting b/c of catabolic effects; side effects: weight gain, fluid retention, high BP, diabetes, cataracts, osteoporosis; see endocrine section Saltropine (T): most common parasympathetic blocker; inhaler; blocks vagus stimulation to prevent bronchoconstriction; body develops tolerance so short term use; side effects: mental depression (low dose), high doses – delirium, hallucination, decreased GI activity Atrovent (T): also parasympathetic blocker, see above, fewer side effects than saltropine (poorly absorbed) Methylxanthine (ex. Theophylline (G)): commonly found in food and beverages; cause reversible airway dilation by inhibiting cAMP and phosphodiesterase; side effects: increased myocardial work load, confusion, irritability, restlessness; low therapeutic range means high toxicity Caffeine (G): a methylxanthine, see above; only metabolized in the liver; signs and symptoms of overdose: nervousness, jitters, anxiety; has intracellular receptors – quickly diffuses through cell membrane without transporter to receptor on endoplasmic reticulum. Cromolyn (G): mediator-release inhibitor family; can be prophylactic for chronic asthma to prevent immediate hypersensitivity or used for acute attacks to reduce severity; used most for persistent mild asthma; prevents influx of Ca into mast cells and blocks release of mediators causing bronchoconstriction; nasal spray; side effects: dry mouth/throat, airway irritation, bronchospasm Singulair (T): blocks the formation of leukotrienes; treat mild, persistent asthma or combo with corticosteroids can treat mod to severe asthma; categorized as an NSAID; side effects: upset stomach, fatigue, dizziness, headache and rash DRUGS FOR ALLERGIES Antihistamines (ex. Benadryl (T, OTC), Claritin (T, OTC), Allegra (T, Rx), Zyrtec (T, Rx): modulate the neural activity within CNS and regulate gastric secretions through H1 an H2 receptors; block H1 (histamine receptor) to decrease mucosal congestion, irritation, and discharge from allergen; also used for asthma; side effects: dizziness, drowsiness, nausea, dry mouth, muscle aches Astelin: antihistamine; prescription nasal spray Decongestants: specifically given to relieve congestion; nasal sprays, syrup, pill, usually OTC, decrease the swelling from inflammation, shrink blood vessels (less leaky); side effects: could increase BP, insomnia, irritability; used in combo with antihistamines Bronchodilators: see above under asthma DRUGS FOR OBSTRUCTIVE LUNG DISEASE Mucinex (T): expectorant used to for mucous obstructions; moving mucous and lubricating internal lining in airway; side effects: minimal/rare, rash, urinary retention, insomnia, hallucinations Antitussives (ex. Tessalon (T)): suppress a cough; all opioids drugs are cough suppressants (neuro section); act on cough center of the brain (CNS effect); any drug with codeine for respiratory problem or infection would be antitussive ONCOLOGY Alkylating Drugs (ex. Cisplatin): largest group of anticancer drug used to treat leukemias, carcinomas, and other neoplasms; induces binding within DNA strands (cause 2 DNA strands to bind so replication and gene expression don’t take place); kills human and cancerous cells; side effects: anemia, leukopenia, thrombocytopenia, GI distress Cisplatin (G): an alkylating drug (see above); primary use for bladder, ovaries and testicles; side effect: pulmonary fibrosis, restrictive lung disease, impaired gas exchange, peripheral neuropathy, loss of strength, fibrosis and hard edema around a joint, cellulitis, neuronal and pulmonary toxicity, bladder irritation Antimetabolitic Drugs (ex. Fluorouracil, Methotrexate, Adrucil); interferes with replication of DNA; metabolites made to be incorporated into DNA making a nonfunctional segment, slow down activity of enzymes involved in DNA replication; side effects: blood disorders, GI distress, skin rash, hair loss, hepatotoxicity, CNS effects Fluorouracil (G) aka Adrucil (T): antimetabolitic drug (see above); primary use colon, rectium, stomach and pancreas Methotrexate (G): antimetabolitic drug (see above); primary use acute lymphoma leukemia, meningeal leukemia, lung, carcinoma of head and neck, NHL; side effect: pulmonary fibrosis, restrictive lung disease, impaired gas exchange, hair loss Antibiotics (ex. Bleomycin, Adriamycin): harsh drugs that are inserted into the DNA strand so DNA replication and gene expression can’t take place; side effect: GI disorders, blood disorders, skin rash, hair loss, hepatotoxicity Bleomycin (G): antibiotic; primary use: carcinoma of head, neck, cervical region, skin, testicle carcinoma, Hodgkin’s disease, NHL; side effect: pulmonary fibrosis, restrictive lung disease, impaired gas exchange Adriamycin (T): antibiotic; primary use: acute leukemia, carcinoma of bladder, breast, ovary, thyroid, Hodgkin’s disease, NHL; side effect: may cause irreversible cardiac damage (cardiac toxicity), hair loss Plant Alkaloids (Vinblastine, Vincristine): nitrogen-based compounds that dissociate microtubules of cells involved in mitosis; cells can’t divide; side effects: blood disorders, GI distress, hair loss, CNS/PNS neuropathies Vinblastine: plant alkaloid; primary use: breast, testes, Hodgkin’s, nonHodgkin’s, Kaposi’s sarcoma; side effects: peripheral neuropathy, loss of strength, fibrosis and hard edema around a joint, cellulitis Vincristine: plant alkaloid; primary use: acute lymphotic leukemia neuroblastoma, Wilm’s tumor, Hodgkin’s, non-Hodgkin’s lymphoma, Ewing’s sarcoma; side effect: peripheral neuropathy, weakness and paresthesia distally, hair loss Mylotarg (T): antibodies to proteins that bind only to cancer cells; CD33 antibody given to treat people with relapsed acute myeloid leukemia IMMUNOLOGY ANTIBACTERIAL AGENTS (ANTIBIOTICS) Penicillin (G): most widely prescribed and effective class of antibiotics because it treats a broad spectrum of infectious agents; Tx gram positive bacteria (streptococci, meningococci, enterococci, group A beta hemolytic and staph infections); administered orally, intramuscularly, intrathecally; few side effects: hypersensitivity to drug, allergic reactions, seizures, epigastric distress, vomiting, colitis, rashes and pain; toxicity: convulsions Amoxicillin: Extended-spectrum Penicillin; commonly used to treat peptic ulcers; prescribed for pneumonia, strep and staph infections, and prevention of rheumatic fever Vancomycin (G): effective with treating gram positive bacteria; drug of choice for severe staph infections or when other antibiotics are ineffective; hinder bacterial cell-wall synthesis; intervention for sepsis or endocarditis caused by methicillinresistant staphylococci; poor GI absorption; administered: capsule, powder form, nasal inhaler or IV; side effects: skin rash, nausea, vomitting; resistance has become major clinical problem; Tetracycline: inhibit bacterial protein synthesis of ribosomes; wide spectrum of activity; inhibit both gram positive and gram negative bacteria (ex. Chlamydiae, mycoplasmas, rickettsiae, protozoa, amebas); administered: tablets, capsules, topical solution, IV; few side effects: nausea, vomiting, diarrhea, sore throat, hoarseness, inflammatory lesions, local venous thrombosis; not for pregnant women or children (deformities); commonly prescribed for peptic ulcers Chloramphenicol: binds to ribosome’s responsible for protein production in bacteria; broad spectrum against aerobic/anaerobic gram positive and negative bacteria; fairly toxic: usually only Rx for rickettsial infection, typhus and Rocky Mountain Spotted Fever; administered: orally; Side effects: GI problems; Toxic to infants: “Gray Baby Syndrome” (grey color, vomiting, flaccidity, and shock) Macrolides (ex. Erythromycin): inhibit protein synthesis; used for diphtheria, erthrasma, genital chlamydia and H influenza; substitute for penicillin; side effects: anorexia, nausea, vomiting and diarrhea, liver toxicity possible Erythromycin: destroyed in stomach acid, given in coated tablet form or IV Aminoglycosides (ex. Gentamycin, Kanamycin, Neomycin): family of drugs that block protein synthesis; rely only on the kidneys for excretion Kanamycin, Neomycin: treat gram negative rods (E Coli, Proteus, Enterobacter Aerogenes, Klebsiella pneumonia); bind onto ribosome subunits and inhibit protein synthesis; administered: capsules, injections; side effects: headaches, confusion, vertigo, hearing loss; toxicity: tinnitus, extreme vertigo, decreased renal clearance, increased BUN Gentamycin: gram negative; treat: Pseudomonas Earuginosa, proteus, E Coli, Klebsiella pneumonia, enterobacter aerogenes; administered: intramuscular or IV; side effects: renal functional impairment; Not for pregnant women Sulfonamides (ex. Sulfadiazine (T)): treat bacterial infections (mostly UTI), diabetes mellitus, edema and gout; inhibit bacterial folic acid synthesis; administered: tablets, oral suspensions, injections; side effects: nausea, vomiting, mental confusion; capable of toxicity: anemia, leukopenia; contraindications: kidney irritation or damage, pregnancy, bone marrow depression Isoniazid: first line of defense to treat active tuberculosis (Mycobacterium tuberculosis) in combo with other agents; tuberculosis difficult to treat because a myobacteria (dont respond to antibacterial agents, replicate slowly, develop drug resistance); preventative tx to people exposed to TB; block synthesis of bacterial cell walls and interfere with cell metabolism; administered: tablets, syrup, injections; side effects: nausea, vomiting, fever, rashes, stomach pain, weakness, loss of appetite, headaches; toxicity: blurred vision, eye pain, diff breathing, seizures; contraindications: liver disease/damage, alcholic ANTIVIRAL AGENTS Acyclovir: inhibits DNA synthesis (doesn’t harm host because it requires a viral protein to activate it, attacks only cells with virus); treat: herpes simplex virus, vericell-zoster virus; administered: oral, IV, topically; side effects: nausea, diarrhea, tolerated well Azidothymidine aka AZT (ex. Epivir): reverse transcriptase inhibitor; first drug designed for HIV (slow rate of progression and prolong survival, viral resistance quickly); administered: IV, oral; strict time regiment; side effects: myelosuppression, GI problems, headaches, myopathies; Indinavir (ex. Ritonavir): inhibitor of protease specific to HIV-1; used in combo with reverse transcriptase inhibitors (more effective with combo); side effects: kidney problems, hyperbilirubinemia, nausea, diarrhea Ritonavir: protease inhibitor; interacts with many drugs (problem); not useful for HIV since on multiple meds Interferon: endogenous proteins (cytokine) inserted into cell membrane after viral infection; block viral entrance into healthy cells (“fools” virus the cell is already infected); artificially administered; success rate not great; Tx: hep B/C, Kaposi’s sarcoma; side effects: GI problems, anemia, weakness, fever ANTIFUNGAL AGENTS Amphotericin: attacks the unique lipids in fungi compromising the stability of the fungus; administered: orally, topically, IV; broad spectrum of antiviral activity: Crytococcus neofomans, candida albican, histoplasma capsulatum, blastomyces dermatitidis; resistance and toxicity likely: renal impairment/failure; side effects IV: fever, headache, vomiting, nausea, muscle spasm Flucytosine: inhibit DNA/RNA synthesis; narrow spectrum: Cryptococcus neofomans, some Candida; rare resistance; typically used in combo with other antifungals; oral admin; side effects: bone marrow toxicity, anemia Azole (ex. Ketoconazoles (G), Diflucan (T)): new category of antifungals that bind to cytochrome P450 enzyme; fight fungal infections on systemic level or topically; broad spectrum (Candida, Blastomycosis, histoplasmosis, Cryptococcus neofomans); Tx amphotericin-resistant fungi; few side effects: minor GI problems DRUGS TO BOOST THE IMMUNE SYSTEM Cytokines (ex. Actimmune, Roferon, Interferon (Betaseron)): endogenous proteins that have regulatory capacities within the immune system; extra amounts can produce severe side effects GASTROINTESTINAL ACID REDUCING DRUGS Antacids (ex. Di-gel, Maalox, Mylanta, Rolaids, Tums): attempt to neutralize excess stomach acid (heart burn or acid reflux); for minor GI discomforts; common side effect is constipation; aluminum containing associated with constipation and magnesium with diarrhea H2 Receptor Antagonists (ex. Tagamet (T), Pepcid AC (T), Zantac (T)): decrease the amount of stomach acid by preventing histamine-activated release of acid under resting conditions and food stimulation; acute and long term care of ulcers; over the counter= peptic ulcers, prescription= reflux disorder; side effects: headaches, dizziness, mild/transient GI complaints Tagamet: more drug interactions if taken in combo, see above Pepcid AC: only Maximum strength Pepcid AC has enough active ingredient to treat/heal peptic ulcers, see above Proton-Pump Inhibitors (PPI) (ex. Prilosec, Prevacid, Nexium): directly act on the proton pump to block hydrogen and the production of acid; 90% more effective than H2 receptor antagonists; can use antibiotics combo (H. pylori can cause peptic ulcers); side effects: headache, diarrhea, constipation, abdominal pain, nausea, rash; typically prescription except Prilosec OTC Gastrozepin (T): most common acetylcholine receptor antagonist for GI problems inhibits gastric secretion at doses below those needed to affect the CNS; relaxes esophageal sphincter; less effective than H2 blockers reducing acid, but good long term healing ulcers; rarely used; side effects: urinary retention, confusion, constipation, dry mouth LAXATIVES: drug of choice when no obstructions in GI tract Citrucel (T) (generic -Methylcellulose): bulk forming lax; absorbs water and swells in lower GI; stretches stimulate peristalsis; side effects: distended, painful abdomen Dulcolax (T), Ex-Lax (T), Senna (G): stimulant lax: these activate peristalsis by unknown means, but thought it increases fluid accumulation in small intestines; side effects: stomach pain, cramping, diarrhea Amitiza (T), Fleets enema (T): hyperosmotic lax; these produce gradients that draw water into the bowel and small intestines=excretion; side effects: stomach pain, gas, cramps Amitiza: see above; frequently used for irritable bowel syndrome, diverticulitis and chronic constipation Colace (T): lubricant and stool softener; brings water into fecal mass and easy elimination; short-term basis for constipation; side effects uncommon: stomach cramp ANTIDIARRHEA AGENTS Kaopectate (T): stool thickener; compound carries pectin which thickens stool, should not be taken more than 2 days since it can kill normal bacteria in GI ANTI-SPASMODIC DRUGS Imodium (T): opiate that produces a general decrease in GI motility; thought to produce local effect on gut wall; slow travel allows water to be removed from stool=firm stool; not taken for more than 3 days; side effects: nausea, abdominal pain, dry mouth, constipation, drowsiness, fatigue, dizziness OTHER Aldosterone: mineralcorticoid responsible for maintaining electrolyte balance; responds to low blood pressure; works in kidneys by increasing sodium reabsorption Antioxidants: ex. Vitamin E, selegiline, rasagiline; control the synthesis of elimination of free radicals (lower the bodies concentration of free radicals); used to treat Parkinson’s (body loses defense against radicals or has increase in production) Calcium channel blockers: bind to voltage-gated calcium channels in arteries (i.e. smooth muscle in coronary arteries); inhibits calcium into cell and the drug blocks the interaction between actin and myosin (contractile elements); the cell is encouraged to relax/increase in diameter, decrease local blood pressure, increase blood flow to that region. Interferon: cytokine thought to inhibit the immune system from attacking itself; antiviral, anticancer, boost immune system Pharmacokinetics: study of the factors that are involved in getting the drug to its target in the body; the mechanisms and regulatory processes that determine how drugs are transported throughout the body comprise the study of pharmacokinetics Pharmacodynamics: the study of the mechanisms of action of the drug, the therapeutic and toxicologic effects, and the chemical structure-activity relationships; the study of what the drug does when it gets to the target molecule