LECTURE 5: GASTROINTESTINAL HORMONES All gastrointestinal
advertisement

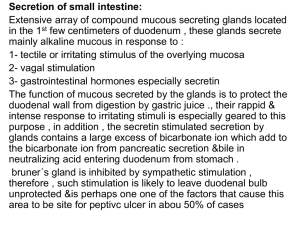
LECTURE 5: GASTROINTESTINAL HORMONES All gastrointestinal hormones are peptides but not all peptides found in the digestive tract mucosa are hormones. Gastrointestinal tract peptides are divided into endocrines, paracrines and neurocrines depending on the method by which the peptide is delivered to its target site. A classical definition of hormones states that they are substances released into the general circulation and which all tissues - particularly the target tissues which contain specific receptors that recognize and bind the hormone. There are four established gastrointestinal cholecystokinin and gastric inhibitory peptide. hormones, namely; gastrin secreting, General Characteristics Four steps are required to establish the existence of gastrointestinal hormone: 1. It must demonstrate a physiological event such that a meal provides the stimulus. 2. The effect must persist after all nervous connections between the two parts of the tracts have been severed. 3. From the site of application of the stimulus, one must isolate a substance that, when injected into the blood, mimics the effect of the stimulus. 4. The substance must be identified chemically and its structure and synthesis must be confirmed. Four gastrointestinal peptides have satisfied their criteria for hormones viz secreting, gastrin, cholecystokinin (CCK) and gastric inhibitory peptide (GIP). Others that are yet to be fully accredited are pancreatic polypeptide, motilin, neurotensin, substance P, vasoactive intestinal peptide (VIP), glucagon and somatostatin. Actions and Interactions Each gastrointestinal hormone has some actions on almost every target test. Even though large doses of a hormone were sometimes necessary to produce an effect, either stimulatory or inhibitory it demonstrated that receptors for each hormone were present on most target tissues. The important actions of the gastrointestinal hormones are those that occur physiologically. 1. Gastrin Gastrin is produced by the G-cells in the lateral walls of the glands found in the antral portion of the gastric mucosa. Apart from this area, a significant amount of gastrin is also secreted by the human duodenal mucosa. Gastrin secreting tumors have been found in the pancreas. These have also been found in the pancreatic islet in fetal life. Three molecular forms of gastrin have been isolated in pure forms. All have the same Cterminal configuration. G-17 - predominant in the tissues. It contains 17 amino acids residues. This increases after feeding. This is the principal form of gastrin with respect to the gastric acid secretion. G-34 - predominant in the blood. It is also called big gastrin. It is not as active as G-17. It is probably a prohormone from which G-17 is derived. G-14 - (mini gastrin) this is less active than G17.It has been isolated from tissues and also from blood. The gastrins occur in 2 biochemical forms viz: sulphated (gastrin II) or non sulphated (gastrin I). When SO3H is present on the tyrosine residue in position 12, the gastrin is said to be sulphated. Both groups are active and are found in the blood and tissue. Gastrins are inactivated primarily in the kidney and small intestine. Actions of Gastrin 1. Stimulation of gastric acid and pepsin secretion (primary action),it is 1,500 times more potent than histamine 2. Stimulation of growth of the gastric mucosa 3. In small doses it causes contraction of the musculature that closes the gastrooesophageal junction 4. It stimulates insulin and glucagon secretion only after a protein meal and not after a carbohydrate meal. 5. It also stimulates calcitonin secretion which in turn appears to inhibit gastrin secretion. 6. It stimulates RNA, protein and DNA synthesis and the growth of exocrine pancreas and mucosa of the small intestine, colon and oxyntic gland area of the stomach. Factors affecting Secretion Secretion is increased by 1. Presence of the product of protein digestion in the stomach particularly amino acids which act on the G-cells. 2. Increased vagal discharge 3. In human, atropine augments the gastrin response to feeding and insulin Secretion is reduced by 1. In dogs by atropine which reduces gastrin released 2. By acid in the antrum. This inhibits gastrin secretion Role of Gastrin in Pathophysiology of duodenal Ulcers In pernicious anaemia in which acid secreting cells are damaged, gastrin secretion is chronically elevated. In achalasia, in which food accumulates in the oesophagus because the gastro oesophageal junction fails to relax, gastrin secretion is elevated. In gastro oesophageal reflux, in which the junction is abnormally relaxed, the gastrin secretion is subnormal. 2. Cholecystokinin (CCK) This is found in the nerves in many parts of the body including distal ileum, colon and the brain. It is secreted in the mucosa of the upper small intestine. Porcine CCK exists in 6 forms with equal activity. These are CCK 58, 39, 33, 12, 8 and 4 (no amino acid residues) Actions 1. 2. 3. 4. 5. 6. 7. 8. 9. Causes contraction of the gall bladder and relaxation of the sphincter of Oddi Causes secretion of a pancreatic juice rich in enzymes Augments the action of secretin in producing secretion of an alkaline pancreatic juice It inhibits gastric emptying It exerts a trophic effect on the pancreas stimulating the growth of the exocrine pancreas. It increases the secretion of enterokinase It enhances the motility of the small intestine and colon Along with secretin, it augments the contraction of the pyloric sphincter thus preventing the reflux of duodenal contents into the stomach It stimulates glycogen secretion Stimulus for release 1. Presence of fatty acids containing more than 10 carbon atoms in the duodenum – increases secretion 2. Amino acids e.g. tryptophan and phenylalanine, Ca++ and H+ increases the secretion. 3. Products of protein and fat digestion. 3. Secretin This is secreted by cells located deep in the glands of the mucosa of the upper portion of the small intestine. The structure is similar to glucagon. Secretin contains 27 amino acids, glucagon contains 29, but 14 amino acids in the two hormones are similar and occupy the same positions in the two hormones. Actions 1. 2. 3. 4. 5. 6. It increases the secretion of bicarbonate by the pancreas and biliary tract It causes secretion of a watery alkaline pancreatic juice It augments the action of CCK in producing pancreatic secretion of digestion enzymes It decreases gastric acid secretion It causes contraction of the pyloric sphincter It increases insulin secretion Stimulus for release 1. Acid bathing the mucosa of the upper small intestine stimulates its release. This is a feed – back action. 2. Protein, carbohydrates and acetylcholine are ineffective. 4. Gastric inhibitory peptide (GIP) This is found in the mucosa of the duodenum and jejunum. It contains 43 amino acid residues; it inhibits gastric secretion and motility. It also stimulates insulin secretion by stimulating the beta cells; its secretion is stimulated by glucose and fats in the duodenum. 5. Vasoactive Intestinal Peptide (VIP) It has been isolated from the nerves in the intestine and recently found in the brain as well. It contains 28 amino-acid residues. It is found also in the blood. Actions 1. It stimulates intestinal secretion of electrolytes and also of water 2. It causes dilatation of peripheral blood vessels and inhibition of gastric acid secretion. 3. It potentiates the action of acetylcholine 6. Enterogastrone This is a putative hormone. It inhibits gastric acid secretion and motility. 7. Motilin This is a polypeptide containing 22 amino acid residues. It has been extracted from the duodenal mucosa. The concentration of motilin in the blood undergoes cyclic fluctuation during fasting. The peak blood levels correspond in the time to the beginning of the activity front of interdigestive myoelectris complex (IMC). It stimulates gastric acid secretion. It also causes contraction of the gall bladder thereby increasing the secretion of bile. It causes contraction of intestinal smooth muscle and it also prepares the intestine for the next meal. 8. Chymodenin This is a polypeptide extracted from the duodenal mucosa. It causes selective increases in the secretion of chymotrypsinogen from the pancreas. Its structure is unknown. 9. Substance p This is found in the neurons in the brain and gastro-intestinal tract. It is not found in circulation. It increases the motility of the small intestine. 10. Bombesin It increases gastrin secretion and the motility of the small intestine and gall bladder 11. Somatostatin It is secreted into circulation by the D-cell in the pancreatic islets and the D-cells in the gastrointestinal mucosa. It is a tetradecapeptide which was originally isolated from the hypothalamus. It exists in 2 forms. It inhibits the secretion of gastrin, VIP, GIP, secretion and motilin. It also inhibits pancreatic exocrine secretion and gastric acid secretion and motility. Secretion is stimulated by acid in the lumen. 12. Glucagon Secretion by –cells in the mucosa of the stomach and duodenum in addition to the -cells in the pancreatic islets, It appears to play a role in the hyperglycaemia of diabetes. The relationship of this gut glucagon – like immunoreactivity (GLI) found in the mucosa of the small intestine is unknown. 13. Gastrin-releasing peptide (GRP) It contains 27 amino acid residues. it is present in vagal nerve ending that terminate on the G-cells its produces vagally increases in gastrin secretion. 14. Neurotensin It has been isolated from the brain and the gut. It increases blood glucose by stimulating glycogenolysis and glucagon release. It also inhibits insulin release. 15. Others Enkephalins and serotonin are also gastrointestinal hormones. They are present in the gland cells and nerve fibres in the gastrointestinal tract. They are also found in the brain.