Physio Chap 66 [10-26
advertisement
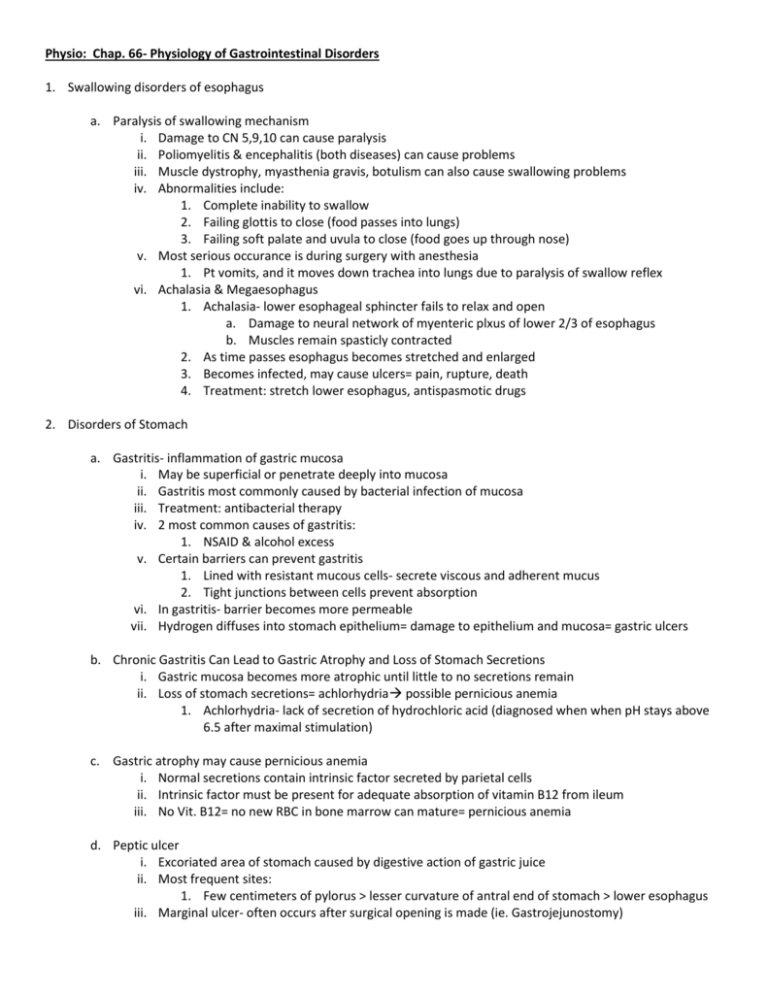
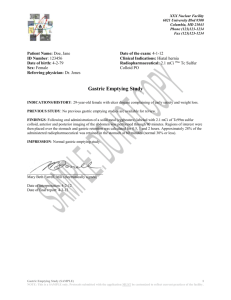
Physio: Chap. 66- Physiology of Gastrointestinal Disorders 1. Swallowing disorders of esophagus a. Paralysis of swallowing mechanism i. Damage to CN 5,9,10 can cause paralysis ii. Poliomyelitis & encephalitis (both diseases) can cause problems iii. Muscle dystrophy, myasthenia gravis, botulism can also cause swallowing problems iv. Abnormalities include: 1. Complete inability to swallow 2. Failing glottis to close (food passes into lungs) 3. Failing soft palate and uvula to close (food goes up through nose) v. Most serious occurance is during surgery with anesthesia 1. Pt vomits, and it moves down trachea into lungs due to paralysis of swallow reflex vi. Achalasia & Megaesophagus 1. Achalasia- lower esophageal sphincter fails to relax and open a. Damage to neural network of myenteric plxus of lower 2/3 of esophagus b. Muscles remain spasticly contracted 2. As time passes esophagus becomes stretched and enlarged 3. Becomes infected, may cause ulcers= pain, rupture, death 4. Treatment: stretch lower esophagus, antispasmotic drugs 2. Disorders of Stomach a. Gastritis- inflammation of gastric mucosa i. May be superficial or penetrate deeply into mucosa ii. Gastritis most commonly caused by bacterial infection of mucosa iii. Treatment: antibacterial therapy iv. 2 most common causes of gastritis: 1. NSAID & alcohol excess v. Certain barriers can prevent gastritis 1. Lined with resistant mucous cells- secrete viscous and adherent mucus 2. Tight junctions between cells prevent absorption vi. In gastritis- barrier becomes more permeable vii. Hydrogen diffuses into stomach epithelium= damage to epithelium and mucosa= gastric ulcers b. Chronic Gastritis Can Lead to Gastric Atrophy and Loss of Stomach Secretions i. Gastric mucosa becomes more atrophic until little to no secretions remain ii. Loss of stomach secretions= achlorhydria possible pernicious anemia 1. Achlorhydria- lack of secretion of hydrochloric acid (diagnosed when when pH stays above 6.5 after maximal stimulation) c. Gastric atrophy may cause pernicious anemia i. Normal secretions contain intrinsic factor secreted by parietal cells ii. Intrinsic factor must be present for adequate absorption of vitamin B12 from ileum iii. No Vit. B12= no new RBC in bone marrow can mature= pernicious anemia d. Peptic ulcer i. Excoriated area of stomach caused by digestive action of gastric juice ii. Most frequent sites: 1. Few centimeters of pylorus > lesser curvature of antral end of stomach > lower esophagus iii. Marginal ulcer- often occurs after surgical opening is made (ie. Gastrojejunostomy) e. Basic cause of Peptic Ulcer i. Imbalance between rate of secretion of gastric juice and degree of protection afforded by: 1. Gastroduodenal mucosal barrier 2. Neutralization of gastric acid by duodenal juices ii. Areas with gastric juice normally covered by mucous coated cells by mucous glands iii. Brunner’s glands in upper duodenum- secrete highly alkaline mucus iv. Duodenum protected by alkalinity of small intestinal secretions (pancreatic secretion) 1. Provides alkalinity for cells= protection from gastric juice 2. Contains lots of sodium bicarb to neutralize HCL, and to inactivate pepsin v. Bicarbonate found in brunners glands and in bile from liver vi. 2 feedback mechanisms to neutralize gastric juices 1. Excess acid in duodenum inhibits gastric secretion and peristalsis in stomach a. = decreases rate of gastric emptying 2. Acid in small intestine liberates secretin which passes to and activates pancreas to empty more pancreatic juice= alkalinity vii. Peptic ulcer caused by 2 ways: 1. Excess secretion of acid and pepsin by gastric mucosa 2. Diminished ability of gastroduodenal mucosa barrier to protect against the juices f. Specific causes of peptic ulcer in human beings i. H. pylori breaks down gastroduodenal mucosal barrier & stimulates gastric acid secretion 1. Eradicated by antibacterial therapy ii. Rate of gastric secretion is greater than normal iii. Smoking- enhances risk (increased nervous stimulation of stomach secretory glands) iv. Alcohol- breaks down mucosal barrier v. Aspririn/NSAIDS- break down barrier g. Treatment of Peptic Ulcer i. Antibiotics- to kill bacteria ii. Acid-supression drugs (ranitidine)- antihistaminic blocks stimulatory effects of histamine 1. = reduced gastric acid secretion 3. Disorders of Small Intestine a. Abnormal digestion of food in SI- pancreatic failure i. Failure of pancreas to secrete juices 1. Occurs frequently in: pancreatitis, pancreatic duct blockage, head of pancreas removed 2. Loss of trypsin, chymotrypsin, carboxypolypeptidase, pancreatic amylase, pancreatic lipase 3. = fat entering SI are not broken down and absorbed; same with carbs, and proteins ii. Pancreatitis- causes: 1. Drinking excess alcohol; blockages of papilla of vater by gallstone 2. Enzymes back up in ducts and then into pancreas= trypsinogen accumulates a. Trypsinogen trypsin which digests parts of pancreas causing damage b. Malabsorption by small intestinal mucosa- Sprue i. Sprue-inadequate absorption of nutrients from Small intestine ii. Nontropical sprue- idiopathic sprue, celiac dz, gluten enteropathy- toxicity to gluten 1. Gluten destroys intestinal enterocytes 2. = blunted/ disappeared villi reducing absorption area of gut iii. Tropical Sprue- in tropics and often treated with antibacterials 1. Caused by inflammation of intestinal mucosa from unidentified infection c. Malabsorption in sprue i. Early stages- fat absorption most affected; fat appears in stool (mostly salts of fatty acids and NOT undigested fats)= steatorrhea- excess fat in stool ii. Impaired protein, carbohydrate, calcium, Vit. K, folic acid, Vit. B12 absorption 1. Persons suffers severe nutritional deficiency= wasting of body 2. Develops osteomalacia (demineralized bone from lack of calcium) 3. Develops inadequate blood coagulation from lack of Vit. K 4. Develops macrocytic anemia (pernicious anemia)- diminished Vit. B12 and folic acid absorp. 4. Disorders of Large Intestine a. Constipation i. Slow movement of feces through large intestine (hard, dry, lg quantity of feces in descending colon) ii. Frequent cause: irregular bowel habits over lifetime iii. Infants normally not constipated- with age they learn to control defecation and this causes problem iv. If you don’t allow defecation when needed or if use lots of laxatives: 1. = reflexes become weak; colon becomes atonic (lack muscle tone) v. Constipation can also come from sigmoid colon spasm 1. Feces accumulates above spasm; then diarrhea occurs, and cycle repeats vi. Megacolon (Hirschprung’s Dz) 1. Bowel movements only every several days to once per week 2. Colon enlarges and becomes distended (due to increased fecal matter content) 3. Frequent cause of megacolon: a. Deficiency of ganglion cells in myenteric plexus in segment of sigmoid colon b. = lack defecation reflex or peristaltic motility b. Diarrhea i. Rapid movement of fecal matter through large intestine ii. Enteritis- Inflammation of intestinal tract 1. Usually caused by virus or bacteria 2. Infectious diarrhea usually in large intestine & distal ileum 3. Secretion is enhanced-more fluid to flush out pathogen iii. Cholera- toxin stimulates excessive secretion of electrolytes and fluid- can cause death 1. Therapy replace fluids and electrolytes as fast as possible (best given by IV) iv. Psychogenic diarrhea- diarrhea accompanies nervous tension or emotional stress 1. Excessive stimulation of parasympathetic nervous system excites motility and excess mucous secretion v. Ulcerative Colitis 1. Walls of Large Intestine become inflamed and ulcerated (often pts with diarrhea) 2. Cause is unknown- heredity is suspected 3. Once progressed too far ileostomy is usually performed vi. Paralysis of Defecation in spinal cord injuries 1. Accumulated feces triggers spinal cord-mediated defecation reflex from rectum to conus medullaris of spinal cord 2. Injury between conus medullaris and brain- voluntary defecation is blocked a. = loss if voluntary aid with defecation= difficult to defecate b. Small enema usually helps in mornings shortly after meal 5. General Disorders of GI tract a. Vomiting- upper GI rids self of contents i. Excessive irritation, distention can cause vomiting ii. “vomiting center”- in brain stem (vagal/ sympathetic afferents) iii. Motor impulses are transmitted from vomiting center by CN V, VII, IX, X, XII iv. Antiperistalsis occurs prior to vomiting (peristalsis moves up GI tract instead of down it) v. Distention occurs causing excitement of nervous system vi. Vomiting initiated by strong contractions of duodenum and stomach; relaxation of esoph-stomach sphincter vii. Abdominal muscles expel vomit b. Vomiting act i. Deep breath ii. Raising hyoid bone and larynx to pull upper esophageal sphincter open iii. Closing of glottis (prevent vomit into lungs) iv. Lifting soft palate to close nose v. Downward contraction of diaphragm + abdominal muscle contraction vi. Pressure builds- sphincter relaxes= expulsion occurs c. Chemoreceptor trigger zone in brain medulla for initiation of vomiting by drugs or by motion sickness i. – certain drugs can initiate vomiting response 1. Apomorphine, morphine, digitalis- stimulate chemoreceptor trigger zone ii. Rapidly changing directions from vestibular labyrinth of inner ear can cause similar effects d. Nausea i. Prodrome of vomiting- conscious recognition of excitation in area of medulla (vomiting center) ii. Caused by: 1. irritative impulses from GI tract 2. impulses originating from lower brain associated with motion sickness 3. impulses from cerebral cortex to initiate vomiting e. GI obstruction i. Can be from: 1. Cancer 2. Fibrotic constriction resulting from ulceration or from peritoneal adhesions 3. Spasm of segment of gut 4. Paralysis of segment of gut ii. Can occur in different parts of GI tract and cause different effects: 1. Pylorus (often from fibrosis from ulcer repair)= acid vomiting a. =reduced body nutrients b. = reduced acid contents from stomach= whole-body metabolic alkalosis 2. Obstruction below duodenum= neutral or basic vomitus a. = loss of water and electrolytes= dehydration b. Little change in acid-base balance 3. Obstruction in small intestine= extreme vomiting= dehydration 4. Lower obstruction of Large intestine= extreme constipation with less vomiting f. Gases in GI tract (flatus) i. Flatus enters GI tract usually from 3 sources: 1. Swallowed air a. Usually found in stomach- expelled by belching 2. Gasses formed in gut as result of bacterial action a. Usually forms CO2, methane, and hydrogen 3. Gases that diffuse from blood into GI tract ii. Certain foods cause more flatus: 1. Beans, cabbage, onion, cauliflower, corn, vinegar iii. Amount of gases entering or forming in large intestine: 1. 7-10L/day iv. Amount of gases expelled: 1. 0.6L/day 2. Remainder is normally absorbed into blood and expelled from lungs