Microbiology 63 [5-11

Microbiology 63: Urinary Tract Infections
Most common bacterial infection in humans
UTI -> can occur at any site in urinary tract (usually bladder, kindey, prostate)
Urethritis caused by Neisseria gonorrhea and Chlamydia pneumoniae
Acute uncomplicated UTI = acute cystitis in healthy women
Acute nonobstructive pyelonephritis = kidney infection in healthy women
Complicated UTI = underlying structural or functional abnormality
Asymptomatic bacteriuria = bacteria in urine without symptoms
Bacterial prostatitis = bacterial infection of prostate
Acute bacterial prostatitis = severe infection, acute onset
Chronic bacterial prostatitis = persistence of bacteria in prostate
Renal abscess = can occur with severe pyelonephritis or bacterial spread
Recurrent infection = reinfection or relapse
Pathogenesis
Infecting organisms -> from normal gut flora ascending up the urinary tract, turbulent flow in men with prostate hypertrophy, or bloodstream from other site (multiple cortical abscesses) o S. aureus and Candida common with hematogenous spread
Most important uropathogen = Escherichia coli
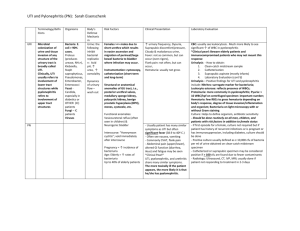
Acute Uncomplicated UTI = E. coli with mannose-sensitive fimbria (FimH) -> adherence to urothelial cells o Staphylococcus saprophyticus (Gram +) in 5-15% of -> temporal variation (autumn) o E. coli in 90% of acute nonobstructive pyelonephritis from P fimbriae (adhesion) bind to
glycosphingolipid Gal(α1-4) Galβ disaccharide
Aerobactin (iron scavenger) and hemolysin (lyse host cells) -> virulence factors on pathogenicity islands on E. coli chromosome
Complicated UTI = E. coli most common pathogen, lower virulence factors than above (host principal determinant of infection) o Enterobacteriacease family (Klebsiella, Enterobacter, Citrobacter), nonfermenting Gram neg. organisms (Pseudomonas aeruginosa), urease-producers (Proteus mirabilis,
Morganella morganii and Provendencia -> metabolize urea to ammonia for further damage) o Enterococcus species and coag neg staph are most common Gram + o Candida alibans, C. tropicalis, C. glabrate, C. parapsilosis (occasionally) o Many have indwelling urologic devices (catheter, stent, or nephrostomy tube)
Biofilm has microorganisms
Asymptomatic Bacteriuria = E. coli in healthy women, low virulence factors
Bacterial Prostatitis = S. aureus or E. coli, prevalence of virulence factors, prostate stones source of bacteria
Host Factors
Uncomplicated UTI = normal voiding, genetic predisposition through nonsecretor of ABH blood
group antigens (bind to bacteria preventing attachment) or behavioral risk with sexual
intercourse and spermicide use for birth control, or estrogen deficiency o Lactobacillus flora in vagina maintains acidity but spermicide kills normal flora o New sexual partner, diaphragm use, and antimicrobial therapy also increase risk
Complicated UTI = structural or functional abnormalities (reflux, stones, pregnancy or catheters)
Host response
Acute cystitis = inflammatory response with local cytokine production (IL6, IL8, IL10), IgA and
IgG antibody response o Local immunity from acute cystitis does not protect from subsequent episodes
Acute uncomplicated pyelonephritis = pyuria, cytokine production, fever, leukocytosis, elevated
CRP, IgM (first infection) and IgG (subsequent infection)
Spontaneous resolution less frequent in complicated UTI
Gram + (Enterococcus) and coag neg staph less often accompanied by pyuria
Clinical presentation
Uncomplicated cystitis or pyelonephritis = dysuria, frequency, urgency, suprapubic or low-back discomfort, some hematuria o Physical exam normal in acute cystitis by CVA pain and tenderness in pyelonephritis
(fever, nausea, vomiting)
Complicated UTI = symptoms of acute cystitis/pyelonephritis
Bacterial Prostatitis = high fever, pelvic pain, urinary retention, swollen tender prostate (digital exam not recommended), if chronic-> recurrent episodes of acute cystitis
Urine Culture
Contamination from periurethral area or vagina -> false positive o Clean-catch specimen mid-void is adequate
Colony counts of contaminants in voided specimens are low, while infecting organisms
achieve high concentrations o Prompt forward to lab o Most have 1 organism but complicated UTI may have more
Biofilm-coated devices -> greater number and higher count of organizms o Use new catheter for urine collection to avoid biofilm organisms
Any quantitative count of potential uropathogen is consistent with UTI for women with acute
uncomplicated UTI o In pyelonephritis or complicated UTI -> at least 10 5 CFU/mL of pathogen o Asymptomatic bacteriuria IDed with 2 consecutive urine specimens w/ > 10 5 count
H. influenzae and Ureaplasma urealyticum infrequently cuase and not isolated with lab methods
Other Lab Tests
Pyuria -> dipstick leukocyte esterase test (not specific for UTI)
Systemic manifestations require blood culture obtained
Treatment
Antimicrobials excreted in urine preferred (achieve high urinary levels)
Acute uncomplicated cystitis = treat empirically, antimicrobial short-course (3-day) therapy o Trimethoprim/sulfamethoxazole (TMP/SMX) or trimethoprim = first choice drugs o Second choice = fluoroquinolone (3 days) or nitrofurantoin (7 days) o If pregnant, use cephalosporins o Fosfomycin trometamol (single does) not as effective
Acute uncomplicated pyelonephritis = urine culture pretherapy, leukocyte count and blood/urine cultures o Oral therapy = TMP/SMX, TMP, or fluoroquinolone o Parenteral therapy = extended spectrum cephalosporin, aminoglycoside, or fluroquiniolone (10-14 days)
Complicated UTI = urine culture pretherapy, if sever may need hospitalization and initial parenteral therapy
Asymptomatic bacteriuria = common in nursing homes, mostly don’t treat (unless pregnant or need procedure with potential trauma) o If in pregnancy, may risk pyelonephritis later (end of 2 nd or early 3 rd trimester)
Recurrent UTI = management of pt instead of treat individual episode (prolonged antimicrobial therapy)
Acute Uncomplicated UTI = if 2 episodes every 6 months or 3 every year, prophylactic therapy
(long-term low-dose therapy) o TMP-SMX, TMP, and fluoroquinolones reduce Gram – flora o Nirtofurantoin effective but no impact on flora (intermittent urine sterilization)
Complicated UTI = suppressive therapy with recurrent infection and urologic abnormalities