Manual Service Authorization Form
advertisement

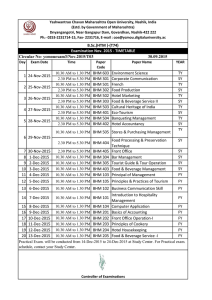
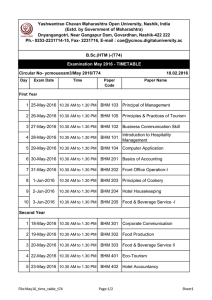
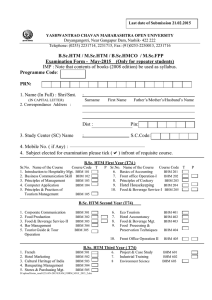
Manual SAR Process Partners Behavioral Health Management (Partners BHM) will post a paper Service Authorization Request (SAR) on the website. This form is to be used for the following situations: The Alpha MCS system is not available and is not expected to be available for an extended period of time. For example; 8 hours or more; this information will be communicated via the Partners BHM website. The Provider is an out-of network and/or out-of-area provider who is serving a Partners BHM consumer who either requires specialty treatment not available in the network, is out of the catchment area when a crisis occurs, or lives in another catchment area but Medicaid is not expected to change. For example, consumers who are living in residential situations outside of the Partners BHM catchment area, but continue to have Medicaid from one of Partners BHM counties A service is being requested that is not in the Partners BHM Benefit Plan and is not an available drop-down option for services in the Alpha MCS system. For example, an EPSDT Medicaid request for a service not included in the Partners BHM Medicaid Benefit Plan. The Manual SAR Form: Provider: Complete Provider name, address and the site number where the consumer will receive services. Also list the Provider’s NPI#. A Provider Identification number will be assigned by Partners BHM when the Consumer Specific Agreement application has been reviewed and approved. Consumer: List the demographic information to identify the consumer. The out-of-area/out-of-network policy applies only to Medicaid consumers. Call Customer Services (ACCESS) @ 1-888-235-4673 to obtain a consumer Identification number, if you do not have a log-in to the Partners BHM Alpha MCS system. Consumer information includes the social security number, Medicaid Identification Number, Date-of Birth, address, guardian name and relationship to the consumer, type of request, urgency of request, disability of consumer, voluntary/involuntary status of consumer, and Level of Care Assessment using the LOCUS/CALOCUS, ASAM or NC-SNAP/SIS. Diagnosis: List the consumer’s DSM-5 diagnoses. Substance Use: List any substance use including; name of the substance, age of first use, frequency, amount and route for each substance. Revised 2/18/2015 Medical: Verify that consumer has a medical home and that a release of information has been signed between the provider and primary care physician. Provide a list all medications and the dosage, regimen and # of monthly doses. Supporting Documents: Use the website to determine the documents required for the service(s) requested. Provide, when applicable, the Inpatient Review Form, Comprehensive Clinical Assessment or Intake Evaluation, Psychological/psychiatric evaluations, PCP or basic treatment plan, school information and any other documents that might support the request. Request for Service: Choose the appropriate benefit plan for each service being requested. If multiple benefit plans are involved, a separate Service Authorization Request is required for each one. List the service code, number of units, start and end date for each service, and indicate any service that is being requested under Early, Prevention, Screening, Diagnostic Treatment (EPSDT). Enter a justification for the service request based on medical necessity for admission or continuing service per the Medicaid Clinical Policy. Be sure to list a Provider contact person and their contact information in the event that Partners BHM Utilization Management needs additional information to process your request. Review Outcome: This section contains the outcome of the review. If approved, the begin date, end date and number of units will be communicated to the provider. If the UM reviewer is unable to approve the request for authorization as submitted, he/she will attempt to contact you to request additional information and communicate the status of the request. The request may be sent to Peer Review, partially denied, denied totally, denied for administrative reasons or unable to process if information is lacking that prevents the review. The reviewer will complete a justification for any status of the request and sign their name. Partners will receive Manual SAR request by mail, fax, email (only if encrypted), or hand delivery: Mailing/hand delivery: Partners BHM Attn: UM Department 901 South New Hope Road Gastonia, North Carolina 28054 Email: Out of Network Paper SAR (only) can be emailed to: providers@partnersbhm.org Fax to: Inpatient Requests: 704-884-2703 Outpatient Requests: 704-884-2701 Innovations/IDD Requests: 704-884-2690 Revised 2/18/2015 SAR MANUAL REQUEST Date of Submission:____________ Provider Name: Provider Address: Site: Consumer Name: Patient ID: SS#: Address: Address 1: Legal Guardian Name: Relation: Self Parent DSS Other Initial Request Reauthorization Expedited: Yes No LOCUS: ASAM: NPI#: MID#: DOB: MH SA DD Date of Initial Assessment: Voluntary Involuntary CALOCUS: NC SNAP/SIS: Diagnostic Profile Substance Use Substance 1: Age of First Use: Frequency: Priority: Route of Usage: Amount: Substance 2: Age of First Use: Frequency: Priority: Route of Usage: Amount: Substance 3: Age of First Use: Frequency: Priority: Route of Usage: Amount: Revised 2/18/2015 Medical Use Primary Care Physician: Compliant Medically Compliant Medically Non-Compliant Medication Signed Release to Primary Physician Comments: Medication Dosage Medication Regimen # of doses per Month Supporting Documents Clinical Doc Type: CCA School Psychological/Psychiatric Evaluation PCP Other EPSDT: Yes No EPSDT: Yes No EPSDT: Yes No Request for Service Benefit Plan: Service Code: Service Code: Service Code: State Service: Service: Service: Medicaid B # of Units: # of Units: # of Units: Medicaid B3 Start Date: Start Date: Start Date: Provider Justification for Service Request: Contact Person: Revised 2/18/2015 Contact Information: Medicaid C End Date: End Date: End Date: Complete this form and attach supporting clinical documentation as indicated for the service on the Medicaid Benefit Plan, which is located on the www.partnersbhm.org website. INFORMATION BELOW TO BE FILLED IN BY PARTNERS MCO UM STAFF ONLY. Review Outcome Approved Total Units: Approved End Date: Approved Effective Date: Status: Peer Review Approved Partial Denial UM Reviewer Justification for Service Request: Reviewer Name: Revised 2/18/2015 Denied Admin Denial Unable to Process