The Effects of Initial Venous Access on the Survival of Patients
advertisement
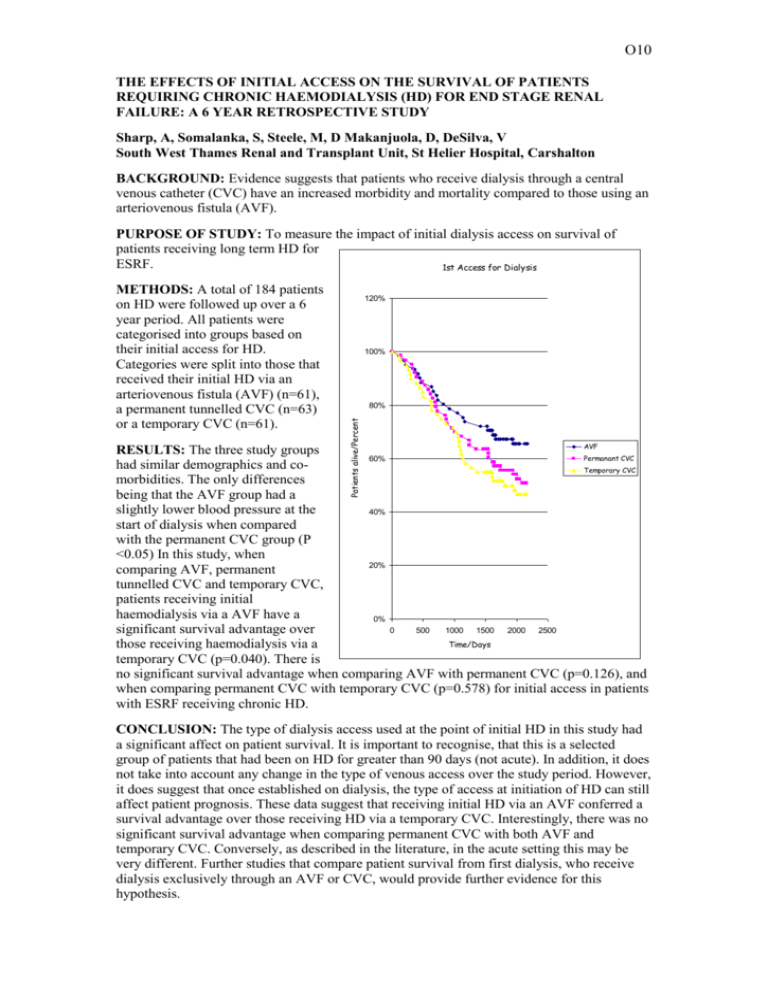
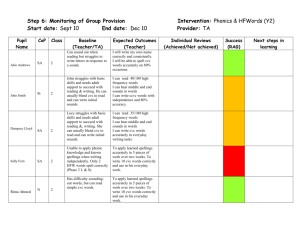
O10 THE EFFECTS OF INITIAL ACCESS ON THE SURVIVAL OF PATIENTS REQUIRING CHRONIC HAEMODIALYSIS (HD) FOR END STAGE RENAL FAILURE: A 6 YEAR RETROSPECTIVE STUDY Sharp, A, Somalanka, S, Steele, M, D Makanjuola, D, DeSilva, V South West Thames Renal and Transplant Unit, St Helier Hospital, Carshalton BACKGROUND: Evidence suggests that patients who receive dialysis through a central venous catheter (CVC) have an increased morbidity and mortality compared to those using an arteriovenous fistula (AVF). PURPOSE OF STUDY: To measure the impact of initial dialysis access on survival of patients receiving long term HD for ESRF. 1st Access for Dialysis 120% 100% 80% Patients alive/Percent METHODS: A total of 184 patients on HD were followed up over a 6 year period. All patients were categorised into groups based on their initial access for HD. Categories were split into those that received their initial HD via an arteriovenous fistula (AVF) (n=61), a permanent tunnelled CVC (n=63) or a temporary CVC (n=61). AVF RESULTS: The three study groups Permanant CVC 60% had similar demographics and coTemporary CVC morbidities. The only differences being that the AVF group had a slightly lower blood pressure at the 40% start of dialysis when compared with the permanent CVC group (P <0.05) In this study, when 20% comparing AVF, permanent tunnelled CVC and temporary CVC, patients receiving initial haemodialysis via a AVF have a 0% 0 500 1000 1500 2000 2500 significant survival advantage over Time/Days those receiving haemodialysis via a temporary CVC (p=0.040). There is no significant survival advantage when comparing AVF with permanent CVC (p=0.126), and when comparing permanent CVC with temporary CVC (p=0.578) for initial access in patients with ESRF receiving chronic HD. CONCLUSION: The type of dialysis access used at the point of initial HD in this study had a significant affect on patient survival. It is important to recognise, that this is a selected group of patients that had been on HD for greater than 90 days (not acute). In addition, it does not take into account any change in the type of venous access over the study period. However, it does suggest that once established on dialysis, the type of access at initiation of HD can still affect patient prognosis. These data suggest that receiving initial HD via an AVF conferred a survival advantage over those receiving HD via a temporary CVC. Interestingly, there was no significant survival advantage when comparing permanent CVC with both AVF and temporary CVC. Conversely, as described in the literature, in the acute setting this may be very different. Further studies that compare patient survival from first dialysis, who receive dialysis exclusively through an AVF or CVC, would provide further evidence for this hypothesis.