BACKGROUND: Renal association vascular access guideline for
advertisement
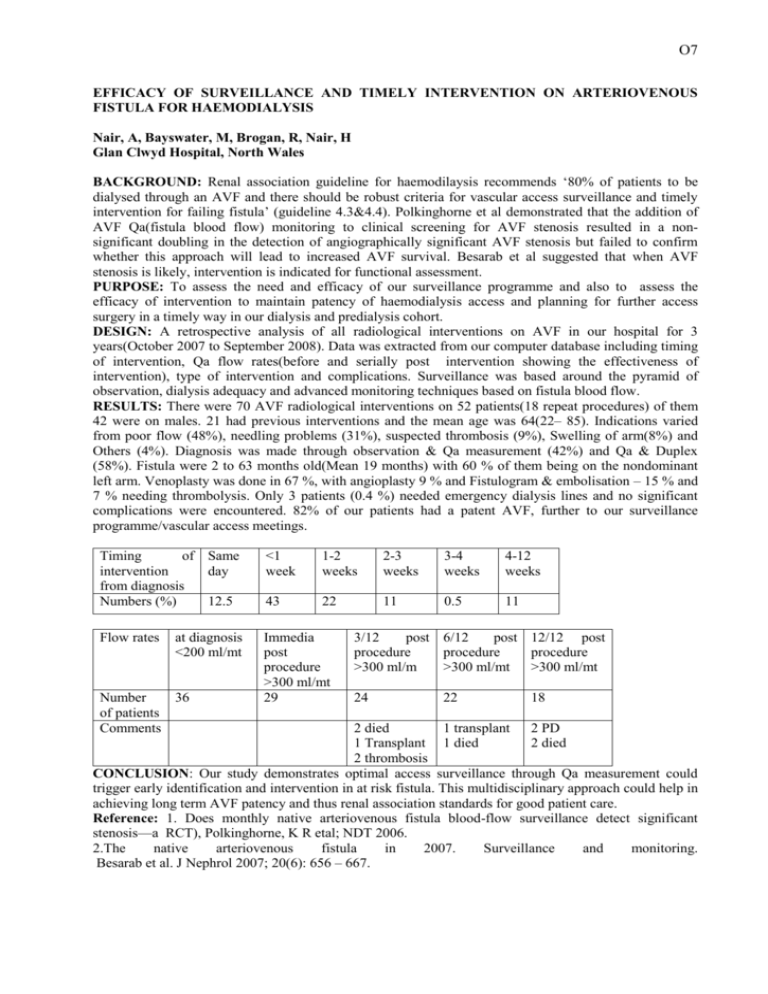
O7 EFFICACY OF SURVEILLANCE AND TIMELY INTERVENTION ON ARTERIOVENOUS FISTULA FOR HAEMODIALYSIS Nair, A, Bayswater, M, Brogan, R, Nair, H Glan Clwyd Hospital, North Wales BACKGROUND: Renal association guideline for haemodilaysis recommends ‘80% of patients to be dialysed through an AVF and there should be robust criteria for vascular access surveillance and timely intervention for failing fistula’ (guideline 4.3&4.4). Polkinghorne et al demonstrated that the addition of AVF Qa(fistula blood flow) monitoring to clinical screening for AVF stenosis resulted in a nonsignificant doubling in the detection of angiographically significant AVF stenosis but failed to confirm whether this approach will lead to increased AVF survival. Besarab et al suggested that when AVF stenosis is likely, intervention is indicated for functional assessment. PURPOSE: To assess the need and efficacy of our surveillance programme and also to assess the efficacy of intervention to maintain patency of haemodialysis access and planning for further access surgery in a timely way in our dialysis and predialysis cohort. DESIGN: A retrospective analysis of all radiological interventions on AVF in our hospital for 3 years(October 2007 to September 2008). Data was extracted from our computer database including timing of intervention, Qa flow rates(before and serially post intervention showing the effectiveness of intervention), type of intervention and complications. Surveillance was based around the pyramid of observation, dialysis adequacy and advanced monitoring techniques based on fistula blood flow. RESULTS: There were 70 AVF radiological interventions on 52 patients(18 repeat procedures) of them 42 were on males. 21 had previous interventions and the mean age was 64(22– 85). Indications varied from poor flow (48%), needling problems (31%), suspected thrombosis (9%), Swelling of arm(8%) and Others (4%). Diagnosis was made through observation & Qa measurement (42%) and Qa & Duplex (58%). Fistula were 2 to 63 months old(Mean 19 months) with 60 % of them being on the nondominant left arm. Venoplasty was done in 67 %, with angioplasty 9 % and Fistulogram & embolisation – 15 % and 7 % needing thrombolysis. Only 3 patients (0.4 %) needed emergency dialysis lines and no significant complications were encountered. 82% of our patients had a patent AVF, further to our surveillance programme/vascular access meetings. Timing of Same intervention day from diagnosis Numbers (%) 12.5 <1 week 1-2 weeks 2-3 weeks 3-4 weeks 4-12 weeks 43 22 11 0.5 11 Flow rates Immedia post procedure >300 ml/mt 29 at diagnosis <200 ml/mt Number 36 of patients Comments 3/12 post 6/12 post 12/12 post procedure procedure procedure >300 ml/m >300 ml/mt >300 ml/mt 24 22 18 2 died 1 transplant 2 PD 1 Transplant 1 died 2 died 2 thrombosis CONCLUSION: Our study demonstrates optimal access surveillance through Qa measurement could trigger early identification and intervention in at risk fistula. This multidisciplinary approach could help in achieving long term AVF patency and thus renal association standards for good patient care. Reference: 1. Does monthly native arteriovenous fistula blood-flow surveillance detect significant stenosis—a RCT), Polkinghorne, K R etal; NDT 2006. 2.The native arteriovenous fistula in 2007. Surveillance and monitoring. Besarab et al. J Nephrol 2007; 20(6): 656 – 667.