Do More With Less - Association for Surgical Education
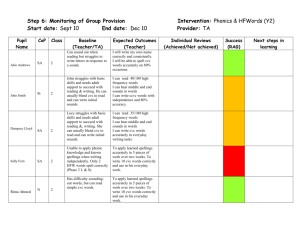
advertisement

Do More With Less: A Surgery Directed Institutional Model for Resident Central Line Training David Leshikar, M.D. Jonathan Pierce, M.D. Edgardo Salcedo, M.D. Gurpreet Bola, B.S. Joseph Galante, M.D. April 23, 2013 “See One, Do One, Teach One” • Apprenticeship model • Little to no supervision • Bedside teaching Simulation Training • Background • Uses • Procedural training • CPR/ACLS • Endoscopy • Laparoscopy • Endovascular • Fundamentals of Laparoscopic Surgery Central Venous Catheters (CVC) • Common bedside procedure • Performed by many specialties • Complications Central Line Simulation • CVC Simulation: • Decreases complications • Improves comfort level • Widespread adoption Barsuk, et al, Crit Care Med, 2009. Barsuk, et al, Arch Intern Med, 2009 Burden, et al, J Clin Anesth, 2012. Procedural Simulation • Expensive • Equipment costs • Faculty time • No standardized assessment metrics • Redundant within institutions Duncan, et al, J Grad Med Educ, 2010 Hypothesis • A curriculum centralized in the department of surgery • Single faculty trainer • Maintain quality of training • Institution wide • Efficient resource utilization Curriculum • Web-based module • Covered all aspects of central line placement • Pre/Post testing • Hands-on simulation training • Technical training – all components • Video assessment Resource Utilization • Equipment costs • CVC simulator • Simulator supplies • Staff productivity • Number of faculty involved • Preparation time • Compared pre vs post implementation Pre-Implementation • Individual departments • Inconsistent simulator use • No standardization Post-Implementation • Study Period: July 2010-June 2012 • Departments involved: • Surgery • Internal Medicine • Emergency Medicine • Family Practice • Pediatrics • Anesthesia • Standardized evaluation • Single faculty trainer Online Module July 2010 – June 2011 July 2011 – June 2012 N= 132 N = 126 Pre-Test Mean 7.0 7.1 Post-Test Mean 8.4 8.4 +1.4 +1.3 < 0.0001 < 0.0001 Difference P value Video Assessments PGY-1 PGY-2 PGY-3 PGY-4+ N=26 N=9 N=5 N=1 Pre-Test Mean 14.2 15.0 12.8 15.0 Post-Test Mean 17.5 15.4 14.8 17.0 Difference +3.3 +0.4 +2.0 +2.0 P value 0.0001 0.426 0.0217 Central Line Infections Mean before, 3.8 infections per 1000 catheter days Mean after, 2.3 infections per 1000 catheter days Resource Utilization Pre-Implementation Post-Implementation 1-5 3-5 5 (4 manufacturers) 2 (single manufacturer) 1 per session 1 per 10 sessions Attending Participation Variable Standardized Attending Preparation Variable Standardized Not standardized Standardized Residents Per Session Simulators Used CVC Kits Facility Preparation Estimated Program Costs Pre-Implementation Post-Implementation Supply Costs CVC Simulator 5 models ($1500) Maintenance 4 manufacturers CVC Kits 1 per session ($100) $7,500 2 models ($1500) Single manufacturer $2600 1 per 10 sessions ($100) $260 Staff Productivity Attending Physicians Preparation Time 10 30 min x 26 sessions $3,000 1 13 hours None Sim Lab Staff Setup 4 manufacturers Single manufacturer Faculty Familiarity 10 different attendings Single attending Summary • Streamlined development • Effective instruction • Improved efficiency Conclusion • Standardization of simulation • Maintained quality of teaching • Decrease resource utilization Questions?