genetic diseases
advertisement

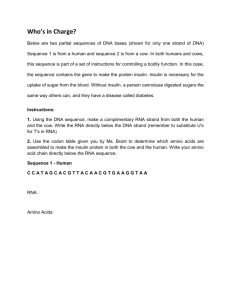
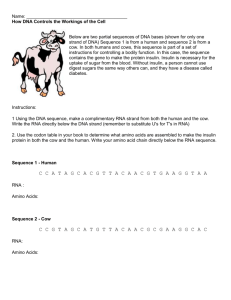
Disease Underlying Cause/ Inheritance Genetic mutation of the CFTR protein; AR Normal Function Diseased Function Symptoms/ Diagnosis Treatment The CFTR protein transports ions like Cl- through the membrane of the epithelia cells and helps regulate fluid and electrolyte balance. In cells like lungs, sinuses, pancreas, intestines, sweat glands. Viscous secretions obstruct organs because Cl- is not excreted out so Na+ absorption is increased (and it absorbs with water). This causes the membranes to be dehydrated and leads to the mucus being sticky Symptoms include: salty skin, distended abdomen, coughing/increased mucus, infertility, clubbed fingers. Testing: sweat chloride test, newborn screening, DNA test G6PD Deficiency Deficient function of G6PD; X-linked R G6PD is responsible for converting NADP+ to NADPH in RBC's which helps fight oxidative stress by reducing GSSG to GSH. Methemoglobemia Increased methemoglobin concentration in the blood; not inherited but can be caused by drugs (sulfa drugs or dapsone) or diseases like G6PD deficiency Depletion of plasma membrane in RBC's; AD When something (like a drug) oxidizes Fe2+ Hgb to met (Fe3+) Hgb, the body uses methemoglobin reductase and NADPH to reduce it back to Fe2+ Without NADPH and GSH, the RBC's cannot fight off oxidative stress and undergo hemolysis causing anemia and jaundice (increase in bilirubin, a blood breakdown product) If there is a lack of NADPH and an oxidizer affecting the blood, the met Hgb percentage increases. Met Hgb binds to oxygen tighter, but does not let it go, reducing the oxygen that goes to the tissues Often asymptomatic unless triggered (illness, antibiotics like sulfa drugs). Symptoms include rapid breathing, jaundice, rapid heartbeat, anemia Symptoms include chocolate brown blood, cyanosis Testing can be done in lab with the hemoglobin Management includes airway clearance techniques and inhaled medications to break up mucus, pancreatic enzymes. N-acetylcysteine can be used to break up the mucus as well. Some treatment may be based upon class with Class 1 being no functional enzyme created and Class 6 being less-thannormal functioning enzyme. Often okay without treatment. In hemolytic anemia, blood transfusions may be necessary. Autoimmune disorder in which antibodies binding to acetylcholine receptors in the neuromuscular junction; not typically inherited through family Normally when impulses travel down the nerve, the nerve endings release a neurotransmitter substance called acetylcholine, which travels through the short neuromuscular junction and results in the activation of muscle contraction. Action potential → motor nerve → nerve terminal → Ach released → combine with AChRs at postsynaptic fold → channel opens → Na+ enters → depolarization at end-plate of muscle fiber → triggers actions potential → muscle contraction → termination via hydrolysis of ACh via ACh Esterase As the plasma membrane is depleted in the cells, they cannot deform and thus can be trapped in microcirculation like in the spleen and are increasing fragile due to the membrane not able to withstand swelling MG occurs due to antibodies binding to ACh receptors in the NMJ. This causes receptors to be blocked/degraded, decreasing the amount of sodium that can flow through nicotinic receptors when ACh is released, and ultimately make it more difficult for end-plate potentials to occur. Enlarged spleen, jaundiced eyes, right shifted osmotic fragility curve, blood smear with spherocytes (small, dark, apparently dense red cells without the usual central pallor) The cardinal features are weakness and fatigability of muscles. The weakness increases during repeated use (fatigue) or late in the day and may improve following rest or sleep. Diagnosis is difficult because a lot of diseases closely resemble MG, there is no definitive test, and treatment may involve surgery and harsh drugs. Tests include ice pack test, serum acetylcholine receptor antibody test, repetitive nerve stimulation Cystic Fibrosis Hereditary Spherocytosis Myasthenia Gravis RBC's need to be deformable to fit through various tight spaces in circulation, so it relies on its plasma membrane to be able to move but still be stable Removal of oxidizing substance, supplemental oxygen, methylene blue (contraindicated in G6PD deficiency) No treatment needed, but should avoid contact sports because of danger to spleen. Treatment: oral anticholinesterase, glucocorticoids and immunosuppressant drugs, intravenous immune globulin, plasmapheresis (directly removes acetylcholine inhibitors from body) Acetylcholine Toxicity/ Organophosphate Poisoning Poisoning by cholinesterase inhibitors, not inherited Acetylcholine is a neurotransmitter that activates nicotinic and muscarinic receptors in the nervous system. It is normally degraded by cholinesterase. Organophosphates are cholinesterase suicide inhibitors, which cause an excess of acetylcholine (ACh) in the synapse. This leads to parasympathetic excess and can lead to death. Diabetes Type 2 Endocrine disorder characterized by high glucose due to body's reduced ability to produce insulin or reduced ability to respond to it. Lots of risk factors including health and genetics. Over production or impaired removal of cholesterol (LDL). Lots of risk factors including health and genetics. Glycogen storage disease resulting from glucose-6-phosphatase deficiency; AR Insulin normally functions to bring in glucose to the cells through the transporter GLUT4 (only one that is insulin dependent). It also promotes glycolysis. Insulin resistance and abnormal insulin secretion are central to the development of type 2 DM. Although the primary defect is controversial, most studies support the view that insulin resistance precedes an insulin secretory defect but that diabetes develops only when insulin secretion becomes inadequate. With hypercholesterolemia, individuals have too much LDL and too little HDL. This causes excess cholesterol in the body which can lead to atherosclerosis. Lack of insulin response leads to accumulation of ketone breakdown from fat; not inherited Normally insulin is used to take in glucose and that is broken down for energy. In fasting fats may also be broken down, which produce ketones but the liver also produces glucose through gluconeogenesis. Familial Hypercholesterolemia Von Gierke Disease Diabetic Ketoacidosis LDL is the lipoprotein that brings cholesterol into the body to be incorporated into cell. HDL is the lipoprotein that brings cholesterol to the liver to be degraded by bile and recycled. Glucose-6-phosphotase is the last step in gluconeogenesis that creates glucose from glucose-6-phosphate In this disease, although the liver is able to create and break down glycogen, it is unable to release glucose into the blood. The result is poor glucose control and marked fasting hypoglycemia. In diabetic ketoacidosis, the fats are broken down into ketones but the body does not have insulin to regulate when to stop the breakdown of fats thus they are overproduced and the body. test among others Symptoms resulting from parasympathetic excess can be summarized by the mnemonic DUMBBELSS: Diarrhea, Urinary incontinence, Miosis, Bronchospasm, Bradycardia, Excitation of skeletal muscle and central nervous system, Lacrimation, Sweating, and Salivation. Central nervous system effects, such as confusion or slurred speech, are common. Symptoms include increased thirst and hunger, weight loss, fatigue, blurred vision, acanthosis nigricans (dark spots on skin), and slow healing sores/frequent infections. Atropine and pralidoxime (2PAM) can reverse organophosphate poisoning. Atropine works by inhibiting muscarinic receptors (it has little effect at nicotinic receptors), thereby decreasing the effect of acetylcholine. 2PAM works by inhibiting the binding of organophosphates to acetylcholinesterase. Lifestyle changes, metformin, insulin, anti-hypertension and cholesterol lowering drugs High blood pressure, high LDL, low HDL, overweight Lifestyle changes, HMG-CoA inhibitor, niacin Seizures, restlessness, vomiting, and sweating that most commonly occur between meals and subside after feeding. Small and protuberant abdomen, liver below the costal margin, and xanthomas, hepatomegaly and bilaterally enlarged kidneys. Symptoms include excessive thirst, frequent urination, nausea and vomiting, abdominal pain, weakness or fatigue, shortness of breath, fruityscented breath, confusion. Testing is done by looking Treatment consists of frequent meals to prevent hypoglycemia. Some patients make cornstarch a central part of their diet because it is absorbed slowly and provides a steady glucose supply. Allopurinol is often used for gout. Liver transplantation is curative. Treatment is replenishing fluids as individuals are often dehydrated and giving insulin, but should always give K+ as well. at glucose, ketone and lactate levels. Alcoholic Ketoacidosis Ketoacidosis due to alcohol intake instead of diabetes Ethanol breakdown creates a lot of NADH which in moderation is completely fine to the body and the body can run both glycolysis and ethanol breakdown If the ethanol breakdown is excessive, there is too much NADH in circulation and the body diverts glucose to other pathways to use up the NADH like lactate and malate. Symptoms are the same as diabetic ketoacidosis Argininosuccinic academia (Urea Cycle Disorders) Defect in arginoscuccinate lyase; all Urea Cycle disorders are AR except ornithine transcarbamylase deficiency which is Xlinked Deficiency of the branched chain alphaketoacid dehydrogenase complex (BCKDC) The urea cycle works to transform toxic ammonia into urea so it can be safely excreted from the body. With a malfunctioning enzyme in the urea cycle, there is a build up of certain cycle intermediates as well as a build-up of ammonia in the body causing hyperammonemia. Branched chain amino acids are broken down into ketoacids and then broken down by BCKDC. They are later converted into propionylCoA and methomalonyl-CoA (isoleucine and valine) or acetylCoA and acetoacetate (leucine) Without the BCKDK, there is an accumulation of ketoacids in the body and they cannot be degraded Gout Accumulation of urate crystals in joint; can happen to anyone, but certain genetics traits can make it more likely The breakdown of DNA and RNA create xanthine which is further broken down into uric acid where it is excreted by the kidneys as urate. Due to the production of too much urate or the excretion of too little uric acid, uric acid builds up in the joints as crystals which become inflamed and are very painful. Homocystinuria Reduced activity of cystathionine synthase (most common but there are 2 other types); AR Methionine is converted to cysteine through several enzymes, one of which is cystathionine synthase. Without the full activity of the enzyme, homocysteine is built up and methionine cannot be fully metabolized and cysteine becomes an essential amino acid. Symptoms include muscle weakness, fatigue, liver and kidney damage, and seizures. Testing can be done by looking at enzymatic function and the intermediate build-up. Symptoms include maple syrup sugar odor in sweat, ear wax and urine, vomiting, anorexia, muscle fatigue, and neurologic symptoms. Testing can be done in prenatal screening. Intense joint pain, lingering discomfort, inflammation and redness. The only sure diagnosis can come from joint fluid test where the crystals are looked at to see if it's uric acid (but people tend to not like that) Vision difficulties (dislocated lenses), tall, thin body with long extremities (similar to Marfan syndrome) Osteogenesis Imperfecta Defect in type I collagen; various patterns of inheritance, but often AD and spontaneous mutations are common Collagen I is in the bones, tendons, ligaments, and sclera. It is synthesized from 3 alpha chains which then are cleaved and formed into collage fibrils. These are then used in connective tissue to provide resistance to force, tension and stretch. Due to a mutation in the collagen, it cannot form the alpha helix properly. This causes significant bone fragility due to the disruption of the bone matrix with the malformed collagen Maple Syrup Urine Disease Malformed body, loose ligaments, muscle weakness, curved spine, frequent fractures. Can be tested using skin biopsy and DNA testing. Both are as the biopsy looks at the extent of collagen malfunction and the DNA test looks at Treatment is replenishing fluids, thiamine/Mg (must give this with any glucose) to prevent Wernicke-Korsakoff (complete thiamine deficiency). In some cases other drugs may be given to fix the NADH/NAD+ ratio. Treatments include arginine supplementation, hemodialysis, low protein diet and hyperammonemia drugs. Special diet of purified amino acids Anti-inflammatory drugs, medication that block xanthine oxidase, and medicine that improve urate removal. Vitamin B6 (pyridoxine) is a necessary cofactor with cystathionine synthase. A diet low in methionine and cysteine supplementation is also necessary. Minimizing fractures, braces, physical therapy Fragile X Syndrome Mutation in FMR1 gene causing mental retardation; X-linked with anticipation The FMR1 gene makes the FMRP which helps regulate protein production in synapses. In the full mutation, due to CGG repeats, the protein is not produced causing mental retardation. A premutation can occur in individuals with <200 repeats and have generally milder symptoms Ehlers-Danlos Syndrome Mutation of type III collagen; inheritance varies by type, but most are AD Collagen III is located in tissues, organs, smooth muscle and blood vessels. It is produced in the same manner as collagen I. Non-syndromic Deafness Hearing loss with no other symptoms (many different mutations but most often GJB2); most inheritance is AR Lysosomal storage disease due to a defect in the HEXA gene; AR GJB2 and GJB6 provide instructions for making connexin which are subunits of gab junctions. These gap junctions allow communication between neighboring cells. The HEXA gene provides instructions for making part of an enzyme, beta-hexosaminidase A, which plays a critical role in the brain and spinal cord. This enzyme is located in lysosomes. Within lysosomes, beta-hexosaminidase A helps break down a fatty substance called GM2 ganglioside. The defect in Ehlers-Danlos causes frequent bruising due to the abnormal collagen in the blood vessels among other symptoms (but much milder issues compared to OI) Without the gap junctions, so of the cells are damaged due to ion accumulation (K+) and thus hearing is lost. Disruption of dystrophin causing muscle wasting; AR 2 main types Duchenne's (severe) and Becker's (mild) Dystrophin normally provides mechanical reinforcement to the sarcolemma and stabilizes the glycoprotein complex, thereby shielding it from degradation. Tay-Sachs Disease Muscular Dystrophy Mutations in the HEXA gene disrupt the activity of beta-hexosaminidase A, which prevents the enzyme from breaking down GM2 ganglioside. As a result, this substance accumulates to toxic levels, particularly in neurons in the brain and spinal cord. Progressive damage caused by the buildup of GM2 ganglioside leads to the destruction of these neurons, which causes the signs and symptoms of Tay-Sachs disease. Mutations in the DMD gene alter the structure or function of dystrophin or prevent any functional dystrophin from being produced. Muscle cells without enough of this protein become damaged as muscles repeatedly contract and relax with use. The damaged fibers weaken and die over time, leading to the muscle weakness and heart problems characteristic of Duchenne and Becker muscular dystrophies. Mutations that lead to an abnormal version of dystrophin that retains some function usually cause BMD. mutations alone. Full mutation: large face, enlarged testes, developmental delay. Girls may have the full mutation due to nonrandom X chromosome inactivation. Pre-mutation: tremor and ataxia and premature ovarian insufficiency Testing is done through DNA or chromosome analysis Hyperextendible joints, flat feet, frequent bruising, frequent dislocation, dental crowning. Can be tested through DNA analysis Loss of hearing No treatment. Special education can be used to help with some of the neurologic symptoms No treatment No treatment Progressive neurodegeneration, developmental delay, cherry red spot on macula No treatment In boys with Duchenne muscular dystrophy, muscle weakness tends to appear in early childhood and worsen rapidly. Affected children may have delayed motor skills, such as sitting, standing, and walking. The signs and symptoms of Becker muscular dystrophy are usually milder and more varied. In most cases, muscle weakness becomes apparent later in childhood or in adolescence and worsens at a much slower There is no treatment Phenylketonuria (PKU) Deficient function of phenylalanine hydroxylase (PAH); AR PAH is responsible for converting phenylalanine into other important components of the body (one of which is tyrosine) Without PAH, there is a buildup of phenylalanine and a lack of tyrosine. There are different forms of PKU: the classic is the most severe with little to no function of PKU, milder forms like variant PKU may not require treatment. Hereditary BreastOvarian Cancer Syndrome (HBOC) Mutation of the BRCA1/2 gene; AD BRCA1 and 2 are tumor suppressor genes involved in the repair of double strand breaks, specifically the error-free homologous recombination. Mutated BRCA 1 or 2 make DNA repair rely on non-homologous end joining for repair and (including creation of dicentric chromosomes) and can often lead to cancer. Retinoblastoma Mutation of RB1 gene; germline Retinoblastoma appears to be AD (one inherited gene is sufficient to increase cancer risk), but need two RB1 mutations (loss of heterozygosity) RB1 is a tumor suppressor gene that codes for RB. RB keeps the cell cycle from progressing past G1 by binding to the transcription factor E2F. Without a functioning RB, the cell cycle cannot be regulated at that point, leading to cell cycle dysregulation and cancer Xeroderma Pigmentosum Deficient in proteins involved in global genome nucleotide excision repair (GGNER); AR With no GG-NER, the body cannot repair damage due to UV radiation and the likelihood of getting skin cancer increases 1000 fold Lynch Syndrome; Hereditary Nonpolyposis Colorectal Cancer (HNPCC) MMR gene mutation (MSH2, MLH1, MSH6, PMS2); appears AD but inactivation of both needed The GG-NER can fix nucleotide errors anywhere in the DNA (not just on the transcribed strand) and is much slower than the other TCNER. The GG-NER is particularly important with fixing pyrimidine dimers which occur due to UV radiation. MMR fixes mismatched bases by recognizing, removing, and rewriting the DNA (template and nascent strands distinguished by single stranded breaks on nascent strand) Non-Small Cell Lung Cancer (NSCLC) Lung cancer is caused by a stepwise accumulation of genetic abnormalities (smoking is a major cause); not inherited Non-Small Cell Lung Cancer: There are different types of NSCLC (adenocarcinoma is most common follow by squamous cell, then large cell carcinoma) Superior Vena Cava Caused by gradual The superior vena cava is a large Some important carcinogens are Nnitrosamines (create DNA adducts and interfere with DNA replication) and Benzo(a)pyrene (metabolite BDP induces transversion G to A and inactivates p53, a tumor suppressor) Compressing a major vein is bad for Without MMR, there microsatellite instability (MSI). Errors are likely to occur on the microsatellites (repeated DNA sequences), which can then cause frameshift mutations as these microsatellites expand or contract leading to cancer. rate. Mental retardation, mousy odor (due to the increase in Phe), decreased pigmentation (decrease in Tyr as it is a precursor to melanin). Part of the newborn screening test, which looks at hyperphenylalaninemia. Increased risk of breast, ovarian, prostate cancers; genetic testing can be done to find the mutated BRCA genes Leukocoria (white reflection in eye), Strabismus (lazy eye). In the germline mutation, children are most likely affect and it occurs in both eyes; in the somatic mutation, adults are more likely affect and in only one eye. Freckles, changes in pigmentation (both hypopigmentation and hyperpigmentation), and dry skin after sun exposure. Testing can be done by doing a skin biopsy and looking at the DNA repair Symptoms include rectal bleeding, predominately right sided cancer, and changes in bowel habits. Amsterdam Criteria for HNPCC: 3 family members with colorectal cancer, 2 successive generation, 1 diagnosis before 50 Often only see symptoms of lung cancer in advanced stages and include coughing, dyspnea, hemoptysis, chest pain. Diagnosis is through chest X-rays SVC syndrome typically Low Phe diet and Tyr supplements. Pregnant mothers with PKU need to be on a Phefree diet to prevent newborn being born mentally retarded Surgical treatment recommended is mastectomy due to the high chance of recurrent breast cancers, radiation therapy and chemotherapy Surgery (eye removal), radiation, chemotherapy, and other forms of cancer treatment No cure; sun avoidance, frequent skin and eye exams are used to prevent cancer. Typical cancer treatments including surgery, radiation, chemotherapy. Frequent colonoscopies are also recommended to find cancer early. Stage I, II, and some III cancers can be treated with surgery. Systemic treatment is given for advanced stages of cancer. Overall, prognosis for lung cancer is one of the poorest of all cancers. Treatment is most often fixing Syndrome (SVCS) compression of the superior vena cava from an enlarging mass (most often lung cancer, can also be lymphoma, and metastatic cancer); not inherited vein that transmits blood from the upper body back to the heart. the body X-linked Hyper IgM Syndrome Mutations in the CD40L gene; XL CD40L is present on T cells and binds to CD40 which is on APC (including B cells). Connection is needed for the B cells to undergo heavy chain class switching and produce IgG, IgA, IgE antibodies. Without heavy chain class switching, the immune system cannot respond as readily to pathogens in the adaptive system. Immune memory may also not be functional due to the lack of antibody differentiation. IgA Deficiency Most common primary immunodeficiency disease; body does not produce IgA; both AD and AR (may occur with other Ig deficiencies or alone) IgA antibodies are mostly found in the secretions of mucosal surfaces so protects from infection in those areas. Tuberculosis (TB) Caused by inhalation of Mycobacterium tuberculosis; very infectious and transmitted through droplets Epidemiology: Bacteria is a slow growing, and stains with acid-fast stains. Found predominantly in Africa and parts of Asia. (1/3 of the world is latently infected) Without IgA, more prone to infections of the lungs, ears, and GI. When exposed to blood containing IgA, will have an anaphylaxis reaction due to IgG antibodies present against IgA. There is an increased risk of developing other autoimmune diseases as well as intestinal diseases due to the higher chance of developing a food allergy without IgA in the intestines (celiac disease and milk allergy) Latent TB and active forms; only a small amount of individuals with TB get the active form (HIV/immunosuppressed). Miliary TB can occur in kids and causes widespread disease. Malaria Plasmodium species (P. falciparum, P. vivax, P. malariae, P. ovale, P. knowlsei), vector is the female Anopheles mosquito Malaria Life Cycle: Sporozoites released into the blood and infect the liver (exoerythrocytic phase) and develop into merozoites (motile, infective stage), which are released and invade RBCs in the peripheral blood. Asexual reproduction in RBCs lead to release of more merozoites. Some gametocytes are produced which leads to sexual P. falciparum can is more like severe malaria (especially cerebral malaria) P. ovale and vivax can arrest as hypnozoites and relapse. has an insidious onset, with dyspnea, and may include cough, upper extremity swelling, chest pain and dysphagia due to esophageal compression. Common physical findings include venous distention of the neck and chest wall, facial edema, plethora, and cyanosis. Diagnosis is often done through contrastenhanced CT scan Frequent pyogenic infections and pneumonia. Lots of tests are given including: CBC, quantitative Ig test (looks at Ig types), lymphocyte phenotype analysis, T cell CD40L levels Many individuals are asymptomatic, but may have had frequent ear and lung infections as well as issues in their GI tract. Diagnosis seen through blood tests where IgA is at undetectable levels the underlying cause of the compression or obstruction Night sweats, coughing, shortness of breath, weight loss, fever. Diagnosis is done through PPD and IGRA (blood test) to test infection. Disease can be confirmed through PCR and cultures. Fever and chills often with a periodicity. Possibly anemia and splenomegaly. Severe malaria is when many RBCs have the parasite and they stick to blood vessels causing seizures, coma, respiratory distress, renal failure, liver failure and hypoglycemia. Active TB treatment: 4-drug regimen (isoniazid, rifampin, pyrazinamide, and either ethambutol or streptomycin); must be at least 2. Latent TB treatment: one drug is okay, often rifampin or isoniazid Chloroquine is used for malaria that is sensitive to it. It will not kill hypnozoites so for P. ovale and vivax chloroquine and primaquine are given Antibiotics for infections, IgG therapy, bone marrow transplant (only curative therapy) For individuals experiencing anaphylaxis due to blood transfusions, they should be stopped and given epinephrine, which counteracts the bronchospasms and vasodilation reproduction in the female Anopheles mosquito Neonatal Sepsis Group B Streptococcus (GBS), E. coli, and Listeria monocytogenes are common causes of sepsis Sepsis definition: SIRS plus source of infection SIRS (Systemic Inflammatory Response Syndrome) is: Fever > 100°F or < 96.8°F Heart rate > 90 bpm Respiratory > 20 bpm Abnormal WBC count (>12,000/µL or < 4,000/µL) GBS often colonize the vaginal flora and can be transmitted during delivery, so neonatal sepsis is likely to be due to GBS. Prenatal testing where vaginal cultures are performed try to prevent this Influenza Influenza virus, Type A, B and C; transmitted through droplets Virus: Virus is a linear single stranded negative segmented genome, helical and enveloped Antigenic shift/drift: Antigenic drift caused by inefficient proofreading leading to small changes (both A and B can do this) Follows through regular replication cycle as RNA viruses, except transcription and replication occur in the nucleus Antigenic shift caused by simultaneous infections of two viruses which create a virus with new surface proteins (H and N are different; only occurs in A) The virus preferentially kills CD4 T cells and uses the others as virus reservoirs. The decrease in CD4 T cells and rise in virus is correlated with disease progression. There is a period of latency after the initial infection that can last about 10 years without treatment. When CD4 T cells drop below 200, the disease is considered to progress to AIDS and many opportunistic infections are possible HIV HIV virus; transmitted through sexual contact, injection drug use, pregnancy, and rarely blood transfusions Aspergillus Infections Infection with Aspergillus (Aspergillus fumigatus is most often seen) Virus: Lentiviruses of the subfamily retrovirus; are enveloped and have a complex capsids. They have a linear single stranded positive sense diploid genome Uses the CD4 molecules as receptors and enters T cells, monocytes/ macrophages, and dendritic cells (and also use chemokine surface co-receptor CCR5CXCR4). It integrates genome into the host using integrase and produces more viruses. Epidemiology: Found commonly in nature, even in air ventilation ducts Can cause 3 main diseases: Allergic bronchopulmonary aspergillosis (ABPA): a reaction to colonization in airways similar to asthma Invasive aspergillosis (IA): Occurs in patients with prolonged neutropenia. Seen as infarcts in Diagnosis is through thick smears (easier to see parasites), and thin smears (morphology). The headphone shape is consistent with P. falciparum Symptoms see sepsis definition. Diagnosis with Gram staining of a blood sample: GBS appear as grampositive cocci, L. monocytogenes appears as motile gram-positive rods, and E. coli appears as gram-negative rods. Fever, body aches, coughing, chills Diagnosis is done through a nasal pharyngeal swab Penicillin is used as antibiotic treatment for GBS. Vaccine is the best way to prevent illness. Often does not need to be treated, but high risk groups may take neuroaminidase inhibitors (oseltamivir and zanamivir) Flu-like symptoms at the onset and a period of latency. Symptoms of AIDS include night sweats, swollen lymph nodes, weight loss, easy bruising, lethargy, shortness of breath Diagnosis is done through rapid HIV test, CD4/CD8 count, HIV viral load Treatment involves at least 3 drugs; classes of these drugs are: reverse transcriptase inhibitors (NRTIs and NNRTIs), fusion/entry inhibitors, integrase inhibitors and protease inhibitors. Usually 2 NRTIs and 1 other class. Symptoms include asthma like symptoms, cough, hemoptysis. Diagnosis is done through staining: Aspergillus infections appear as sepatated hyphae with 45 degree branching ABPA is treated with steroids, IA is treated with antifungals like voriconazole and amphotericin B, and Aspergilloma is not treated but fungus may be surgically removed. lungs, sinuses, and brain; poor outcome Celiac Disease Production of antitissue transaminases IgA Epidemiology: Common in Caucasians, highest incidence infancy but may appear during pregnancy or later in life. Celiac disease is an autoimmune disease a correlation with type 1 diabetes and other autoimmune diseases Diabetes Type 1 Body damages the insulin producing beta cells in the body; familial predisposition but inheritance pattern is unknown Insulin is used to move glucose in the bloods into cells (use the GLUT4 transporter) Aspergilloma of fungus ball in preexisting cavity (can sometimes be seen in past TB patients). Not invasive Gliadin, a component of gluten, is taken up in the small intestine and altered by tissue transglutaminase. The altered gliadin protein is presented by MHC-II complexes on enterocytes. TH1 Cells bind to the MHC-II-gliadin complex and initiate antibody production against gliadin, which have cross-reactivity with tissue transglutaminase and also release pro-inflammatory cytokines. Weight loss, pallor due to anemia, steatorrhea, dermatitis herpetiformis, nutritional deficiencies (iron, vitamins) Diagnosis can be done through HLA typing (HLADQ2 and DQ8), tissuetransglutaminase Ig production, and duodenal biopsy Gluten free diet; Dapsone can be used to treat dermatitis herpetiformis (However, there are issues with methemoglobinemia so may also be taken with cimetidine) Lack of insulin means that the body cannot use glucose as a source of energy in cells or control the amount of sugar in the blood. Untreated DM1 leads to diabetic ketoacidosis. Polyuria, polydipsia, fatigue, blurred vision (can progress to blindness), peripheral neuropathy, weight loss Insulin (glargine and lispro), healthy lifestyle, frequent blood glucose monitoring