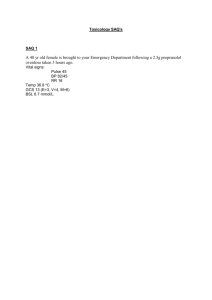
Lead poisoning: (Please select 1 option) Causes adrenal
advertisement

Lead poisoning: (Please select 1 option) Causes adrenal suppression Incorrect answer selected Can only result from lead ingestion Is associated with a macrocytic anaemia Causes a peripheral neuropathy due to demyelination This is the correct answer Commonly presents with diarrhoea Lead can also be absorbed through the skin and by inhalation. Associated with iron deficiency & a microcytic anaemia. Most common GI symptoms are abdominal colic and constipation A 17-year-old female presents to the emergency department following self-confessed paracetamol poisoning after discovering she is eight weeks pregnant and had a row with her boyfriend. She claims to have taken an approximately 30 paracetamol tablets approximately 58 hours ago. Her history is considered to be reliable. There are no abnormalities to find on examination. Her blood sugar by finger prick testing was 3.1 mmol/l. Which of the following would be the most appropriate treatment for this patient? (Please select 1 option) Haemodialysis Intravenous dextrose infusion Intravenous N-acetylcysteine Correct Oral activated charcoal Oral vitamin K Irrespective of the pregnancy, this girl should receive n-acetyl cysteine. Paracetamol concentration is unhelpful in delayed presentation of paracetamol overdose. A dose of more than150mg/kg is considered to be toxic and toxicity occurs at a lower concentration if the patient is thought to be in high risk group. Clotting screen international normalised ratio (INR), liver function tests, acid-base balance and plasma glucose should be taken without delay prior to starting treatment with N-acetylcysteine. Serial monitoring of clotting screen is required and N-acetylcysteine should continue until INR returns to normal. Further advice on treatment of complicated cases should be sought from National Poisons Information Service. Other supportive treatment is guided by the patient's condition. A 60-year-old male who has been prescribed lisinopril for hypertension presents with an irritating cough. What is the mechanism responsible for ACE-induced cough? (Please select 1 option) Angiotensin I accumulation Asthma Bradykinin accumulation Correct Laryngeal irritation Renin accumulation The enzyme ACE is also responsible for the metabolism of bradykinin in mast cells. The accumulation of this substance is responsible for the cough found in up to 30% of subjects taking ACE-inhibitors. This phenomenon is not seen in subjects taking Angiotensin receptor blockers such as Losartan. A 30-year-old man is admitted three hours after taking an overdose of amitriptyline and diazepam. On examination he was drowsy with a Glasgow coma scale of 8, he had a pulse of 140 beats per minute, a blood pressure of 114/88 mmHg and dilated pupils. His oxygen saturation was 90% on room air. What is the most appropriate initial action for this patient? (Please select 1 option) Activated charcoal CT head scan ECG This is the correct answer IV atenolol IV flumazenil Incorrect answer selected Daft question really. The most appropriate initial action would be to get the investigations done as quickly as possible - arterial blood gases and ECG, as the latter may show QRS widening and merit treatment. Then, the next step would be gastric decontamination with lavage and activated charcoal. Treatment with bicarbonate is also advocated as this patient displays features of severe TCA overdose. He does not need a CT scan as the symptoms are typical of tricyclic overdose. Flumazenil is not appropriate for this patient as the symptoms are mostly of TCA overdose nor is IV atenolol appropriate for the arrhythmias - bretylium, phenytoin or lidocaine A 58-year-old male presents with painful breast tissue. Six weeks previously he was treated for atrial fibrillation and had a number of drugs commenced. Which one of the following drugs may have caused this problem? (Please select 1 option) Aspirin Digoxin Incorrect answer selected Flecainide Spironolactone This is the correct answer Warfarin Digoxin may cause gynaecomastia but usually only on prolonged use. Spironolactone is well known to cause gynaecomastia due to its well described anti-androgen effects. A 24-year-old female who has previously suffered with severe depression presents with secondary amenorrhoea. She is found to have a prolactin of 645mU/L (normal 50-350). Which of the drugs which she takes may cause this? (Please select 1 option) Becotide Omeprazole Montelukast Risperidone Sertraline This is the correct answer Incorrect answer selected Antipsychotic medications are known to elevate prolactin levels, due to dopamine antagonist effects. Sertraline is not thought to exert dopamine antagonist effects and thus does not result in hyperprolactinaemia. The other medications on her list have not been associated with hyperprolactinaemia. A middle-aged lady presents with cervical and inguinal lymphadenopathy. She is also experiencing pins and needles in a glove and stocking distribution, and has gum hypertrophy. She has a previous history of epilepsy and is on regular medication. Which of the following drugs is most likely to cause her symptoms? (Please select 1 option) Carbamazepine Phenobarbitone Phenytoin Correct Sodium valproate Vigabatrin Recognised side effects of phenytoin include drowsiness ataxia confusion blurred vision dizziness nystagmus permanent cerebellar ataxia peripheral neuropathy rashes gum hypertrophy thickening of the facial features lymphadenopathy chorea sleep disturbance. Remarkable side effects of other anti-epileptic drugs are: drowsiness blurred vision dizziness leukopaenia SIADH and rash (carbamazepine) liver toxicity (sodium valproate) severe rash (lamotrigine) retinal damage (vigabatrin) aplastic anaemia (felbamate). A 42-year-old man presents with gingival hypertrophy. Which of his cardiac medications is likely to be responsible? (Please select 1 option) Amlodipine Correct Atenolol Digoxin GTN Simvastatin Calcium channel blockers and drugs like phenytoin and cyclosporin are associated with gingival hypertrophy. A 60-year-old male with diet controlled type 2 diabetes mellitus is commenced on metformin due to deteriorating glycaemic control. Which of the following is true regarding metformin? (Please select 1 option) It does not require any functioning pancreatic islet cells for its action Incorrect answer selected It is contra-indicated in patients suffering a myocardial infarction (MI) correct answer This is the It is safe in patients with renal impairment It may cause metabolic alkalosis It often causes hypoglycaemia Metformin is a biguanide which acts to improve insulin sensitivity through mechanisms that involve hepatic gluconeogenesis and improved muscle glucose utilisation. Thus, some insulin must be produced for it to have an effect. It is associated with hypoglycaemia although this side effect is unusual. It is contra-indicated in subjects with renal failure, hepatic failure and heart failure due to the association with lactic acidosis. The BNF states that there should be a six week "cooling off" period post-MI before the commencement or recommencement of metformin. A 60-year-old retired nurse with idiopathic Parkinson’s disease presented with motor oscillations and on-off periods. She had received Co-Beneldopa for 5 years. Selegiline was added to her treatment. Which one of the following enzymes does Selegiline act on to cause this adjuvant action? (Please select 1 option) catechol-0-methyltransferase dopa decarboxylase dopamine hydroxylase monoamine oxidase Correct tyrosine hydroxylase Selegiline is a MAO-B inhibitor Which of the following pharmacological agents acts through the opening of potassium channels? (Please select 1 option) Amiloride Glibenclamide Lidocaine Nicorandil Correct Phenytoin Nicorandil is a potent potassium channel activator. It relaxes vascular smooth muscle through membrane hyperpolarization via increased transmembrane potassium conductance and, like nitrates, through an increase in intracellular cyclic GMP. Glibenclamide blocks potassium channels. Amiloride inhibits the action of aldosterone on the distal convoluted tubule producing potassium reabsorption. Which of the following is a metabolic effect of exenatide? (Please select 1 option) Accelerates gastric emptying Improves insulin sensitivity Incorrect answer selected Inhibits insulin release Promotes gluconeogenesis by the liver Suppresses appetite This is the correct answer Exenetide mimics the effect of the gut hormone GLP-1 (glucagon-like peptide 1) and has favourable effects on the metabolism of individuals with diabetes mellitus. Exenetide suppresses appetite, inhibits glucose production in the liver, slows gastric emptying and stimulates insulin release. It does not increase insulin sensitivity which is achieved by drugs such as metformin and the glitazones. In summary exenatide has the following metabolic effects: Stimulates insulin release Inhibits glucose production by the liver Slows gastric emptying Suppresses appetite. Diabetes Care 27:2628-2635, 2004 A 60-year-old female suffers from bipolar affective disorder and is being treated with Lithium. She also has a long history of hypertension for which she is on treatment. During a recent clinic visit her blood pressure was noted to be 170/94 mmHg and a new antihypertensive agent was added. A week later she presents with features of Lithium toxicity including tremor, nausea and weakness. The addition of which one of the following drugs was likely to have precipitated the Lithium toxicity? (Please select 1 option) Doxazosin Hydrallazine Lisinopril Correct Minoxidil Moxonidine The precipitation of Lithium toxicity by diuretics is well appreciated. Yet ACE inhibitors and Angiotensin Antagonists are also capable of precipitating Lithium toxicity through reduced Lithium clearance. Other drugs that may precipitate Lithium toxicity include NSAIDs, tetracycline, phenytoin and ciclosporin. A 68-year-old lady presented to her general practitioner with a history of generalised tiredness. She had recently been commenced on a water tablet to ease her swollen feet. She was also diagnosed with glaucoma for which she used topical eye drops. Investigations: Serum sodium 138 mmol/L (137-144) Serum potassium Haemolysed sample Serum urea 4.3 mmol/L (2.5-7.5) Serum creatinine 88 µmol/L (60-110) Serum corrected calcium 2.68 mmol/L (2.2-2.6) Which diuretic was this lady most probably taking? (Please select 1 option) acetazolamide amiloride bendroflumethiazide Correct furosemide indapamide Thiazide diuretics are associated with increased calcium concentrations as well as raised urate A 62-year-old male presented to the urologists with symptoms of urinary hesitancy and dribbling. They diagnose benign prostatic hyperplasia and he is commenced on finasteride. Through which of the following mechanisms does finasteride function? (Please select 1 option) 5-alpha-reductase inhibitor Alpha receptor antagonist LHRH analogue Correct LHRH antagonist Testosterone receptor antagonist Finasteride is a 5-alpha-reductase inhibitor preventing the conversion of testosterone to the active dihydrotestosterone (DHT). Consequently this agent opposes testosterone, so gynaecomastia and reduced libido are common side effects. It is also taken orally (under the brand name Propecia) for the treatment of male pattern hair loss! A 17-year-old boy is admitted with a severe paracetamol overdose following an argument with his girlfriend. He is treated with intravenous N-acetylcysteine. Paracetamol is normally metabolised to harmless compounds except in overdose. Which of the following compounds is the toxic metabolite that accumulates during paracetamol overdose and is reduced by treatment with Nacetylcysteine? (Please select 1 option) Glucuronide Homocysteine Methionine N-acetyl-p-benzoquinoneimine Correct N-hydroxyacetaminophen Paracetamol is predominantly metabolised to glucuronide and sulphate conjugates, which are excreted in the urine. Hepatotoxicity is related to the conversion of a small proportion of the ingested dose to N-acetyl-p-benzoquinoneimine. In therapeutic doses N-acetyl-pbenzoquinoneimine is detoxified by conjugation with glutathione in the liver, but once the protective intracellular glutathione stores are depleted hepatic and renal damage may ensue. NAC and Methionine replenishes glutathione stores in the liver and may also act through its Sulphhydryl (-SH) group as a direct reducing agent. Further Reading: Wikipedia - paracetamol OD 75-year-old patient being treated for heart failure presents with hyperkalaemia, the potassium being 6.9mmol/L (Normal 3.5-5.0). He was recently commenced on Amiloride. The interaction of Amiloride with which of his drugs listed below is likely to have caused the hyperkalaemia? (Please select 1 option) Bisoprolol Digoxin Metolazone Perindopril Correct Warfarin The co-administration of a potassium-sparing diuretic and an ACE inhibitor, in this case Perindopril, may result in profound hyperkalaemia, as has occurred in this patient. Thus patients on both these drugs should have their potassium monitored closely. Metolazone may result in profound hypokalaemia Which one of the following is a recognised treatment option in poisoning? (Please select 1 option) Ethanol for isopropyl alcohol poisoning Glucagon for cocaine poisoning Methylene blue for cyanide poisoning N-acetylcysteine in paraquat poisoning Pralidoxime in sarin (nerve gas) poisoning Correct Sarin is an organophosphorus. Pralidoxime reactivates acetyl cholinesterase enzyme. It should be used in the first few hours. Ethanol reduces the formation of toxic metabolites produced after ingestion of methanol and ethylene glycol, but not isopropyl alcohol. Glucagon is used in symptomatic beta-blocker overdose. N-acetylcysteine is used in paracetamol overdose. Methylene blue is the antidote for serious methaemoglobinaemia. A 55-year-old male who is being treated with Lithium for a bipolar disorder has a long history of hypertension for which he is receiving escalating doses of medication. On his most recent visit to clinic his blood pressure was noted to be 166/102 mmHg and new antihypertensive was added to his current antihypertensive therapy. Five days later he presents with features of Lithium toxicity including tremor, nausea and weakness. The addition of which of the following drugs was likely to have precipitated the Lithium toxicity? (Please select 1 option) Doxazosin Hydrallazine Irbesartan Minoxidil Correct Moxonidine The precipitation of Lithium toxicity by diuretics is well appreciated. Yet ACE inhibitors and Angiotensin Antagonists are also capable of precipitating Lithium toxicity through reduced Lithium clearance. Other drugs that may precipitate Lithium toxicity include NSAIDs, tetracycline, phenytoin and ciclosporin A 44-year-old man presents with new onset bilateral gynaecomastia. He has been diagnosed with Zollinger-Ellison syndrome in the last year. He underwent normal puberty at age 14. Which of the following drugs would be most likely to cause gynaecomastia? (Please select 1 option) Cimetidine Correct Famotidine Lanzoprazole Rabeprazole sodium Ranitidine The answer to this question is cimetidine which is an H2 receptor antagonist. Blockade of androgen-responsive receptors in the target organ appears to be the most likely mechanism involved. Reasearch has shown that the other drugs listed above which may also be used as part of the treatment of Zollinger-Ellison syndrome have a much lower almost insignificant risk in the development of gynaecomastia. Other drugs that can casue gynaecomastia include - spironolactone, digoxin, methyldopa, gonadotrophins and cyproterone acetate. Zollinger-Ellison sydrome The association of peptic ulcer with a gastrin-secreting pancreatic adenoma - 50-60% are malignant. It occurs in approx 0.1% of patients with duodenal ulcer disease and is to be suspected in those with multiple peptic ulcers that are resistant to drugs. In a study, healthy volunteers are given 50 mls of 50% dextrose solution by one of two routes. Route A is intravenous and Route B is via a nasogastric tube. Every 15 minutes the plasma insulin level and glucose is measured and plotted on a graph. Which of the following statements would best describe the likely results comparing Route A to Route B in this experiment? (Please select 1 option) Insulin higher, glucose higher in Route A Insulin higher, glucose higher in Route B Insulin higher, glucose lower in Route A Insulin higher, glucose lower in Route B This is the correct answer Insulin and glucose the same in Route A and Route B Incorrect answer selected Glucose given via the gut elicits a greater insulin response as compared to the same quantity given intravenously even though the plasma glucose peak is higher when it is given IV. This phenomenon is called the 'incretin effect'. The incretin effect denominates the phenomenon that oral glucose elicits a higher insulin response than does intravenous glucose. The two hormones responsible for the incretin effect, glucosedependent insulinotropic hormone (GIP) and glucagon-like peptide-1 (GLP-1), are secreted after oral glucose loads and augment insulin secretion in response to hyperglycemia. Gastric Inhibitory Polypeptide and Glucagon-Like Peptide-1 in the Pathogenesis of Type 2 Diabetes. Diabetes 53:S190S196, 2004 The investigation of the incretin effect is not usually performed using the same quantity of glucose as in this question. An 'isoglycaemic study' is often used where an infusion of glucose is designed to copy exactly the blood glucose profile generated in an individual or animal by a certain enteral glucose load. Exenatide (synthetic exendin-4) is a new agent for the treatment of Type 2 Diabetes. Exendin-4 occurs naturally in the saliva venom of the North American lizard called the Gila Monster. It mimics the action of the gut hormone GLP-1 (Glucagon-like peptide 1) In which of the following would the first drug be associated with increased pharmacological action of the second drug? (Please select 1 option) Erythromycin : theophylline This is the correct answer Phenytoin : ethinyloestradiol Ranitidine : cortiocosteroid Rifampicin : warfarin Valproate : phenobarbitone Incorrect answer selected Erythromycin would inhibit the metabolism of theophylline. Ranitidine unlike cimetidine is not an enzyme inhibitor. Phenytoin would speed up metabolism of ethinyl-oestradiol making the pill less effective. Rifampicin is a well recognised enzyme inducer. A 24-year-old female presents with a two week history of polyuria and polydipsia together with frequent nocturia. Investigations show Serum Sodium 144 mmol/L (137-144) Serum Potassium 3.3 mmol/L (3.5-4.9) Serum Calcium 2.6 mmol/L (2.2-2.6) Plasma glucose 6.8 mmol/L (3.0-6.0) Serum Osmolality 310 mOsmol/L (275-295) What is the diagnosis? (Please select 1 option) Diabetes Insipidus Diabetes Mellitus Drug abuse This is the correct answer Primary hyperparathyroidism Primary polydipsia Incorrect answer selected This patient has polyuria and polydipsia of relative recent onset and has an elevated plasma osmolality with a high calcium and glucose concentration. These features would be unlikely in DI and are more in keeping with thiazide diuretic abuse - high calcium, glucose and hypokalaemia. Similarly, the serum osmolality would be low in association with primary polydipsia. There may be plenty of variations purely by alteration of the biochemistry of this question in the exam Which term best describes the affinity of a drug for its receptor? (Please select 1 option) Efficacy Intrinsic activity Potency Selectivity This is the correct answer Incorrect answer selected Therapeutic effect Affinity is the measure of the net molecular attraction between a drug (or neurotransmitter or hormone) and its receptor. The receptor's affinity for binding a drug determines the concentration of drug required to form a significant number of drug-receptor complexes. Affinity and intrinsic activity are determinants of potency. Efficacy contributes both to potency and to the maximum effect of the agonist. Efficacy is a measure of the efficiency of the drug–receptor complex in initiating the signal transduction process. A 30-year-old patient with learning difficulties is admitted as a medical emergency. The patient complains of headache, anorexia and vomiting. On examination she is febrile with a temperature of 38°C, pulse 110 bpm and is clinically jaundiced. Investigations reveal: Bilirubin 60 µmol/L (1-22) Albumin 28 g/L (37-49) AST 400 IU/L (5-40) Alkaline Phosphatase 400 IU/L (45-105) Prothrombin time 35 seconds (<14) She was commenced on a new medication within the last three months. Which do you suspect maybe contributing to the presentation? (Please select 1 option) Cabergoline Carbamazepine Lamotrigine Metformin Sodium valproate Correct Sodium valproate can occasionally have an idiosyncratic response leading to severe or even fatal hepatic toxicity. This is more common if the patient has a metabolic or degenerative disorder, organic brain disease or severe seizures associated with mental retardation. Usually this reaction occurs within the first three months of therapy. Carbamazepine can be associated with jaundice occasionally, however the history of mental retardation and short history of drug use point to sodium valproate as the cause. Lamotrigine can disrupt liver function tests (LFTs). Metformin and cabergoline do not affect liver function however caution is advised when using these drugs in patients with hepatic disease. A 22-year-old male is admitted after drinking engine coolant in an apparent suicide attempt after finding his wife in bed with the postman. Investigations reveal: pH 7.1 (7.36-7.44) pO2 15.3 kPa (11.3-12.6) pCO2 3.2 kPa (4.7-6.0) Standard Bicarbonate 2.2 mmol/L (20-28) Serum Calcium 1.82 mmol/L (2.2-2.6) After replacing calcium, which of the following is the most urgent treatment for this man? (Please select 1 option) Alcohol infusion 8.4% bicarbonate infusion Femopizole infusion Correct Gastric lavage Haemodialysis Engine coolant contains ethylene glycol. Ingestion of as little as 30-60ml is capable of causing death. Traditional management of poisoning includes the use of ethanol, with or without hemodialysis. Activated charcoal is not indicated, and gastric lavage may be beneficial only in the first hour after ingestion. However, fomepizole, has recently been approved for use and is a competitive inhibitor of alcohol dehydrogenase. However, it is very expensive and the evidence supporting its use over alcohol is lacking. Also, this patient already has a severe metabolic acidosis. In this circumstance, antidotal therapy to block alcohol dehydrogenase with ethanol or 4-MP alone is insufficient to treat the poisoning. Data suggest that a severe lactic acidosis needs initial correction and in this patient the most appropriate treatment would be IV fluids with bicarbonate to correct the metabolic acidosis. Then haemodialysis is probably required. A 55-year-old woman who has a history of atrial fibrillation and is receiving warfarin and digoxin, informs you that she has been feeling down of late and has been self medicating with St John's Wort that she obtained from a health shop. Which of the following interactions may be expected between St John's Wort and her current medication? (Please select 1 option) INR is likely to be increased INR is likely to be reduced Correct INR is likely to be unaffected There is an increased risk of digoxin toxicity Digoxin concentrations are unlikely to be affected St John's Wort is now commonly taken for depressive symptoms, yet it is a liver enzyme inducer and therefore has interactions with medications typically reducing the efficacy. In this regard, St John's Wort may reduce the efficacy of Warfarin, requiring increased dose to maintain the INR and it may also reduce the efficacy of Digoxin Which of the following drugs interacts with cranberry juice? (Please select 1 option) Amiodarone Digoxin Propranolol Simvastatin Warfarin Correct This is a pathetic question but apparently this theme has been asked in the exam. I suspect that the authors of this paper were the culprits in composing this question. The answer is warfarin. Which of the following antiemetics functions through inhibition of neurokinin (NK)1 receptor? (Please select 1 option) Aprepitant Correct Domperidone Hyoscine Granisteron Ondansetron Aprepitant is a neurokinin receptor blocker used in the prevention of chemotherapy induced nausea. Ondansetron and granisetron are 5HT3 antagonists. Hyoscine is an anticholinergic/antihistaminergic. Domperidone is an antidopaminergic agent. A 53-year-old male is receiving treatment with imatinib for chronic myeloid leukaemia. Which of the following is imatinib? (Please select 1 option) Inhibits p53 Inhibits HER Inhibits guanylate cyclase Inhibits MAP kinase Inhibits tyrosine kinase Correct Imatinib is an inhibitor of tyrosine kinase and is used in the treatment of conditions such as CML and GIST tumours. It inhibits TK on abl proto-oncogene, c-kit and the PDGF-R. In CML, the Philadelphia chromosome leads to a fusion protein of abl with bcr (breakpoint cluster region), termed bcr-abl. As this is now a continuously active tyrosine kinase, imatinib is used to decrease bcr-abl activity. A 53-year-old female with surgically treated acromegaly is receiving treatment with Octreotide therapy due to persistently elevated growth hormone concentrations following surgery. What is the mechanism of action of Octreotide? (Please select 1 option) Inhibition growth hormone receptor Inhibition of dopamine D2 receptor Inhibition of IGF-1 receptor Inhibition of GHRH receptor Stimulation of the somatostatin receptor Correct Octreotide is a somatostatin analogue and directly inhibits growth hormone secretion through interaction with sms receptors. It is also used in the treatment of neuroendocrine tumours such as carcinoid tumours again through interaction with somatostatin receptors A 59-year-old male presents with a three day history of marked muscle aches and weakness. He has ischaemic heart disease for which he takes a number of drugs including simvastatin and has been taking these drugs for a number of years without any problem. On this occasion his CPK confirms a diagnosis of rhabdomyolysis with a level of 4200 iu/l (<200). Which of the following health supplements is he most likely to have taken that would have contributed to the statininduced rhabdomyolysis? (Please select 1 option) Cranberry juice Cod liver oil capsules Ginseng Grapefruit juice Correct Vitamin C Grapefruit juice is well recognised to inhibit statin metabolism thereby potentiating the myotoxicity. In particular, grapefruit juice should be avoided with simvastatin and lovastatin and it also inhibits metabolism of CCB and theophylline A 16-year-old female is admitted after taking an overdose of her mother's propranolol tablets approximately 2 hours ago. On examination she is drowsy and has a pulse of 40 beats per minute with a blood pressure of 80/40 mmHg. She is treated with activated charcoal, IV fluids and IV atropine but her bradycardia and hypotension fail to respond. Which of the following would be the most appropriate next stage in her management? (Please select 1 option) IV adenaline IV amiodarone IV glucagon Correct IV Phenytoin Insertion of temporary pacemaker In those in whom initial atropine is unsuccessful, IV Glucagon is a recommended treatment for betablocker overdose with some evidence indicating improvement in bradycardia and blood pressure. A farmer, on treatment for depression is admitted acutely 1 hour following an intentional overdose of an unidentified substance. On examination he is bradycardic, hypotensive, disorientated, hypersalivating, and has small pupils. He has most likely ingested : (Please select 1 option) Paracetamol A tricyclic anti-depressant Paraquat An organophosphate insectacide Correct Cyanide Hypersalivation and miosis are the specific clues to acetycholine overactivity. Occupational access to organophosphate insectacides. Pupils tend to be dilated with TCA OD. Paracetamol, cyanide, and paraquat shouldn't affect pupils An elderly asthmatic lady on treatment with high dose prednisolone, complains of a 4 week history of right hip pain. She comments that recently she seems to be developing more facial hair and adds that she has also been diagnosed with high blood pressure and diabetes. On examination she is noted to be unable to weight bear on the right side. What is the most likely cause of her hip pain? (Please select 1 option) Avascular necrosis of femoral head Correct Dislocation of the hip joint Fracture neck of femur Gout Osteoarthritis of the hip joint This question simply tests the knowledge of side-effects of corticosteroids (a favourite theme in MRCP 1). The patient has features of hypercortisolism. Obviously, avascular necrosis of femoral head is the cause of her right hip pain. Which of the following statements regarding Antabuse (disulfiram) are correct? (Please select 1 option) Antabuse acts by promoting the metabolism of acetaldehyde Can be used in patients with a history of psychosis in order to limit alcohol excess Can be used to assist abstinence from alcohol in patients with heart disease. Patients using alcohol based perfumes may develop serious reactions Correct Requires regular dose titration once initiated Antabuse inhibits the breakdown of acetaldehyde, which is a major metabolite of alcohol. It is the accumulation of acetaldehyde which causes the flushing, sweating, palpitations, nausea, and vomiting seen in patients taking Antabuse who imbibe alcohol. These reactions may also occur with alcohol based products, for example, perfume. Antabuse is contraindicated in cirrhosis and heart disease, and psychosis is a relative contraindication for its use. A 30-year-old man presents to the Emergency Department with a history of drug overdose. He is known to be repeatedly admitted with similar episodes of self-harm. On this occasion he is drowsy and has prominent hypersalivation. Which of the following agents, found on his person, is the likely cause? (Please select 1 option) Chlormethiazole This is the correct answer Cocaine Dosulepin L-dopa Solvent cannister Incorrect answer selected Hypersalivation is seen with: parasympathomimetic agents insecticides arsenic strychnine chlormethiazole clozapine and others. Solvent abuse may cause an acneiform rash around the buccal cavity. Cocaine abuse leads to hypertension and nasal septum perforation. The other agents are anticholinergic and would cause dry mouth in overdose A 45-year-old obese male with a two year history of type 2 diabetes has recently commenced metformin at a dose of 500 mg twice daily. However, he re-attends clinic and reports numerous gastrointestinal side effects including bloating and flatulence. He is keen to stop metformin and commence an alternative agent. Which of the following drugs is the most appropriate choice? (Please select 1 option) Acarbose Exenatide Insulin Pioglitazone Correct Repaglinide An obese type 2 diabetic patient is almost certain to be insulin resistant. Current guidelines suggest that first line therapy in obese, insulin resistant patients should be an insulin sensitising agent (Bailey C et al. Br J Diabetes Vas Dis 2006; 6: 147-148). Metformin is the drug of choice in this patient therefore. However, in patients intolerant of metformin, the thiazolidinediones rosiglitazone and pioglitazone are licensed for monotherapy for insulin resistant patients. Previously, sulphonylureas, such as gliclazide, would have been advocated in these circumstances, but current opinion favours rosiglitazone and pioglitazone in such a patient. The recent joint ADA / EASD guidelines for treatment in Type 2 diabetics suggests the glitazones are a useful choice where hypoglycaemia is to be avoided. Glitazones increase the risk of congestive heart failure. There is currently controversy over rosiglitazone since some data suggest it is associated with an increased risk of ischaemic heart disease. A 23-year-old footballer was prescribed Ibuprofen by his GP for a sprained ankle. Several hours later he felt very unwell and was passing dark urine. The peripheral blood film shows many schistocytes. The lab results show: Haemoglobin <9 g/dL (13.0-18.0) WBC 7 x109/L (4-11 x109) with normal differentials Platelets 450 x109/L (150-400 x109) Reticulocyte count 5% (0.5-2.4) Bilirubin 40 mol/L (1-22) What is the most likely cause for his presentation? (Please select 1 option) Allergic reaction Autoimmune haemolytic anaemia Incorrect answer selected Glucose-6-phosphate dehydrogenase deficiency This is the correct answer Paroxysmal nocturnal haemoglobinuria Pyruvate kinase deficiency This is a case of intravascular haemolysis with haemoglobinuria. The patient has the history of taking Ibuprofen which is an oxidant and causes hemolysis in patients with G-6-PD deficiency. Oxidative stressors can be infectious agents, drugs, chemicals and certain legumes. In G-6-PD deficient patients, oxidative stress exposes interior sulfhydryl groups that are oxidized and cannot be reduced, leading to irreversible denaturation of the hemoglobin with Heinz body formation. Schistocytes are red blood cell fragments that result from membrane damage. They are sometimes referred to as "bite cells". A 38-year-old male is admitted with an hour history of chest pain, confusion and agitation after taking a recreational drug. On examination, he is confused, has a temperature of 38.3°C and a blood pressure of 188/102 mmHg. Which of the following drugs is most likely to be responsible for his presentation? (Please select 1 option) Cocaine Correct Ecstasy (MDMA) Gamma hydroxybutyrate (GHB) LSD Opiates In this scenario, the young male presents with confusion and agitation following drug abuse. The most likely agent is cocaine. Through central effects, cocaine induces sweating, pyrexia and also adrenergic mediated hypertension. It may also be responsible for coronary and cerebral artery spasm causing infarction. A 72-year-old man presents with painful lumps in his feet and is diagnosed with gout. Following initial treatment with non-steroidal anti-inflammatory agents he is started on allopurinol. How does this work? (Please select 1 option) Increases urinary uric acid excretion Inhibits cyclooxygenase II Inhibits macrophage tubular formation Inhibits nitric oxide synthase Inhibits xanthine oxidase Correct Allopurinol inhibits xanthine oxidase, the enzyme involved in the conversion of purines into uric acid. A 45-year-old female is admitted with fatigue, nausea and weight loss. She is known to have abused alcohol for many years and has previously developed delirium tremens. She stopped drinking alcohol two days ago. On examination, she is thin, alert and orientated. She is slightly icteric, with features of chronic liver disease but there is no flapping tremor. Pulse is 88 bpm regular, blood pressure is 106/74 mmHg and temperature is 37°C. She is treated with IV thiamine. Which of the following agents would be recommended for the prevention of acute alcohol withdrawal? (Please select 1 option) IM haloperidol IV diazepam Oral diazepam This is the correct answer Oral quetiapine No preventative treatment required. Incorrect answer selected This patient with features of alcoholic chronic liver disease would be regarded at high risk of developing acute alcohol withdrawal, particularly in view of her past history of delirium tremens. Benzodiazepines are appropriate agents in preventing acute alcohol withdrawal and oral agents such as lorazepam and diazepam are recommended. A 45-year-old woman has, approximately four hours ago, taken an unknown quantity of amitriptyline tablets that were being prescribed for her depression She is feeling drowsy, agitated and has a dry mouth. An ECG shows wide QRS complexes with arrhythmias. Blood gas analysis revealed: pH 7.2 (7.36-7.44) PaO2 10 KPa (11.3-12.6) PaCO2 4 KPa (4.7-6.0) What is the most appropriate treatment? (Please select 1 option) Activated charcoal Gastric lavage Haemodialysis Intravenous insulin Intravenous sodium bicarbonate Correct There is no specific treatment for tricyclic antidepressant poisoning. 500 ml of 1.26% sodium bicarbonate should be used to treat arrhythmias, hypotension and significant ECG abnormalities to a pH of 7.50 - 7.55 in tricyclic antidepressant overdose even in the absence of acidosis. Which if the following is the mechanism of action of warfarin? (Please select 1 option) Activation of gamma-glutamyl carboxylase Chelation of calcium Inhibition of activated factor X Inhibition of vitamin K epoxide reductase This is the correct answer Inhibition of vitamin K-dependent carboxylase Incorrect answer selected The Vitamin K epoxide is in turn recycled back to Vitamin K and Vitamin K hydroquinone by another enzyme, the vitamin K epoxide reductase (VKOR). Warfarin inhibits epoxide reductase (specifically the VKORC1 subunit), thereby diminishing available vitamin K and Vitamin K hydroquinone in the tissues, which inhibits the carboxylation activity of the glutamyl carboxylase. When this occurs, the coagulation factors are no longer carboxylated at certain glutamic acid residues, and are incapable of binding to the endothelial surface of blood vessels, and are thus biologically inactive. (Wikipedia warfarin) A 45-year-old man with Type 2 Diabetes is being treated with Exenatide. Which of the following would be a recognised adverse effect of his treatment? (Please select 1 option) Hyperglycaemia Hypertension Peripheral oedema Renal impairment Weight loss Incorrect answer selected This is the correct answer Exenatide (synthetic exendin-4) is a new agent for the treatment of Type 2 Diabetes. Exendin-4 occurs naturally in the saliva venom of the North American lizard called the Gila Monster. It mimics the action of the gut hormone GLP-1 (Glucagon-like peptide 1). It causes hypoglycaemia (which is its therapeutic effect) especially when used in combination with oral antidiabetic drugs, weight loss, nausea and other gastrointestinal side effects A 70-year-old man presents with an episode of syncope. On subsequent investigation he is found to have marked postural hypotension. He has been taking felodipine for hypertension for a number of years and he also takes aspirin. On further questioning he appears to have taken up a new healthier lifestyle on his seventieth birthday. Which of the following health supplements is he most likely to have taken that would have contributed to the calcium-channel blocker induced hypotension? (Please select 1 option) Cranberry juice Cod liver oil capsules Ginseng Grapefruit juice Correct Vitamin C Grapefruit juice interacts with drugs. The basis for this interaction has been diligently explored and appears to relate to both flavanoid and nonflavanoid components of grapefruit juice interfering with enterocyte CYP3A4 activity. Of the calcium channel blockers felodipine in particular is affected. Am J Hypertens (2006) 19: 768-73 Which of the following antiemetics functions through antagonism of the 5-hydroxytryptamine 3A receptor? (Please select 1 option) Aprepitant Domperidone Hyoscine Metoclopramide Ondansetron Correct Ondansetron is a serotonin 5-HT3 receptor antagonist used mainly to treat nausea and vomiting following chemotherapy. Its effects are thought to be on both peripheral and central nerves. One part is to reduce the activity of the vagus nerve, which is a nerve that activates the vomiting center in the medulla oblongata, the other is a blockage of serotonin receptors in the chemoreceptor trigger zone. It does not have much effect on vomiting due to motion sickness. This drug does not have any effect on dopamine receptors or muscarinic receptors. Which of the following antiemetics functions as a cholinergic muscarinic antagonist? (Please select 1 option) Aprepitant Domperidone Hyoscine Correct Metoclopramide Ondansetron Scopolamine is named after the genus Scopolia. The name "hyoscine" is from the scientific name for henbane, Hyoscyamus niger. It acts as a competitive antagonist at muscarinic acetylcholine receptors; it is thus classified as an anticholinergic or as an anti-muscarinic drug A 63-year-old female presents with dry mouth of 3 months duration. She is taking medication for hypertension, stress incontinence and reflux oesophagitis. Which of the following may be responsible for her dry mouth? (Please select 1 option) Oxybutinin Correct Doxazosin Hydrallazine Cimetdine Bendroflumethiazide Oxybutinin is an effective treatment for detrussor instability and is a parasympathetic muscarinic antagonist. Consequently dry mouth is a problem in up to 70% of cases. Bendroflumethiazide, the thiazide diuretic, at a dose of 2.5 mg per day is not associated with dry mouth. Cimetdine is a H2 antagonist and is not associated with dry mouth A 63-year-old patient with bipolar disorder and Type 2 diabetes trips over a step and sustains an injury to her left hand. She is unable to dorsiflex her left hand, and an orthopaedic registrar diagnosis a ruptured extensor tendon. She is receiving treatment for an infected diabetic foot ulcer. Which of the following therapies may be implicated in this injury? (Please select 1 option) Aripiprazole Exenatide Fusidic acid Levofloxacin Correct Naproxen The quinolones have recently been associated with tendon rupture. Rupture has been reported in the Achilles, shoulder and hand. This may occur due to disruption of the extracellular matrix and depletion of collagen which is observed in animal models. Aripiprazole is a second generation antipsychotic, and exenatide is a glucagon like-peptide 1 analogue used in the management of Type 2 diabetes. Neither of these products has been associated with tendon rupture. A 40-year-old ex-footballer presents requesting treatment for alcoholism and is prescribed disulfiram. What is the mode of action of disulfiram? (Please select 1 option) Decreases severity of alcohol withdrawal Helps alcoholics to drink safely Inhibits acetaldehyde dehydrogenase activity Correct Inhibits alcohol dehydrogenase activity Reduces the desire for alcohol Alcohol is mainly metabolised in the liver to acetaldehyde by alcohol dehydrogenase. Acetaldehyde is then oxidised to acetate by acetaldehyde dehydrogenase (AcDH). Disulfiram irreversibly inhibits the oxidation of acetaldehyde by competing with the cofactor nicotinamide adenine dinucleotide (NAD) for binding sites on AcDH. The increased acetaldehyde levels are thought to produce the unpleasant side effects associated with acetaldehyde syndrome such as headaches, nausea, flushing, etc. With respect to symptoms of withdrawal related to chronic alcohol use, which of the following statements is correct? (Please select 1 option) Benzodiazepines are ineffective in the treatment of seizuressecondary to alcohol withdrawal, due to cross tolerance withethanol a Type A gamma amino-aminobutyric acid receptor Carbamazepine is as effective as benzodiazepines in the acute treatment of the symptoms of alcohol withdrawal This is the correct answer Phenytoin is an effective treatment for seizures related to alcohol withdrawal Withdrawal reflects enhanced neurotransmission in type A gamma-aminobutyric acid pathways Incorrect answer selected Withdrawal reflects reduced neurotransmission in N-methyl-D-aspartate pathways Carbamazepine at a starting dose of 800 mg per 24 hours has been shown to be as effective as oxazepam in the treatment of acute alcohol withdrawal. Phenytoin is not effective in the treatment of alcohol withdrawal-related seizures. Alcohol withdrawal reflects the damping of neurotransmission through type A gamma-amino-butyric pathways, and enhanced neurotransmission through N-methyl-D-aspartate pathways. For a review see NEJM348:18;1788-90. A 33-year-old woman with a history of alcoholism and self-neglect, presents with an episode of blood streaked vomiting. This is attributed to minor Mallory-Weiss tear. She is admitted to hospital and given an intravenous infusion of 5% dextrose. Her serum potassium concentration is noted the following day to have fallen to 1.9 mmol/L (3.54.9) on admission. What is the likely mechanism for the fall in potassium concentration? (Please select 1 option) Cortisol release in response to stress increasing renal potassium loss Decompensated liver failure causing aldosterone secretion Intracellular re-uptake in response to re-feeding with glucose Correct Metabolic acidosis increasing renal potassium excretion Potassium levels falling following gastric loss in vomiting This neglected person is being fed with dextrose, which will cause an elevation of circulating insulin to maintain glycaemic control. This will consequently drive potassium intracellularly so reducing extracellular potassium concentration. A 32-year-old woman treated with hydrocortisone 10 mg in the morning and 10 mg in the evening for Addison's disease, presents to the clinic with poor compliance. She feels that the hydrocortisone upsets her stomach and wants to switch to enteric coated prednisolone. What would be the appropriate corresponding daily dose of prednisolone? (Please select 1 option) 4mg daily 5mg daily Correct 7mg daily 10mg daily 15mg daily The approximate equivalent glucocorticoid action of prednisolone to hydrocortisone is 4:1. Hence the equivalent dose for 20 mg of hydrocortisone is roughly 5 mg per day of prednisolone. For other glucocorticoid dose conversions try this online glucocorticoid dose calculator A 45-year-old female presents with a six month history of exertional dyspnoea and is diagnosed with pulmonary fibrosis (PF). Over the last one year she has received a variety of medications. Which of the following drugs could be responsible? (Please select 1 option) Dexamethasone Ibuprofen Nalidixic acid Penicillamine Sulphasalazine Correct Sulphasalazine as well as other rheumatology drugs such as gold and methotrexate can cause pulmonary fibrosis. Bleomycin and cyclophosphamide rather than vincristine may be responsible. Corticosteroids are sometimes given as a trial in pulmonary fibrosis. Nalidixic acid is associated with seizures and visual disturbances. However nitrofurantoin is well recognised to cause PF. Other drugs include amiodarone and nitrofurantoin. A 63-year-old man was found collapsed. A department of psychiatry outpatient card was found in his jacket, together with a bottle of procyclidine tablets. He was febrile (38.2°C), conscious but unresponsive to commands. The blood pressure was 160/105 mmHg and there was marked muscle rigidity. What is the most likely diagnosis? (Please select 1 option) Acute catatonic schizophrenia Bacterial meningitis Cerebral malaria Neuroleptic malignant syndrome Correct Procyclidine overdose The symptoms are typical of neuroleptic malignant syndrome (NMS). NMS is characterised by: Fever Muscular rigidity Altered mental status Autonomic dysfunction. Procyclidine is used to treat the Parkinsonian side-effects of neuroleptics; its presence in the patient's pocket implies that he was taking neuroleptics. Signs of procyclidine overdose include: Agitation Confusion Sleeplessness lasting up to 24 hours or more Pupils are dilated and unreactive to light. Visual and auditory hallucinations and tachycardia have also been reported A 90-year-old man with chronic leukaemia presents with gout which his general practitioner treats with Allopurinol. How does Allopurinol prevent the accumulation of uric acid? (Please select 1 option) By competing for its transporter to the kidney By enhancing its solubility By inhibiting purine synthesis Correct By inhibiting pyrimidine synthesis By inhibiting the inflammatory response it causes Allopurinol is a xanthine oxidase inhibitor and is converted by this enzyme to alloxanthine in this form it inhibits the conversion of hypoxanthine to xanthine, and the conversion of xanthine to uric acid. Therefore inhibiting the formation of uric acid. Which of the following cytotoxic agents acts by inhibiting purine synthesis? (Please select 1 option) Bleomycin Cisplatin Doxorubicin Methotrexate Correct Vincristine Methotrexate inhibits purine synthesis. J. Biol. Chem., Vol. 262, Issue 28, 13520-13526, Oct, 1987. The other drugs have different mechanisms of action. Useful therapy for improving fertility in Polycystic ovarian syndrome include (Please select 1 option) Cyproterone acetate Ethinyl oestradiol Metformin Correct Glibenclamide Spironolactone Metformin has been shown to increase the rate of conception in PCOs through improved insulin sensitivity. Ethinyloestradiol and cyproterone acetate combine to form Dianette the oral contraceptive. Spironolactone is used for hirsuitism but is teratogenic. Glibenclamide is not used in PCOs. Oral therapy with which of the following may cause galactorrhoea? (Please select 1 option) Bromocriptine Cabergoline Spironolactone Cimetidine Incorrect answer selected Domperidone This is the correct answer Domperidone is a dopamine antagonist producing large rises in prolactin concentrations. Spironolactone has no effect on prolactin and Cimetidine produces hyperprolactinaemia only when given IV. Both bromocriptine and cabergoline are dopamine agonists and reduce prolactin. A 29-year-old man is starting a chemotherapy regime that includes cisplatin. Which of the following is the mechanism of action of cisplatin? (Please select 1 option) Causes crosslinking in DNA Correct Degrades preformed DNA Inhibits purine synthesis Reduces the formation of microtubules Stabilises DNA-topoisomerase II complex "Cisplatin acts by crosslinking DNA in several different ways, making it impossible for rapidly dividing cells to duplicate their DNA for mitosis." Wikipedia: cisplatin Interferon alpha immunotherapy is used as treatment of which for the following conditions? (Please select 1 option) Acute lymphoblastic leukaemia Acute myeloid leukaemia Burkitt's lymphoma Hairy cell leukaemia Correct Myelodysplastic syndrome "Interferon-alpha is an immune system hormone which is very helpful to a relatively small number of patients, and somewhat helpful to most patients. Most commonly, the drug helps stabilize the disease or produce a slow, minor improvement. The typical dosing schedule injects 3 million units of Interferon-alpha (not pegylated versions) three times a week, although the original protocol began with six months of daily injections." Wikipedia: Hiary Cell Leukaemia A 45-year-old male takes Lithium for a bipolar affective disorder. Which of the following drugs would be contra-indicated in conjunction with Lithium? (Please select 1 option) Atenolol Bendroflumethiazide Codeine Phosphate Correct Flucloxacillin Thyroxine Caution should be exercised when taking Lithium and diuretics as the latter may reduce renal clearance of lithium and increase serum lithium concentrations. NSAIDs also increase Lithium concentrations. Metronidazole, ACEis and Calcium channel blockers also increase serum Lithium concentrations A 26-year-old woman was being treated in the outpatient clinic for autoimmune hypothyroidism. She was taking 150µg of thyroxine and 200 mg of amiodarone. Investigations reveal: Plasma prolactin 654 mU/L (<360) Plasma free T4 24 pmol/L (10-22) Plasma free T3 5.2 pmol/L (5-10) Plasma thyroid-stimulating hormone 68 mU/L (0.4-5) What is the most likely explanation for her high TSH levels? (Please select 1 option) Amiodarone effect Hyperprolactinaemia Poor compliance with medications Correct Thyroid hormone resistance TSH producing pituitary adenoma This young woman has a slightly elevated thyroxine (T4) and an elevated thyroid-stimulating hormone (TSH). The most probable explanation is poor compliance. This also explains the slightly high prolactin concentration too; a consequence of reduced dopaminergic tone on the lactotrophs. The typical scenario is that the patients take their medication in the days before the clinic. This is a classic MRCP question and is highly discriminating. Consider this one carefully and try to understand fully why this is not an effect of amiodarone. A 29-year-old man who is a keen amateur photographer with his own development studio presented to the Emergency department with confusion. His partner said he had been under a great deal of stress recently and she found him foolishly drinking a developer solution with a poison symbol on it. He is hypoxic and hypotensive. The local poisons unit suggests a diagnosis of cyanide poisoning. Which of the following would be the most appropriate treatment? (Please select 1 option) Desferrioxamine Dicobalt EDTA Correct Gastric lavage with Fuller's earth Haemodialysis Penicillamine Potassium ferricyanide is used chiefly for blueprints, in photography, for staining wood, in calico printing, and in electroplating. Kelocyanor (dicobalt EDTA), given by intravenous injection, has been proven to be of use when administered to seriously ill victims of confirmed cyanide poisoning. It is itself toxic, however, and can kill if used wrongly. HSE knows of several cases of inappropriate use resulting in hospital treatment. Its administration is beyond the scope of first aid and a recommendation has been made in the past that a 'Kelocyanor kit' should be kept by users of cyanide and transported to hospital with the patient. Unfortunately we are aware of cases where this has misled doctors to treat patients for cyanide poisoning when this diagnosis was not correct. UK guidelines for the first aid of cyanide poisoning A 24-year-old male presents after developing a bluish discolouration of the body, lips and nails. He denies any relevant past medical history. Examination reveals a central cyanosis and a grey complexion. Investigation revealed: Haemoglobin 17.0 g/dL (13.0-18.0) PaO2 13.0 kPa (11.3-12.6) SaO2 (using an oximeter) 85% (>95) What is the most likely diagnosis? (Please select 1 option) Argyria Cyanotic congenital heart disease Haemochromatosis Methaemoglobinaemia Correct Methylene blue poisoning This patient is otherwise well and has no specific features of congenital heart disease (clubbing etc). He appears desaturated with sats of 85% yet good pO2. This is a typical description of methaemoglobinaemia which is the accumulation of reversibly oxidised methaemoglobin causing reduced oxygen affinity of the Hb molecule with consequent cyanosis. It can occur due to an inherited condition or as a consequence of drugs such as nitrites. Argyria is colloidal silver toxicity. more ... A 48-year-old lady with Addison's disease presented in a small peripheral clinic. She says that she has run out of her hydrocortisone and she usually takes 20 mg in the morning and 10 mg in the evening. No hydrocortisone is available at the clinic but you do have prednisolone which you would like to prescribe instead until a prescription of hydrocortisone can be dispensed. What is the equivalent daily dose of prednisolone? (Please select 1 option) 2.5 mg 5 mg 7.5 mg Correct 10 mg 20 mg 1 mg is equivalent to 4 mg hydrocortisone so this lady should be given 7.5 mg. If 2.5 mg tablets were not available (to go with a 5 mg tablet to make 7.5 mg tablet) then 10 mg would be fine. It is better to overdose rather than under-dose especially where there is stress or illness. A patient is suspected of having taken a substance with anticholinesterase effects. Which of the following combinations of signs, if present, would be the most likely to confirm this effect? (Please select 1 option) Bradycardia and miosis Correct Bradycardia and mydriasis Bradycardia and urinary retention Tachycardia and diarrhoea Tachycardia and lacrimation An Acetylcholinesterase inhibitor or Anti-cholinesterase is a chemical that inhibits the cholinesterase enzyme from breaking down acetylcholine (ACh), so increasing both the level and duration of action of the neurotransmitter acetylcholine. ACh can stimulate postganglionic receptors to produce effects such as salivation, lacrimation, defecation, micturition, sweating, miosis, bradycardia, and bronchospasm. Muscarine produces these effects, and hence they are referred to as muscarinic effects, and the postganglionic receptors are called muscarine receptors. (eMedicine) SLUD (Salivation, Lacrimation, Urination, Defecation [and emesis]) is a syndrome of pathological effects indicative of massive discharge of the parasympathetic nervous system. Unlikely to occur naturally, SLUD is usually encountered only in cases of drug overdose or exposure to nerve gases. Nerve gases irreversibly inhibit the enzyme acetylcholinesterase; this results in a chronically high level of acetylcholine at cholinergic synapses throughout the body, thus chronically stimulating acetylcholine receptors throughout the body. (Wikipedia) A 68-year-old lady with mitral valve disease and atrial fibrillation is taking warfarin. Lately her international normalised (INR) has fallen and the dose of warfarin has had to be increased. Which of the following new treatments may account for this change? (Please select 1 option) Allopurinol Amiodarone Clarithromycin Sertraline St John's wort Correct The metabolism of warfarin has been increased since it is becoming less effective. St John's wort is an enzyme inducer. The other drugs are enzyme inhibitors. A 40-year-old lady presents with a swollen right calf. She has a history of mental health problems and is on a number of medications. Which of the following treatments increases the risk of thromboembolism? (Please select 1 option) Antipsychotics This is the correct answer Benzodiazepines Monoamine oxidase inhibitors Selective serotonin reuptake inhibitors Tricyclic antidepressants Incorrect answer selected The oral contraceptive and antipsychotics are possible causes of thromboembolism. A 70-year-old woman is on multiple medications for various conditions and she is found to have a macrocytic anaemia with a low serum B12. Which of the following medications is a possible cause of the B12 deficiency? (Please select 1 option) Amiodarone Ezetimibe Metformin This is the correct answer Nicotinic acid Sodium valproate Incorrect answer selected Metformin can lead to reduced B12 absorption but this is not usually a clinical problem. "The clinician must be aware of the possibility of metformin-associated B12 deficiency in users who suffer cognitive impairment, peripheral neuropathy, subacute combined degeneration of the cord or anaemia." Age Ageing. 2006 Mar;35(2):200-1 The drug of choice for the treatment of Chlamydia trachomatis infection during pregnancy is: (Please select 1 option) Metronidazole Cephazolin Amoxicillin Correct Tetracycline Clindamycin Chlamydia infection in the non-pregnant state is usually treated with a tetracycline, or with erythromycin. More recently, however, amoxicillin has been found to be as effective as the latter. During pregnancy, tetracycline therapy is contraindicated because of its incorporation into fetal bones and teeth. Thus, of the options listed, amoxicillin is the drug of choice A 55-year-old man on treatment for hypertension, epilepsy and gasto-oesophageal reflux disease presented with an urticarial skin eruption. A drug reaction is suspected since he has recently started a new drug. Which of the following medications is most likely to be responsible? (Please select 1 option) Aspirin Correct Atorvastatin Omeprazole Paracetamol Sodium valproate "Urticaria is one of the most common dermatologic problems seen by primary care physicians and often a source of frustration for patient and physician alike. Pinpointing the cause may be challenging--or impossible--because of the many and varied triggers. "Patients with aspirin sensitivity can present with either mucosal reactions (the aspirin triad of nasal polyposis, sinusitis, and asthma) or cutaneous reactions (urticaria or anaphylaxis)." Postgrad Med 2001;109(2):107-23 A 65-year-old man has locally advanced pancreatic cancer and has been paying privately for treatment with Erlotinib (Tarceva) for the past 9 months. It has worked effectively for that period but a recent CT scan showed further growth in the tumour. Which of the following mechanisms best explains this resistance to treatment with Erlotinib? (Please select 1 option) Development of antibodies to Erlotinib Lack of autophosphorylation at binding site Malabsorption Mutated IGF-1 receptor Correct Reduced expression of EGFR Erlotinib specifically targets the epidermal growth factor receptor tyrosine kinase (which is required for the conformational change) and binds in a reversible fashion to the adenosine triphosphate binding site. For the signal to be transmitted, two members of the EGFR family need to come together to form a homodimer. These then use the molecule of ATP to autophosphorylate each other, which causes a conformational change in their intracellular structure, exposing a further binding site for binding proteins that cause a signal cascade to the nucleus. By inhibiting the ATP, autophosphorylation is not possible and the signal is stopped. A key issue with EGFR-directed treatments is that after a period of 8-12 months, the cancer cells become resistant to the treatment, most commonly by recruiting a mutated IGF-1 receptor to act as one of the EGFR partners in the homodimer, so forming a heterodimer. This allows the signal to be transmitted even in the presence of an EGFR inhibitor. Some IGR-1R inhibitors are in various stages of development (based either around tyrphostins such as AG1024 or AG538 or pyrrolo[2,3-d]pyrimidine derivatives such as NVP-AEW541. You look up a drug in the BNF and note the following against it: What does this signify? (Please select 1 option) Drug is not available on the NHS Prescription only drug Incorrect answer selected Over the counter therapy Report any potential adverse event This is the correct answer Report only potentially serious adverse events The Committee on the Safety of Medicines assigns the inverted black triangle to those relatively new drugs/vaccines or blood products to notify prescriber's that the drug is under surveillance and that all suspected adverse reactions associated with the drug should be reported, typically with a yellow card This symbol appears next to a drug that you have looked up in the BNF: What does this signify? (Please select 1 option) Not available for prescription on the NHS Correct Not recommended for NHS use Only available for specialist use and not for the wider NHS use Over the counter only therapy Specialist licence required for prescription on the NHS This symbol signifies that the drug is not available for NHS prescription but may be available as a private script. What does this symbol signify? (Please select 1 option) Prescribing can be optional and medication can be obtained over the counter Medication only available as prescription by licenced practitioner Intense monitoring required for any adverse events Pharmacist prescribable drug Controlled drug Correct Prescription Only Medicine - POM and can be prescribed only by licensed medical or dental practitioners symbol appears next to a drug in the BNF. What does this signify? (Please select 1 option) A drug less suitable for prescribing Correct A drug that requires closer surveillance for possible side effects Controlled drug Over the counter medication Prescription only therapy This symbol indicates those preparations that are considered by the Joint Formulary Committee to be less suitable for prescribing. Although such preparations may not be considered first choice agents their use may be justifiable under certain circumstances. A type 2 diabetic patient being treated with gliclazide, presents with sweating and dizziness. He is on treatment for hypertension, atrial fibrillation, joint pain and indigestion. Blood glucose was 1.9 mmol/L (3.0-6.0). Which of the following drugs is responsible? (Please select 1 option) Aspirin Atenolol Digoxin Fluconazole Correct Ranitidine Gliclazide is highly bound to plasma proteins, about 94%. Its free plasma level increases on displacement by aspirin given for joint pains. As a result of drug interaction, hypoglycemia may be potentiated when a sulfonylurea is used concurrently with agents such as: long-acting sulfonamides, tuberculostatics, phenylbutazone, clofibrate, MAO inhibitors, coumarin derivatives, salicylates, probenecid, propranolol, cimetidine, disopyramide and angiotensin converting enzyme inhibitors. Plasma protein binding of fluconazole is low and its excreted by kidney. Gliclazide is a sulphonylurea drug with an intermediate half-life of around 11 hours. It is extensively metabolised within the liver by CYP2C9. Renal clearance accounts for only 4% of total drug clearance. As fluconazole is a potent inhibitor of CYP2C8 and CYP2C9, it may also interact with the sulphonylureas (eg. glimepiride and gliclazide). Thus the best answer in this scenario would be likely to be Fluconazole. A 45-year-old female with chronic schizophrenia was recently converted to a new anti-psychotic agent. She presented two weeks later with a sore throat and fever. Her full blood count shows: Haemoglobin 12.5 g/dL (11.5-16.5) White cell count 1.3 x109/L (4-11 x109) Platelets 135 x109/L (150-400 x109) What drug is she likely to have commenced? (Please select 1 option) Clozapine Correct Haloperidol Olanzapine Quetiapine Risperidone Unlike the other newer antipsychotic agents, clozapine is associated with agranulocytosis in approximately 1-2% of patients. The mechanism through which this happens remains unclear A 59-year-old male type 2 diabetic is attending the foot clinic regularly. He has a neuropathic ulcer complicated by osteomyelitis a deep wound swab has grown Staphylococcus aureus and E coli. He also takes warfarin for atrial fibirillation. Which of the following antibiotics will reduce the anticoagulant effect of Warfarin? (Please select 1 option) Ciprofloxacin Co-trimoxazole Erythromycin Metronidazole Rifampicin Correct The anticoagulant effect of warfarin can be affected by drugs, which induce or inhibit the action of enzymes involved in the metabolism of warfarin. Rifampicin is known to induce the action of such enzymes therefore increasing the metabolism of warfarin so reducing its anticoagulant effect. Erythromycin and ciprofloxacin inhibit the effect of these enzymes therefore enhancing the anticoagulant effect of warfarin. Metronidazole and Co-trimoxazole inhibit the clearance of the active S isomer of warfarin therefore enhancing its anticoagulant effect. A 30-year-old male presented with a paranoid psychosis accompanied by visual hallucinations which resolved over the next three days. Which one of the following is the most likely diagnosis? (Please select 1 option) Alcohol withdrawal. Correct Diazepam dependence. Fluoxetine overdose. Heroin withdrawal. Smoking cannabis. The paranoid psychosis with visual hallucinations is highly suggestive of delirium tremens - alcohol withdrawal Folic acid metabolism can be affected by (Please select 1 option) tetracycline pyrimethamine Correct vitamin B12 penicillin brufen Drugs which inhibit dihydrofolate reductase = methotrexate, pyrimethamine and trimethoprim. Drugs which interfere with absorption/storage of folate = phenytoin, primidone, oral contraceptives Galactorrhea + hyperPL => DA antagonist [maxolon, domperidone] A 30 year-old female presents with a one year history of galactorrhoea. She has been receiving treatment for hay fever, depression, obesity and dyspepsia. Her investigations reveal: Full Blood Count Normal Urea and electrolytes Normal Prolactin 820 mU/L (<360) Free thyroxine (T4) 18.3 pmol/L (10-22) TSH concentration 2.1 mU/L (0.4-5) Which one of the following drugs is most likely to explain these findings? (Please select 1 option) Astemizole Metoclopramide Correct Paroxetine Ranitidine Sibutramine Although the SSRIs are also rarely associated with hyperprolactinaemia, the answer has to be Metoclopramide which is a dopamine antagonist that is typically associated with hyperprolactinaemia. A firm 2-3 cm mass is palpable in the upper outer quadrant of the right breast of a 52year-old woman. There are no palpable axillary lymph nodes. A lumpectomy with axillary node dissection is performed and the breast lesion is found to have positive immunohistochemical staining for HER2/neu (c-erb B2). Staining for oestrogen and progesterone receptors is negative. Which of the following additional treatment options is most appropriate, based upon these findings? (Please select 1 option) Radical mastectomy St John's wort Tamoxifen Trastuzumab Correct Vancomycin This is an infiltrating ductal carcinoma. The lack of oestrogen receptor staining suggests a poor response to hormonal therapy with tamoxifen. The positive C-erb B2 (HER2/neu) staining suggests that trastuzumab (Herceptin) may be effective. A 52-year-old woman who complains of exertional breathlessness presents to the clinic as she is desperate to stop smoking. She has had a number of unsuccessful attempts to stop smoking over the years and has tried nicotine patches. Which of the following would be an appropriate choice to assist in her attempts at smoking cessation? (Please select 1 option) Acupuncture Hypnotism Nicotine gum Nortriptyline Varenicline Correct Varenicline (Champix) is an oral anti-smoking agent with dual action, reducing the craving for cigarettes and also making the smoking of cigarettes less pleasurable. ASH, Action on Smoking and Health have released guidance on its use. It appears to be effective and safe with the main side effect being nausea. Varenicline appears to be more effective in clinical trials than either bupropion or placebo and is prescribed for 12 weeks in the first instance with further 12 week course if craving still persists A 48-year-old lady with a history of epilepsy and ischaemic heart disease presented with the following Full Blood Count. Haemoglobin 7.4 g/dL (11.5 - 16.5) Mean cell volume 125 fL (80 - 96) White cell count 2.5 x 10 9/L (4 - 11) Platelet count 130 x 10 9/L (150 - 400) Which of the following medications is the most likely cause? (Please select 1 option) Carbamazepine Clopidogrel Furosemide Phenytoin Correct Spironolactone There is a macrocytic anaemia with low platelets and WCC typical of a nutritional deficiency. Phenytoin can lead to folate deficiency and is therefore the most likely cause With regard to poisoning / overdose: (Please select 1 option) Phenobarbitone causes a metabolic acidosis Ethylene glycol causes a metabolic alkalosis and renal failure Aspirin causes acidosis due to hypoventilation Methanol causes a metabolic acidosis with an increased anion gap Correct Chlormethiazole causes hyperthermia and hypertension Aspirin causes hyperventilation which may result in a respiratory alkalosis; massive overdose may cause a metabolic acidosis. Phenobarbitone and chlormethiazole both suppress the central nervous system causing hypoventilation, hypotension and hypothermia. Ethylene glycol causes a metabolic acidosis. Methanol is metabolised to formaldehyde and formic acid An 18-year-old Asian female is noted to have gingival hypertrophy by her dentist. Which of the following is most likely to be responsible for her presentation? (Please select 1 option) Carbamazepine Scurvy Lead poisoning Phenytoin Correct Sodium valproate The inclusion of 'Asian' descent in this question is intended as a distractor. Gum hypertrophy may be seen in conditions such as acute myeloid leukaemias and with drugs such as phenytoin. Scurvy (vitamin C deficiency) is associated with bleeding gums. Lead toxicity is associated with pigmentation of the gingiva. Carbamazepine is not associated with gingival hyperplasia but recognised side effects include ataxia, drowsiness and blood dyscrasias. Which of the following reactions is involved in the metabolism of paracetamol under normal conditions? (Please select 1 option) Acetylation Conjugation to glucuronic acid Correct Conjugation to glutathione Cytochrome p450 dependent oxidation Hydrolysis Paracetamol is conjugated to glucuronic acid and sulphate under normal conditions. In overdose these processes become saturated and the drug is then conjugated with glutathione. If the glutathione supply is depleted then a toxic metabolite is formed Which of the following doses of prednisolone is equivalent in its glucocorticoid potency to 20mg of hydrocortisone? (Please select 1 option) 2 mg 5 mg Correct 10 mg 15 mg 20 mg It is important to know the relative potencies of the glucocorticoids. Dexamethasone for instance is roughly 30 times more potent than hydrocortisone In which of the following have randomised controlled trials shown that long-term oxygen therapy (LTOT) reduces mortality? (Please select 1 option) Asthma Cor pulmonale due to chronic airflow obstruction Correct Cryptogenic fibrosing alveolitis Cystic fibrosis Pulmonary sarcoidosis Adequate data for LTOT prolonging survival exists only for chronic obstructive pulmonary disease (COPD) although in practice it is assumed to apply in other chronic hypoxaemic lung conditions. A 35-year-old woman with known seafood allergy presented after developing an itchy rash at a restaurant. She had widespread urticaria which spared her neck and face. On examination, her blood pressure is 130/70 mmHg, pulse 95 bpm, respiratory rate 24/min and O2 saturation 99% on air. Intravenous hydrocortisone and intramuscular antihistamine have been given. What is the next most appropriate step in the management of this patient? (Please select 1 option) Inhaled adrenaline Intramuscular adrenaline Incorrect answer selected Intravenous adrenaline Observe This is the correct answer Subcutaneous adrenaline Where there is a history of a typical allergic reaction as here current United Kingdom resuscitation guidelines suggest adrenaline if there is: stridor wheeze respiratory distress or clinical evidence of shock. A literature review in the BMJ includes a copy of the algorithm and a discussion of the evidence for adrenaline. BMJ 2003;327:1332-1335 An overweight, 60-year-old female with an eight year history of Type 2 diabetes mellitus presents with deteriorating glycaemic control. She takes gliclazide 160 mg twice daily. Investigations reveal: Sodium and potassium Normal Serum urea 10 mmol/L (2.5-7.5) Serum creatinine 160 µmol/L (60-110) Serum alanine transaminase 31 U/L (5-35) Serum aspartate transferase 30 U/L (1-31) HbA1C 9.0% (3.8-6.4) Which of the following would be the most appropriate additional therapy for improved glycaemic control? (Please select 1 option) Acarbose Guar gum Metformin Repaglinide Incorrect answer selected Rosiglitazone This is the correct answer This woman with diabetes has poor glycaemic control with renal impairment. With creatinine concentrations above 150 µmol/L, metformin is not recommended due to the small risk of lactic acidosis. Therefore, the most appropriate treatment as recommended by NICE would be rosiglitazone as liver function tests are normal and there is no suggestion of heart failure. Acarbose is poorly tolerated and is now rarely prescribed. Guar gum has little place in the treatment of diabetes. Repaglinide the non-sulphonylurea insulin secretagogue would have little benefit in conjunction with a traditional SU such as gliclazide. The following are causes of drug induced hepatitis except: (Please select 1 option) Amiodarone Ethambutol Correct Isoniazid Methyldopa Pyrazinamide Side effects of ethambutol are largely confined to visual disturbances in form of loss of acuity, colour blindness and restriction of visual fields. It does not cause hepatitis and is renally excreted. Isoniazid, amiodarone, pyrazinamide and methlydopa are a cause of drug induced hepatitis. A 48-year-old man is admitted with nausea and excessive drowsiness after taking an antihistamine tablet. He has previously used the antihistamine but on this occasion he has recently been drinking large amounts of grapefruit juice for his health. Grapefruit juice is suspected of causing a drug interaction in this man. Which of the following liver enzyme systems is affected by grapefruit juice? (Please select 1 option) Cytochrome p450 3A4 Correct Glycine decarboxylase Glucuronidation Glutathione S-transferase Sulfation Bergamottin is a constituent of grapefruit juice and is metabolised by the Cytochrome p450 3A4 pathway. A youth worker, aged 40, presents to the Emergency Department with vomiting. On detailed questioning, he states that he has taken about 36 paracetamol tablets two hours previously. He is vomiting profusely with a blood pressure of 90/60 mmHg. Which of the following measures would be the most appropriate immediate step in the management of this patient? (Please select 1 option) Coagulation screen IV fluids Correct IV N-acetyl cysteine Oral methionone Paracetamol levels The most pressing issue in this patient is resuscitation as he is vomiting and is hypotensive. It is unusual to see such hypotension in paracetamol overdose but is feasible in a massive overdose and usually associated with lactic acidosis. It is too early to carry out paracetamol levels as these should be carried out at four hours. Although he states that he has taken 18 g of paracetamol this may NOT be the case and he may not require N-acetyl cysteine. You can wait. In fact the benefit of N-acetyl cysteine is maximum as long as it is given within eight hours of ingestion. Its benefit extends up to 24 hours. An elevated international normalised ratio (INR) gives an indication of hepatocellular damage and again this will not be seen at presentation of paracetamol overdose. Further reading: Emergency treatment of paracetamol poisoning. British National Formulary. BNF 56. Daly FFS, Fountain JS, Murray L, Graudins A, Buckley NA. Guidelines for the management of paracetamol poisoning in Australia and New Zealand - explanation and elaboration; consensus statement from clinical toxicologists consulting to the Australasian poisons information centres. MJA 2008; 188 (5): 296-302 The antibiotic combination quinupristin and dalfopristin are: (Please select 1 option) Administered orally. Effective against multi-resistant Staph. aureus Correct Effective against resistant mycobacterium TB. Indicated in subjects with chronic renal impairment. Particularly effective in the treatment of pseudomonas infection in cystic fibrosis. Quinupristin and dalfopristin are a synergistic combination of a streptogramin A and B respectively. They are effective against gram positive aerobes and are particularly useful against resistant Strep. pneumoniae and Staph. aureus. They can be administered only via a central line A 17-year-old female presents with three headaches over a six month period. She describes the headaches as severe, right-sided and lasting for twelve hours and associated with nausea and photophobia. Each is preceded by spots before her eyes. What is the most appropriate initial treatment for this patient? (Please select 1 option) Diclofenac at the onset of the next attack Ergotamine suppository at the onset of the next attack Paracetamol plus metoclopramide at the onset of the next attack Correct Prophylaxis with propranolol Sumatriptan at the onset of the next attack First line treatment of acute migraine consists of simple analgesic (either soluble paracetamol or aspirin) and an antiemetic (usually domperidone or metoclopramide). Second line treatment includes the use of non-steroidal anti-inflammatory drugs such as diclofenac. If the above measures fail to alleviate the attacks, then triptan therapy (for example, sumatriptan) is indicated. It is important for patients to take the treatment as early as possible. Long-term prophylaxis with drugs (for example, propranolol) is only indicated if the attacks are frequent (more than two a month). A 42-year-old man presented with confusion following a seizure. He has a history of epilepsy and is also known to the community psychiatry team. Examination reveals that he has a temperature of 37°C, BP 138/84 mmHG, coarse tremor and a pulse of 90 bpm. Which of the following is the most likely underlying diagnosis? (Please select 1 option) Benzodiazepine overdose Carbamazepine toxicity Lithium toxicity Correct Neuroleptic malignant syndrome Tricyclic overdose The tremor, seizure and confusion should raise the possibility of lithium toxicity which is the condition that best fits this clinical picture. A 57-year-old man attends the outpatient clinic. He has been a Type 2 diabetic for 7 years having been diagnosed following after an acute myocardial infarction at 50 years of age. His diabetes was deteriorating with blood glucose readings of 9-12 at home despite following a diet and taking regular exercise. Another practitioner commenced him on Rosiglitazone. His current treatment is Metformin 850 tds, Rosiglitazone 4 mg, Aspirin 75 mg/day, Carvedilol 12.5 mg bd, Ramipril 10 mg od, Furosemide 80 mg daily, Simvastatin 40 mg/day. On examination he is overweight with a BMI of 29, his BP is 128/74 mmHg with pulse rate of 63 min-1. He has no heart murmurs and there is some pitting oedema in the lower limbs. Auscultation reveals a clear chest with no evidence of pulmonary oedema. He is obese with no organomegaly. His ECG shows sinus rhythm with poor r wave progression. His Hba1c checked in the clinic is 8.5% (3.8-6.4). What is the most appropriate way to treat his glycaemic control? (Please select 1 option) Add Gliclazide 80mg bd Increase Rosiglitazone to 8mg daily Stop metformin and use Avandamet (combination of Metformin and Rosiglitazone) Substitute Rosiglitazone with Glilazide 80mg bd Correct Substitute Rosiglitazone with Pioglitazone 15mg daily This patient is likely to be insulin resistant; however there is evidence of heart failure and fluid overload, so use of thiazolinediones (Rosiglitazone or Pioglitazone) are absolutely contraindicated. These drugs promote fluid retention by means of an action on the collecting ducts of the kidney so promoting sodium and water retention. The only appropriate action therefore is to stop Rosiglitazone, substituting this with the insulin secretagogue gliclazide which will hopefully improve his glycaemic control. A 52-year-old accountant presents with a five hour history of confusion and agitation. He is known to have an alcohol problem but has avoided all alcohol for the last three days. On examination, he is sweating, is agitated and disorientated. His temperature is 37.5°C, pulse 110 bpm regular and blood pressure is 152/74 mmHg. He claims to see things on the walls. His investigations reveal: FBC Normal U+Es Normal Plasma glucose 4.6 mmol/l (3.6-6) Which of the following agents would be the most appropriate treatment for this man? (Please select 1 option) IV Haloperidol IV Lorazepam This is the correct answer IV Phenytoin IV Phenobarbital Oral diazepam Incorrect answer selected This is a typical history of delirium tremens (DTs). Patients with chronic alcohol dependency typically develop withdrawal symptoms two to three days following abstinence from alcohol. Features of: - clouding of consciousness - visual hallucinations - diaphoresis - pyrexia and - hypertension are typical and it is important to maintain adequate hydration. Parenteral benzodiazepines are the treatment of choice for delirium tremens and include diazepam, lorazepam, chlordiazepoxide and midazolam. Which one of the following concerning insulin is correct? (Please select 1 option) Acts via a similar mechanism to steroid receptors Can be detected in the lymph Correct Causes an increased glucose-protein transport on the endoplasmic reticulum Interacts with the nuclear membrane Is synthesised in the alpha cells of Islets of Langerhans Insulin acts via cell surface receptors. Insulin binding to its receptor results in receptor autophosphorylation on tyrosine residues and the tyrosine phosphorylation of insulin receptor substrates (IRS-1, IRS-2 and IRS-3) by the insulin receptor tyrosine kinase. Insulin is synthesised in the beta cells of the Islets of Langerhans not the alpha cells A 58-year-old woman presents with early features of COPD. She is a heavy smoker and asks about drugs that may help her to stop smoking. In particular, she has heard about a new drug that is now available called Champix (varenicline). Varenicline is an agent used in the treatment of smokers to help them quit. Which of the following best describes its mechanism of action? (Please select 1 option) A tricyclic antidepressant with mostly noradrenergic properties An a2-noradrenergic agonist that suppresses sympathetic activity Is a nicotine replacement therapy Is a partial agonist of the alpha4beta2 nicotinic receptor Correct Reduces uptake of dopamine, serotonin and norepinephrine There are now many therapies that have been investigated for use in smoking cessation. Newer drugs are becoming available that have been sepecifically developed for smoking cessation. Varenicline is one of them. Nicotine is a simulant and releases dopamine in the brain that leads to addictive effects of smoking. Its effects can be replaced in other ways using nicotine replacement therapy and this reduces the addiction to cigarette smoking. Bupropion (Zyban) reduces the neuronal uptake of dopamine, serotonin and norepinephrine. Clonidine, a second line agent in smoking cessation because of its side effects, is an a2noradrenergic agonist that suppresses sympathetic activity. Nortriptyline is a tricyclic antidepressant with mostly noradrenergic properties and is an agent that appears to be effective. Varenicline is a non-nicotine drug that is a partial agonist of the alpha4beta2 nicotinic receptor. Further reading: Int J Clin Pract. 2006 May;60(5):571-6 (Review) JAMA. 2006 Jul 5;296(1):47-55 (trial vs. bupropion and placebo) Royal College of Physicians publication on smoking cessation Other news articles on Varenicline In considering the management of convulsions select the correct statement from the list below. (Please select 1 option) Hypoglycaemia should always be considered. Correct If the fit lasts longer than five minutes, then PR diazepam should be given. Paraldehyde is best given intramuscularly. Phenobarbitone is a useful therapy in school age children. When associated with fever, antibiotics should always be given to cover the possibility of meningitis. Status epilepticus is defined as continuous convulsion lasting longer than 30 minutes, or the occurrence of serial convulsions between which there is no return of consciousness. It may be generalised (tonic clonic, absent) or partial (simple, complex, or with secondary generalisation). Generalised tonic clonic seizures predominate. There are 3 major sub-types: Prolonged febrile seizures. Idiopathic status epilepticus (no underlying central nervous system [CNS] lesion or insult). Symptomatic (long-standing neurological disorder or metabolic abnormality). The most common cause in a child less than 3 years is a prolonged febrile seizure. Sleep deprivation and drug withdrawal can also precipitate it. The relationship between neurological outcome and duration of status epilepticus is unknown in children and adults. In the animal model, 60 minutes of constant seizure activity is associated with pathological changes, even when metabolic homeostasis is maintained. Cell death thus results in increased metabolic demands from continually discharging neurones. Vulnerable areas include the hippocampus, the mid to low cerebellum, middle cortical areas, and thalamus. Approximately 20 minutes of status epilepticus produces regional oxygen sufficiency deficiency promoting cell damage and necrosis. This is, therefore, used as the threshold in children. Initial management begins with ABC. Hypoglycaemia should be excluded (if present 5ml/kg of 10% dextrose is given by IV infusion), and blood obtained for full blood count, electrolytes including calcium and magnesium, glucose, creatinine, anticonvulsant levels. Blood and urine may be obtained for toxicology. Arterial blood gases should be done, and consideration given to lumbar puncture. First line anticonvulsant therapy would be Lorazepam/Diazepam given IV if possible. If seizures persist then phenytoin may be given as a loading dose followed by an infusion. Phenobarbitone may be used as first line in infants. Paraldehyde can be given as a dilute solution intravenously, or administered rectally or IM. The latter two routes can produce tissue damage and sloughing, so these should be reserved for exceptional circumstances. To which of the following drug classes do the oral hypoglycaemic agents, rosiglitazone and pioglitazone belong? (Please select 1 option) A peroxisome proliferator activating receptor (PPAR)-alpha agonist A peroxisome proliferator activating receptor (PPAR)-gamma agonist Correct A sulphonylurea A biguanide An alpha-glucosidase inhibitor Rosi- and pio- glitazone belong to a new class of oral hypoglycaemic agents - PPAR gamma agonists. Through activation of this receptor they modulate adipocyte function and improve insulin sensitivity An adolescent boy presents with unexplained neurological illness. Which one of the following would suggest substance abuse? (Please select 1 option) A history of attention deficit disorder. A history of family conflict. A history of low self-esteem. A history of social isolation. Deposits around the mouth. Correct An increasing number of adolescents are experimenting with alcohol, drugs and solvents, usually soon after entering secondary school. Unfortunately, this includes a rising number of young girls smoking. Factors associated with drug use include low self-esteem, social isolation, depression, family conflicts and other conduct disorders. Presentations suggestive of substance abuse include altered behaviour, sniffer's rash, injection sites, chronic upper respiratory tract infection, irregular pulse, glue stains on the skin or clothes, and acute intoxication - ataxia, coma, respiratory depression and cardiac arrhythmia. The only specific thing indicating substance abuse in this case is, therefore, the deposits presumably of glue around the mouth. Sniffer's rash consists of inflammation and ulceration around the mouth and nose