Pathology (Gallbladder) Case 1 An obese 51 year old woman
advertisement
Pathology (Gallbladder)
Case 1
An obese 51 year old woman presented to emergency with an 8 hour history of severe upper
abdominal pain whcih radiated around to her back and was associated with nausea and
vomiting. Upon examination she was mildly jaundiced, and distressed by the pain, with
tachycardia, fever and tenderness in the right upper quadrant of the abdomen. She had a
past history of episodic epigastric pain which was accompanined by jaundice.
Initial clinical symptoms suggested some form of obstruction (with the upper
abdominal pain), infection (fever, tenderness and tachcardia), the prescence of gallstones
(from episodic epigastric pain with accompanying jaundice), jaundice (due to gallstones
blocking the biliary tree – usually the common bile duct [choledocholethiasis]), and nausea
and vomiting. {Symptoms of choledocholethiasis include, pale stools, darker urine, and
biliary colic.} The presenting infection may be due to the inflammation of the gallbladder
(cholecystitis) or inflammation of the biliary tree (choleangitis).
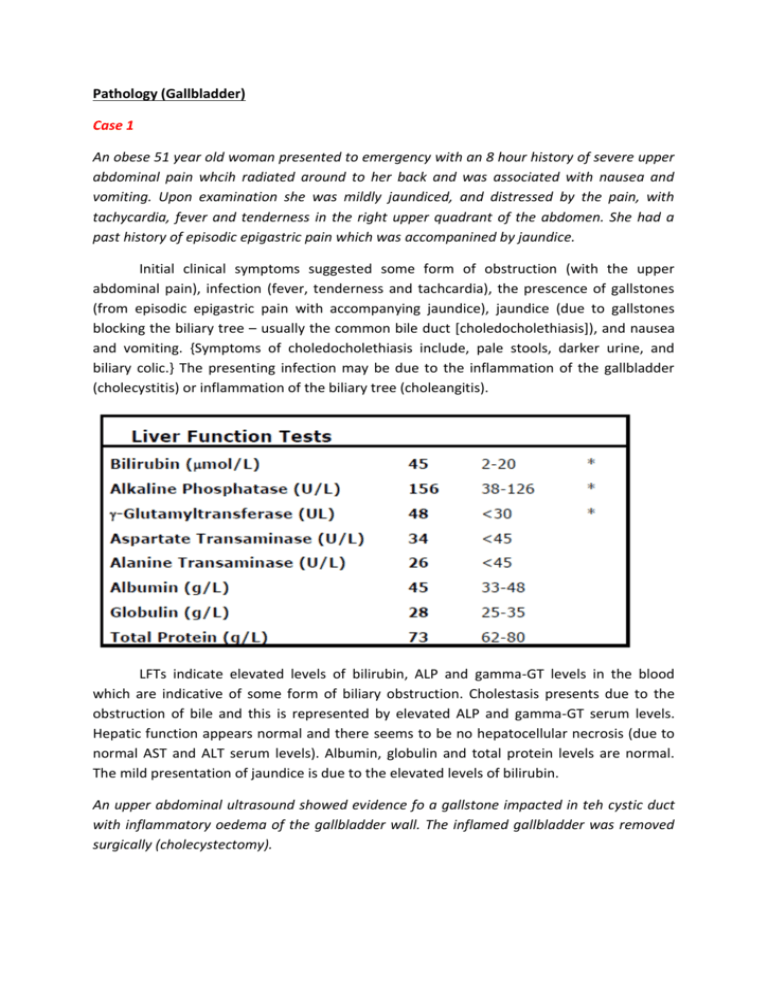
LFTs indicate elevated levels of bilirubin, ALP and gamma-GT levels in the blood
which are indicative of some form of biliary obstruction. Cholestasis presents due to the
obstruction of bile and this is represented by elevated ALP and gamma-GT serum levels.
Hepatic function appears normal and there seems to be no hepatocellular necrosis (due to
normal AST and ALT serum levels). Albumin, globulin and total protein levels are normal.
The mild presentation of jaundice is due to the elevated levels of bilirubin.
An upper abdominal ultrasound showed evidence fo a gallstone impacted in teh cystic duct
with inflammatory oedema of the gallbladder wall. The inflamed gallbladder was removed
surgically (cholecystectomy).
Pathology – Acute Cholecystitis
Acute Cholecystitis – H+E – Low Power
Acute Cholecystitis – H+E – Medium Power
Acute Cholecystitis – H+E – High Power
On low power, the wall of the gallbladder is much thicker. The muscle layer is much
less distinct, and the staining is much more eosinophilic. The epithelial lining is much less
structured and is incomplete at the site of inflammatory response. This epithelium has thus
been ulcerated. The ulceration has penetrated from the epithelium, throught the submucos,
through the muscularis mucosae and straight into the adventitia. Obvious signs of muscle
necrosis is present. Classical signs of acute inflammation are present: infiltration of PMNs,
proteinous (fibrinous) exudate, slight haemorrhage, necrosis, dilated blood vessel and pus
amongst a large area of ulceration.
Previous inflammatory response is determined by the lyphoid aggregation which is a
sign of chronic inflammation indicating previous inflammatory response. Muscle
hypertrophy is another sign of chronic cholecystitis due to previous damage to the
muscularis layer from chronic inflammation.
Macroscopic Appearance: This specimen shows a gallbladder with a thickened, fibrotic wall
(indicative of chronic inflammation), with a gallstone obstructing the gallbladder outlet
(cystic duct). This has resulted in acute inflammation of the gallbladder (cholecystitis), with
pus filling the organ (empyema).
Complications
Gallstones are extremely common in Western society. By far the commonest type of
gallstones are the so-called mixed stones. These stones are multiple, 1-3 cm in diameter.
They may be round, or have faceted surfaces. They are composed largely of cholesterol. Risk
factors include increased cholesterol in bile, which is associated with increasing age; female
gender; obesity; racial and genetic factors; high fat diet; diseases associated with elevated
circulating levels of cholesterol, including diabetes mellitus and some forms of
hyperlipidaemia.
Complications of gallstones include:
1) Recurrent pain in the right upper quadrant of the abdomen (as in this case), known as
"biliary colic". This is caused by passage of stones along the gallbladder outlet (cystic duct)
and the common bile duct.
2) Obstruction of:
a) The cystic duct or neck of the gallbladder to cause acute and chronic cholecystitis (as in
this case);
b) The common bile duct, causing obstructive jaundice;
c) The Ampulla of Vater (where the common bile duct and pancreatic duct empty into the
duodenum), resulting in pancreatitis.
3) Secondary bacterial infection, leading to:
a) Empyema of the gallbladder;
b) Gangrene of the gallbladder wall;
c) Perforation (rupture) leading to peritonitis;
d) Inflammation of the bile ducts caused by obstruction of the common bile duct - ascending
cholangitis;
e) Septicaemia
4) Carcinoma of gallbladder. This is a rare cancer, with most cases occurring in patients with
gallstones.
Case 2
A 59 year old male presented to his local medical officer complaining of weakness, tiredness
and increasing abdominal distension. He consumed more than 100 grams of alcohol per day.
Examination revealed a man who looked older than his stated age. He noted to be pale and
have tense ascites. The liver and spleen were not palpable.
Many visceral organs including the brain, liver, stomach, spleen and pancreas may be
all affected with this man’s alcohol (massive amounts) intake. Ascites is formed due to
decresed serum protein levels. With decresed serum proteins, the colloid osmotic pressure
decreases which is necessary to maintain fluid within the cells. A decrease in colloid osmotic
pressure results in fluid leaking into the interstitial space resulting oedema. Ascites is just
the build-up of fluid in the abdominal cavity. As a consequence, the patient’s spleen and
liver cannot be palpated mainly due the massive swelling that ascites brings.
LFTs indicate slightly elevated bilirubin levels which are indicative of the effects of
jaundice.
Elevated levels of ALP and gamma-GT levels are indicative of either obstruction or
the effects of drugs (including alcohol) which is the case. The consumption of 100g of
alcohol is the likely factor in this case.
ALT and AST levels are slightly elevated which indicate slight levels of necrotic
hepatocytes.
Decreased albumin levels are indicative of reduced ability of albumin synthesis which
occurs in the liver. Protein malnutrition may also be a cause of decreased serum albumin.
Decreased albumin is the cause of ascites due to the reduced colloid osmotic pressure which
normally keeps vessel fluid within vessels. With decreased albumin, fluid is able to leak into
the interstitial spaces leading to ascites (abdominal fluid).
Coagulation protein levels will also be decreased leading to increased prothrombin
times. This is because of decreased hepatic function
The presentation is classical with liver cirrhosis.
While in hospital the man’s acites diminished and he was discharged home. 2 weeks later he
presented in the emergency room with massive haematemesis. Attempts at resusitation
were unsucessful.
Pathology – Liver Cirrhosis
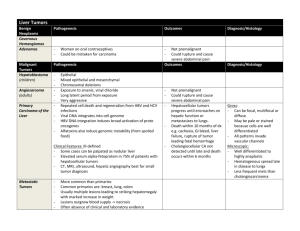
Cirrhosis is the final common pathway for a number of chronic hepatic diseases. The most
common causes in our society are
- alcohol
- chronic viral hepatitis (HBV and particularly HCV)
- chronic biliary obstruction eg. primary biliary cirrhosis
- metabolic disorders eg. haemochromatosis
- cryptogenic (some of these might be related to non-alcoholic fatty liver disease)
Liver Cirrhosis – Medium Power
Liver Cirrhosis – High Power
Liver Cirrhosis – Very High Power – nodular regeneration
Liver Cirrhosis – Very High Power – internodular septa
The fibrous septa are composed of dense, eosinophilic, collagenous bands, and are characteristic of
cirrhosis. The key pathogenic processes in cirrhosis are hepatocyte death, extracellular matrix deposition, and
vascular reorganisation. Proliferation and activation of hepatic stellate cells are primarily responsible for the
fibrosis. As the disease progresses, bridging fibrous bands link portal tracts to portal tracts, and portal tracts to
hepatic veins. The fibrous bands surround nodules of hepatocytes, which undergo regeneration.
In cirrhosis, there is intrahepatic obstruction of biliary outflow. This induces proliferation of ductular
epithelial cells, forming twisted cords of ductules in portal areas. Surviving hepatocytes proliferate and are
arranged in multiple layers rather than single plates of cells. The eosinophilic material surrounding the nodule
is fibrous tissue, containing blood vessels and lymphocytes.
Perisinusoidal fibrosis directly increases resistance to flow in the portal venous system, thereby
contributing to portal hypertension. Obstruction of hepatic veins contributes to portal hypertension in settings
other than cirrhosis (eg. Budd-Chiari syndrome). Biliary ductular proliferation has no effect on portal venous
flow. Hepatic arteriolar disease is not implicated in cirrhosis, and therefore would not contribute to portal
venous hypertension.