Cancer Screening Tests and Clinical Trials
advertisement
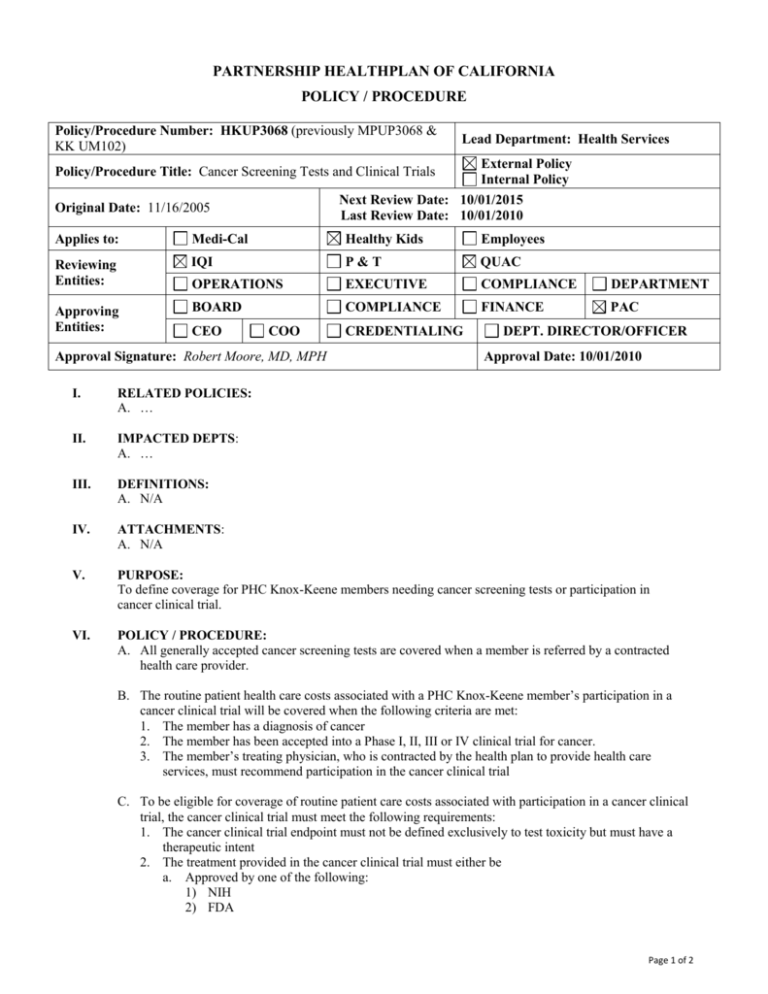
PARTNERSHIP HEALTHPLAN OF CALIFORNIA POLICY / PROCEDURE Policy/Procedure Number: HKUP3068 (previously MPUP3068 & KK UM102) Lead Department: Health Services External Policy Internal Policy Next Review Date: 10/01/2015 Last Review Date: 10/01/2010 Policy/Procedure Title: Cancer Screening Tests and Clinical Trials Original Date: 11/16/2005 Applies to: Medi-Cal Healthy Kids Employees Reviewing Entities: IQI P&T QUAC OPERATIONS EXECUTIVE COMPLIANCE DEPARTMENT Approving Entities: BOARD COMPLIANCE FINANCE PAC CEO COO Approval Signature: Robert Moore, MD, MPH CREDENTIALING DEPT. DIRECTOR/OFFICER Approval Date: 10/01/2010 I. RELATED POLICIES: A. … II. IMPACTED DEPTS: A. … III. DEFINITIONS: A. N/A IV. ATTACHMENTS: A. N/A V. PURPOSE: To define coverage for PHC Knox-Keene members needing cancer screening tests or participation in cancer clinical trial. VI. POLICY / PROCEDURE: A. All generally accepted cancer screening tests are covered when a member is referred by a contracted health care provider. B. The routine patient health care costs associated with a PHC Knox-Keene member’s participation in a cancer clinical trial will be covered when the following criteria are met: 1. The member has a diagnosis of cancer 2. The member has been accepted into a Phase I, II, III or IV clinical trial for cancer. 3. The member’s treating physician, who is contracted by the health plan to provide health care services, must recommend participation in the cancer clinical trial C. To be eligible for coverage of routine patient care costs associated with participation in a cancer clinical trial, the cancer clinical trial must meet the following requirements: 1. The cancer clinical trial endpoint must not be defined exclusively to test toxicity but must have a therapeutic intent 2. The treatment provided in the cancer clinical trial must either be a. Approved by one of the following: 1) NIH 2) FDA Page 1 of 2 Policy/Procedure Number: HKUP3068 (previously Lead Department: Health Services MPUP3068 & KK UM102) ☒External Policy Policy/Procedure Title: Cancer Screening Tests and Clinical Trials ☐Internal Policy Next Review Date: 10/01/2015 Original Date: 11/16/2005 Last Review Date: 10/01/2010 Applies to: ☐ Medi-Cal ☒ Healthy Kids ☐ Employees 3) US Department of Defense 4) US Department of Veterans’ Administration OR b. Involve a drug that is exempt under federal regulations from a new drug application D. PHC shall pay for all routine patient care costs provided at contract rates. Those rendered by noncontracted providers shall be reimbursed at the negotiated rate the health plan would otherwise pay to a contracted provider for the same service, less any applicable co-payments or deductible. VII. REFERENCES: A. California Health and Safety Code, Section 1370.6 and 1367.66 et.seq. B. California Senate Bill 37, Chaptered 2001 VIII. DISTRIBUTION: A. Provider Manual B. PHC Directors IX. POSITION RESPONSIBLE FOR IMPLEMENTING PROCEDURE: X. REVISION DATES: Healthy Kids 11/21/07; 11/19/08; 06/16/10; 10/01/10 PREVIOUSLY APPLIED TO: Healthy Families: MPUP3068 - 10/01/10 to 03/01/2013 ********************************* In accordance with the California Health and Safety Code, Section 1363.5, this policy was developed with involvement from actively practicing health care providers and meets these provisions: Consistent with sound clinical principles and processes Evaluated and updated at least annually If used as the basis of a decision to modify, delay or deny services in a specific case, the criteria will be disclosed to the provider and/or enrollee upon request The materials provided are guidelines used by PHC to authorize, modify or deny services for persons with similar illnesses or conditions. Specific care and treatment may vary depending on individual need and the benefits covered under PHC. Page 2 of 2