HANDOUT: Cardiovascular System
advertisement

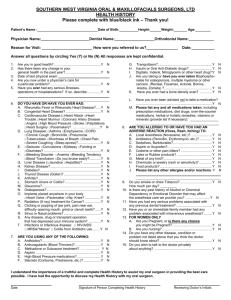
HANDOUT: Cardiovascular System Peripheral Arterial Disease: (PAD/Acute Artial Occlusion/Buerger’s Disease/Raynaud’s Disease) Nonsurgical nursing intervention to promote circulation: 1. Encourage exercise to build collateral circulation-initiate gradually, increase slowly, encourage the client to walk until the point of pain-stop and rest-then walk a little further. 2. Positioning: AVOID crossing legs Refrain from wearing restrictive clothing Elevate legs to reduce swelling (BUT NOT above the level of the heart. 3. Promote vasodilation and AVOID vasoconstriction: Promote a warm environment (warm promotes vasodilation) Wear insulated socks Never apply direct heat to the extremity (sensitivity is decreased may cause BURN) Avoid exposure to COLD (causes vasoconstriction) Avoid Stress, caffeine, and nicotine. (causes vasoconstriction) 4. Administer medications as prescribed: Hemorheologic drugs : pentoxifylline(Trental) increases flexibility of RBC’s and decreases blood viscosity that reduces clot formation and increase blood flow to the extremities. Antiplatelet agents: ASA and clopidogret (Plavix) Antihypertensives: Improve tissue perfusion. Peripheral Venous Disease: (DVT/Thrombophlebitis) Nursing intervention to Promote Circulation: 1. Encourage REST: Bedrest Elevate the extremity above the level of the heart Warm moist compresses Antiembolism stockings 2. Administer Medications: Anticoagulants; (Heparin/Warfarin (coumadin/ Enoxaparin (Lovenox) Heparin- (IV) prevents the formation of further clotting Enoxaprin (Lovenox )( SQ) )used for prevention and treatment of DVT’s Warfarin (coumadin) (PO) When heparin Therapy is discontinued patients are placed on coumadin to produce therapeutic effects. Therapeutic levels of Coumadin: Takes 3-4 days for it to reach its therapeutic effect. Patient needs to be carefully monitored while on this medication for adjustment of the dosage to reach a therapeutic level. 3. Administer analgesics for pain: Anemias: Types of Red Blood Cell Anemias (Identified by ABNORMAL Lab values) 1. Iron deficiency Anemia- MOST COMMON TYPE Not enough Iron to synthesize Hgb. 2. Pernicious Anemia (lack of Intrinsic Factor necessary for absorption of Vitamin B12) 3. Aplastic anemia-When bone marrow stops making enough blood cells. 4. Acquired Hemolytic-Destruction of RBC’s 5. Sick Cell Anemia-Hereditary has abnormal hemoglobin S rather than Hemoglobin A on RBC’s Nursing responsibilities during a cardiac arrest: 1. Utilize the current guidelines for BLS and ACLS 2. Know institutional policy/procedures and location and operation of CRASH CART 3. Have current certification for BLS/ACLS skills. Nursing responsibilities include: Maintain patent airway Acess depth and rate of respirations Provide chest compressions as instructed Assess VS for effectiveness of chest compressions and ventilation Defribrillate the patient as instructed Obtain and maintain IV access Provide medications as ordered Monitor lab values (ie. ABG’sCBC, Electrolytes) Document all interventions and medications (x1 nurse should be a recorder) Dysrhythmia: Heartbeat disturbances (May be benign or life threatening) Monitoring with a telemetry monitor /EKG Classified according to site of origin: SA node, atrioventricular (AV) node or ventricle Effect on heart’s rate and rhythm: Bradycardia, tachycardia, heart block, premature beat, flutter, fibrillation, asystole Treatment: according to patient’s symptoms and the cardiac rhythm Dysrhythmias: Atrial Fibrillation: Erratic electrical activity of the atria, resulting in a rate of 350-600 beats/minute. Atrial depolarization is so uncoordinated during the dysrhythmia that the atria quivers rather than contracts. The AV node is bombarded with impulses and randomly transmits the impulses to the ventricles, causing varied irregular contractions of the ventricles with a ventricular rate of 100 to 80 beats/minute Cause: mitral valve disease or dysfunction, CAD, acute MI, Hypertensive heart disease. Heart failure, cardiomyopathy, or hyperthyroidism. Pacemakers: A battery-operated device that electrically stimulates the heart when the natural pacemaker of the heart fails to maintain an acceptable rhythm. Patient teaching: (Permanent pacemaker discharge teaching) 1. 2. 3. 4. Instruct patient to carry ID card at all times. Teach that batteries last 0 years average Teach patient to take a pulse daily at the same time. Tell the patient the set rate of the pacemaker and to notify the MD if the heart rate is less than 5 beats below pacer rate. 5. Report signs of dizziness, fainting, fatigue, weakness, chest pain, hiccupping, or Palpitations. 6. For patients with pacer -defibrillators inform the patient that anyone touching the patient when the device delivers a shock will feel a slight electrical impulse but the impulse will not harm the person. 7. The patient should avoid direct blows or injury at the generator site. 8. The patient can resume sexual activity as desired , avoiding positions that can put stress on the incision line. 9. Household appliances should not affect pacer function unless held directly over pacer generator. (ie microwave ovens, garage door openers, burglar alarms, etc.) 10. Pacemakers WILL set off airport security detectors and officials should be notified. 11. Instruct the patient to inform other doctors, dentists about the pacer. Some test such as MRI’s may be contraindicated. Pulmonary Embolism: (PE) Priority Intervention: (oxygenation/anticoagulation therapy) At risk patients: Hx. Of thrombophlebitis, Heredity, smokers, peripheral Vascular Disease, Diabetes, oral contraceptives. Phlebitis: Inflammation of a vein: RX. Warm MOIST compresses/ elevate the part Angiography: The insertion of a catheter into a femoral (sometimes brachial) vessel and threading it into right or left side of the heart. Coronary artery narrowings and occlusions are identified by the injection of contrast media under fluoroscopy. Patient indications for angiography: 1. Unstable Angina and ECG Changes 2. Confirmation and determination of location and extent of heart disease. 3. Evaluation of treatment effectiveness. Angina: Temporary and inadequate blood flow and oxygenation to the myocardial tissue That cause CHEST PAIN that is relieved with coronary vasodilators (NTG)/REST Patient teaching: 1. Medications: NTG (SL) x3 (Maximum) at 5 minute intervals (take BP) before administering second and third NTG. PAIN should be relieved after x3 NTG if NOT Call 911 2. REST is important 3. May need surgical intervention PTCA (Percutaneous Transluminal coronary angioplasty) and intracoronary STENT implant. 4. DIET Lo-Fat. LO- Cholesterol, NA Restriction 5. Increase Activity (walking) to improve circulation and decrease cholesterol.