parkinson
advertisement
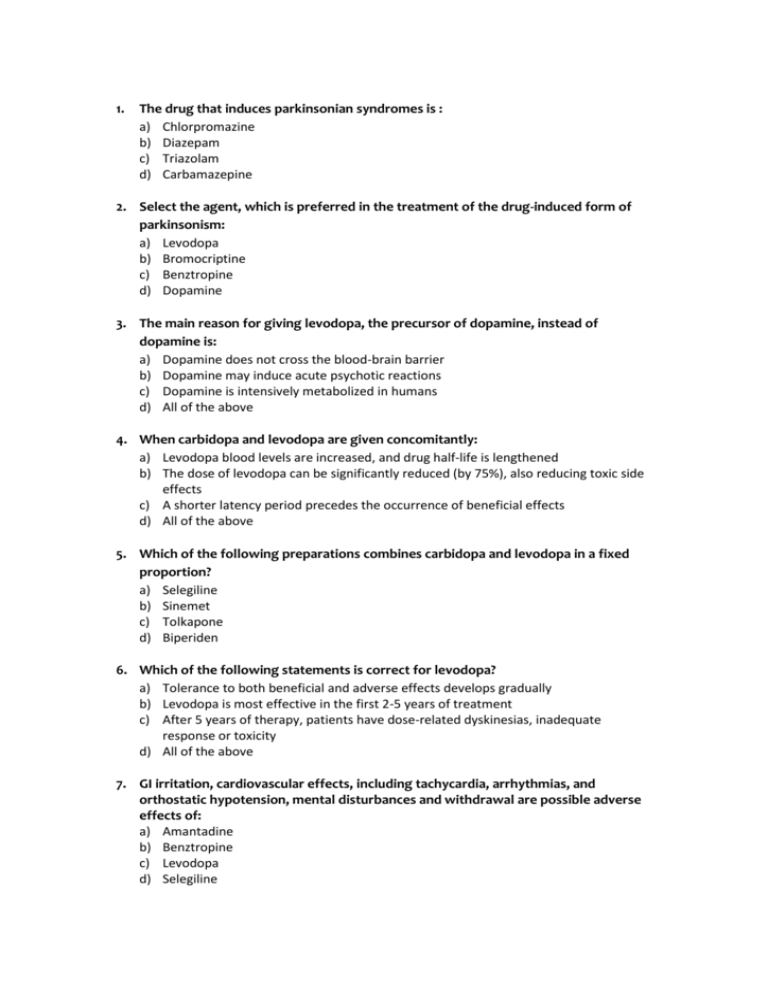
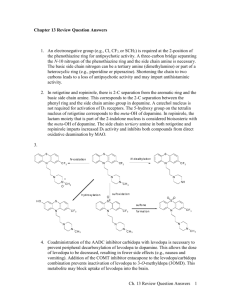
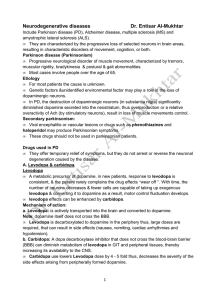
1. The drug that induces parkinsonian syndromes is : a) Chlorpromazine b) Diazepam c) Triazolam d) Carbamazepine 2. Select the agent, which is preferred in the treatment of the drug-induced form of parkinsonism: a) Levodopa b) Bromocriptine c) Benztropine d) Dopamine 3. The main reason for giving levodopa, the precursor of dopamine, instead of dopamine is: a) Dopamine does not cross the blood-brain barrier b) Dopamine may induce acute psychotic reactions c) Dopamine is intensively metabolized in humans d) All of the above 4. When carbidopa and levodopa are given concomitantly: a) Levodopa blood levels are increased, and drug half-life is lengthened b) The dose of levodopa can be significantly reduced (by 75%), also reducing toxic side effects c) A shorter latency period precedes the occurrence of beneficial effects d) All of the above 5. Which of the following preparations combines carbidopa and levodopa in a fixed proportion? a) Selegiline b) Sinemet c) Tolkapone d) Biperiden 6. Which of the following statements is correct for levodopa? a) Tolerance to both beneficial and adverse effects develops gradually b) Levodopa is most effective in the first 2-5 years of treatment c) After 5 years of therapy, patients have dose-related dyskinesias, inadequate response or toxicity d) All of the above 7. GI irritation, cardiovascular effects, including tachycardia, arrhythmias, and orthostatic hypotension, mental disturbances and withdrawal are possible adverse effects of: a) Amantadine b) Benztropine c) Levodopa d) Selegiline 8. Which of the following is the most helpful in counteracting the behavioral complications of levodopa? a) Tolkapone b) Clozapine c) Carbidopa d) Pergolide 9. The D2 receptor agonist with antiparkinsonian activity is : a) Sinemet b) Levodopa c) Bromocriptine d) Selegiline 10. Which of the following antiparkinsonian drugs has also been used to treat hyperprolactinemia? a) Benztropine b) Bromocriptine c) Amantadine d) Levodopa 11. The main reason for avoiding the combined administration of levodopa and an inhibitor of MAO is: a) Respiratory depression b) Hypertensive emergency c) Acute psychotic reactions d) Cardiovascular collapse and CNS depression 12. The mechanism of amantadine action is: a) Stimulating the glutamatergic neurotransmission b) Blocking the excitatory cholinergic system c) Inhibition of dopa decarboxilase d) Selective inhibition of catechol-O-methyltransferase 13. Which of the following antiparkinsonism drugs is an anticholinergic agent? a) Amantadine b) Selegilin c) Trihexyphenidyl d) Bromocriptine 14. Mental confusion and hallucinations, peripheral atropine-like toxicity (e.g. Cycloplegia, tachycardia, urinary retention, and constipation) are possible adverse effects of: a) Sinemet b) Benztropine c) Tolkapone d) Bromocriptine 15. The antiparkinsonism drug which should be avoided in patients with glaucoma: a) Selegilin b) Levodopa c) Bromocriptine d) Trihexyphenidyl 16. Indicate a peripheral dopa decarboxylase inhibitor: a) Tolcapone b) Clozapine c) Carbidopa d) Selegiline 1- Amantadine .. all true EXCEPT : - It increases the re-uptake of DA Amantidine a. # in epilypsy (T) b.Cause urinary retension (T) c.Its effect is lost after few weeks of treatment (T) 1.a 2.c 3.a 4.c 5.d 6.b 7.d 8.c Answer s: 9.b 10c 11.b 12.b 13.a 14.c 15.b 16.d