illustrative case studies
advertisement

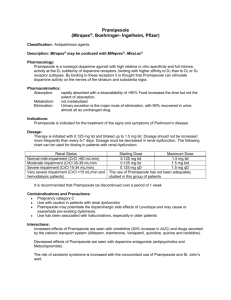
ILLUSTRATIVE CASE STUDIES Case 1: Tranquility restored after surgery Case 1 is a highly active, charismatic person, who is prepared to take risks. His natural hyperthymia has brought him considerable professional success. In 2000, at the age of 44, he was diagnosed with PD. Two years after being prescribed dopaminergic medication (5mgs of pergolide combined with 150 mg of levodopa), he developed a pathological gambling habit. This was accompanied by an internet addiction, nocturnal hyperactivity and an unbridled libido. This hypersexuality had a negative impact on his family life, and the gambling had such serious financial consequences that he voluntarily had himself banned from entering casinos in 2003. During this period, several attempts were made to adjust his medication. However, none of these succeeded in completely eradicating his behavioral problems. While he was no longer gambling by the time he was hospitalized in 2007 with a view to undergoing surgery, a profile of potentially dangerous hyperdopaminergic behavior persisted with, in particular, a pursuit of the rush obtained from excessive speed at the wheel and the making of rash purchases. He was being treated at the time with 3mgs of pergolide and 500 mg of levodopa (Figure 3). The improvement of motor symptoms resulting from STN stimulation permitted the complete discontinuation of dopamine agonists and the reduction of levodopa dosages (to 300 mg/day). One year after surgery, all hyperdopaminergic behaviors had disappeared, in the absence of any onset of apathy, depression or anxiety (Figure 3). The patient’s behavioral profile had been normalized to his complete satisfaction. “I was living like a mad man. I was irrational and unstable. I should have been locked up. But that’s all over now– I’m free from all those vices. I have no more unhealthy thoughts, no more sick needs. Now I am at peace in all respects.” Case 2: post-operative relapse of manic state A 56 year old male with a disease-duration of 12 years was examined in 2007 with a view to surgical intervention. The previous year, while being treated with a combination of pramipexole 3 mg and 1600 mg of levodopa, he experienced a classic manic episode, with heightened irritability and psychotic symptoms which included paranoia, loss of identity, mistrust and feelings of abandonment. In addition, nocturnal hyperactivity and addictive behaviors affecting do-it-yourself, shopping and sexual activity had serious consequences on the patient’s family life (Figure 4). These behavioral problems were alleviated by reducing the dosage of pramipexole, while maintaining that of levodopa. The behavioral assessment carried out at the pre-operative consultation revealed that although none of his symptoms attained pathological levels, the patient continued to function in an overall hyperdopaminergic mode. The patient was offered STN stimulation due to disabling motor fluctuations. A rapid improvement of motor symptoms was noted, permitting the discontinuation of dopamine agonists and a considerable reduction in dosages of remaining medication. However, the onset of a severe restless leg syndrome resulting in insomnia necessitated the prescription of tramadol controlled release 200 mg, clonazepam 2 mg and 100 mg LP of levodopa-carbidopa controlled release at bed-time. The inefficacy of this combination led to the introduction of a dopamine agonist (piribedil 300 mg). Stimulation parameters remained unchanged. This treatment gained control of the restless leg syndrome, but on the patient’s return home, his family noticed worrying behavioral changes. Patient became impulsive and started to take risks when driving. He seemed irritable and muddled, was verbally aggressive and even purchased a top of the range car on a whim. It was at this point that we saw the patient, who himself made the link between his behavior and a manic episode in 2006 (Figure 4). Piribedil dosages were reduced to 200 mg/day and shortly afterwards, a progressive return to normal was noted in terms of behavior. One year after surgery, his treatment remains unchanged and a moderate hyperactivity persists, affecting do-it-yourself and creativity levels. There has, however, been no relapse to the former manic state. Although this patient’s behavior remains highly sensitive to medication, dopamine agonists are essential to offset the severe restless leg syndrome, making management of this patient difficult. Case 3: Preoperative non-motor fluctuations and postoperative non-motor withdrawal state A 58 year old female patient was offered surgery for severe motor fluctuations which developed after 8 years of PD. Before surgery on 1500mg/day levodopa and 4,5 mg of pramipexole she presented with a dopaminergic compulsive medication use, accompanied by severe fluctuations of mood. During OFF periods, she experienced feelings of anxiety, leading on occasion to full panic attacks, accompanied by sensations of suffocation. She felt a great distress, which she expressed by weeping and shouting; she also spoke of ending her life. “It’s hell….I cannot live like this any longer…people are sick of me….I’d be better off ending it all…” During these episodes, she would withdraw from other people and had no wish to speak. During ON periods, on the other hand, her mood would lift. “I feel alive again…I want to do all sorts of things…” (Figures 5 and 6) The positive effect of subthalamic stimulation noted after surgery enabled discontinuation of the dopamine agonist, while a 75 mg/day dosage of levodopa was maintained. Five months after undergoing surgery, the patient developed a severe hypodopaminergic syndrome, with depression, apathy, anxiety and irritability. Her condition was reminiscent of her preoperative severe OFF-period mood state but instead of being intermittent, these non-motor psychic symptoms had become permanent. Indeed, the patient gave up all activity, her anxiety had returned. She was unable to be alone and was experiencing considerable mental suffering: “Living like this is not a life…at least before I had the ON periods…” In response to this situation, dopamine agonist treatment was undertaken (300 mg of piribedil, combined with 3 mg of bromazepam and 20 mg of paroxetine at bedtime). Apathy, anxiety and suicidal thoughts rapidly disappeared. The patient was once again able to gain pleasure from her activities. One year on from surgery her behavioral profile had normalized (Figure 6). Figure 3: CASE 1 behavioral assessments prior to surgery, with treatment consisting of 5mg of pergolide and 150 mg of levodopa (plus benzerazide), and following surgery with patient on 300 mg of levodopa and stimulation parameters as follows: Right STN monopolar, contact 2 negative, 3.5V/60µs/160 Hz ; Left STN monopolar, contact 6 negative, 3V/60 µs/ 160Hz. Red lines indicate scores for severity of symptoms (0=absence; 1= slight; 2=moderate; 3=pronounced; 4= severe) Figure 4: CASE 2 behavioral assessments during both hypo-manic episodes: in 2006 (prior to surgery), with treatment consisting of 3 mg of pramipexol and 1600 mg of levodopa (plus benzerazide); and in 2008 (following surgery), when it consisted of 200 mg of tramadol controlled release, 2 mg of clonazepam, 100 mg of levodopa controlled release (plus carbidopa) at bedtime, and 300 mg of piribedil. Stimulation parameters were as follows: Right STN, monopolar, contact 2 negative, 1.7 V/ 60 µs/130 HZ; Left STN, monopolar, contact 6 negative, 2.5 V/60 s/130 HZ. Red lines indicate scores for severity of symptoms (0=absence; 1= slight; 2=moderate; 3=pronounced; 4= severe) Figure 5: Case 3 Preoperative non-motor fluctuations involving asthenia and affective state using Norris Visual Analogic Scale, apathy (SAS, cut-off for apathy ≥14) and anxiety (BAI, 2235 scores indicates moderate anxiety, ≥ 36 severe anxiety). Preoperative non-motor fluctuations VAS asthenia /80 4.1 64.8 VAS affective state /80 5.8 Apathy scale /42 9 58.9 OFF 19 Beck anxiety inventory /63 15 37 0 ON 20 40 60 Figure 6: Case 3 behavioral assessments prior to surgery (on 1500mg/day levodopa + 4.5mg pramipexole) and one year following surgery (on 300 mg of piribedil, 300mg levodopa, 3 mg bromazepam, 20 mg paroxetine). Red lines indicate scores for severity of symptoms (0=absence; 1= slight; 2=moderate; 3=pronounced; 4= severe)