Neurodegenerative diseases ...
advertisement

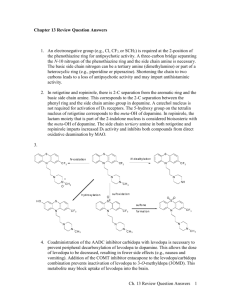
Neurodegenerative diseases Dr. Entisar Al-Mukhtar Include Parkinson disease (PD), Alzheimer disease, multiple sclerosis (MS) and amyotrophic lateral sclerosis (ALS). • They are characterized by the progressive loss of selected neurons in brain areas, resulting in characteristic disorders of movement, cognition, or both. Parkinson disease (Parkinsonism) • Progressive neurological disorder of muscle movement, characterized by tremors, muscular rigidity, bradykinesia & postural & gait abnormalities. • Most cases involve people over the age of 65. Etiology • For most patients the cause is unknown. • Genetic factors &unidentified environmental factor may play a role in the loss of dopaminergic neurons. • In PD, the destruction of dopaminergic neurons (in substantia nigra) significantly diminished dopamine secreted into the neostriatum, thus overproduction or a relative overactivity of Ach (by stimulatory neurons), result in loss of muscle movements control. Secondary parkinsonism: • Viral encephalitis or vascular lesions or drugs such as phenothiazines and haloperidol may produce Parkinsonian symptoms. • These drugs should not be used in parkinsonian patients. Drugs used in PD • They offer temporary relief of symptoms, but they do not arrest or reverse the neuronal degeneration caused by the disease. A. Levodopa & carbidopa Levodopa • A metabolic precursor of dopamine, in new patients, response to levodopa is consistent, & the patient rarely complains the drug effects “wear off ”. With time, the number of neurons decreases & fewer cells are capable of taking up exogenous levodopa & converting it to dopamine as a result, motor control fluctuation develops. • levodopa effects can be enhanced by carbidopa. Mechanism of action: a. Levodopa: is actively transported into the brain and converted to dopamine. Note: dopamine itself does not cross the BBB. • Levodopa is decarboxylated to dopamine in the periphery thus, large doses are required, that can result in side effects (nausea, vomiting, cardiac arrhythmias and hypotension). b. Carbidopa: A dopa decarboxylase inhibitor that does not cross the blood-brain barrier (BBB) can diminish metabolism of levodopa in GIT and peripheral tissues, thereby increasing its availability to the CNS. • Carbidopa use lowers Levodopa dose by 4 - 5 fold thus, decreases the severity of the side effects arising from peripherally formed dopamine. 1 Uses: • Levodopa- carbidopa combination is an efficacious drug regimen. • Withdrawal from the drug must be gradual. Absorption and metabolism: • Levodopa has an extremely short half-life (1 to 2 hours) which causes fluctuations in plasma concentration, that may produce fluctuations in motor response. • Protein rich meal interferes with the transport of levodopa into the CNS. • Also large, neutral amino acids (eg. leucine & isoleucine) compete with levodopa for absorption from the gut & for transport across the BBB. Therefore, levodopa should be taken on an empty stomach, usually 30 minutes before a meal. Adverse effects: 1. Peripheral effects: • Anorexia, nausea & vomiting. • Tachycardia & ventricular extrasystoles. Hypotension may also develop. • Mydriasis, blood dyscrasias & a positive reaction to the Coombs test are seen. • Brownish saliva and urine (due to melanin produced from catecholamine oxidation). 2. CNS effects: • Visual & auditory hallucinations & dyskinesias (abnormal involuntary movements). • Mood changes, depression, psychosis & anxiety. Interactions: • Pyridoxine (vitamin B6) increases peripheral breakdown of levodopa. • Concomitant use of levodopa & non-selective MAOIs (e.g., phenelzine) can cause hypertensive crisis (concomitant administration of these agents is contraindicated). • Cardiac patients should be carefully monitored due to possible cardiac arrhythmias. • In psychotic patients levodopa exacerbates the symptoms which can be treated with low doses of atypical antipsychotics. • In PD, the antipsychotic drugs are contraindicated (potently block dopamine receptors). • Levodopa can increase IOP in patients with glaucoma. B. Catechol-O-methyltransferase (COMT) inhibitors: Entacapone & Tolcapone Normally, methylation of levodopa by COMT to 3-O-methyldopa is a minor pathway. But, when peripheral dopamine decarboxylase is inhibited (by carbidopa), a significant concentration of 3-O-methyldopa is formed & competes with levodopa for transport into the CNS. Thus use of entacapone or tolcapone increases central uptake of levodopa. Pharmacokinetics: • Tolcapone has a relatively long duration of action, while entacapone requires frequent dosing. • Dose adjustment may be needed in patients with moderate or severe cirrhosis. Adverse effects: • Tolcapone cause fulminating hepatic necrosis therefore, entacapone has largely replaced tolcapone. C. Selegiline & Rasagiline Selegiline: Selectively inhibits MAO type B (which metabolizes dopamine), selegiline high 2 doses, may cause hypertensive crises (due to inhibition of MAO type A which metabolizes NE & serotonin). • Selegiline is metabolized to methamphetamine & amphetamine, that may produce insomnia. Rasagiline • Irreversible & selective inhibitor of brain MAO type B. • More potent than selegiline. D. Dopamine-receptor agonists • Include an ergotamine derivative ( Bromocriptine) & nonergot drugs ( Ropinirole, Pramipexole, Rotigotine & Apomorphine). • Durations of actions are longer than that of levodopa. • Bromocriptine, pramipexole & ropinirole are effective for PD complicated by motor fluctuations & dyskinesias, but are ineffective in patients who don’t responded to levodopa. • Side effects (sedation, hallucinations, confusion, nausea & hypotension) limit the utility of the dopamine agonists 1. Bromocriptine: • Comparing to levodopa dyskinesia is less prominent ,whereas other side effects are more common with bromocriptine. • Mental psychiatric illness may be worsened. • Used cautiously in patients with MI or peripheral vascular disease history. • Bromocriptine, has the potential to cause pulmonary & retroperitoneal fibrosis. 2. Apomorphine, Pramipexole, Ropinirole & Rotigotine: • Apomorphine & rotigotine are available as injectable & transdermal formulations respectively. • Apomorphine is used for acute management of the hypomobility “off” phenomenon in severe and advanced PD to supplement oral medications. • Dopamine agonists may delay levodopa use in early PD & may decrease the dose of levodopa in advanced PD. • Rrenal dysfunction necessitate pramipexole dosage adjustments, also cimetidine inhibits renal tubular secretion of pramipexole. • Fluoroquinolone antibiotics or fluoxetine may inhibit ropinirole metabolism. E. Amantadine • Antiviral drug with antiparkinsonism action.It (1) increases dopamine release, (2) blocks cholinergic receptors & (3) inhibits the N-methyl-D-aspartate (NMDA) type of glutamate receptors. • Its high doses may induce acute toxic psychosis. • Less efficacious than levodopa. • Less effective against tremor, but more effective than anticholinergics against rigidity & bradykinesia. F. Antimuscarinic agents : Benztropine, Trihexyphenidyl, Procyclidine & Biperiden • Less effective than levodopa & play only an adjuvant role. • Contraindicated in patients with glaucoma, prostatic hyperplasia, or pyloric stenosis. 3