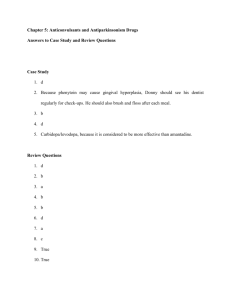
Anti- seizure and Anti-Parkinson Drugs
advertisement

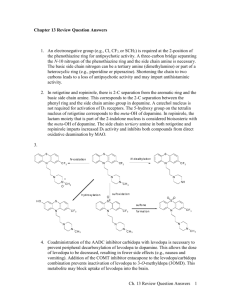
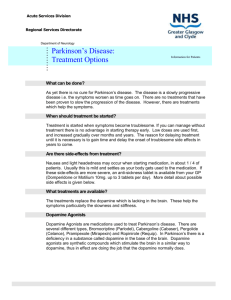
Anti-seizure and AntiParkinson Drugs Nur 3704 By Linda Self Seizure Disorders Seizures involve a brief episode of abnormal electrical activity in nerve cells of the brain that may be accompanied by changes in behavior or appearance Convulsion is a tonic-clonic type of seizure characterized by spasmodic contractions of muscles Seizures May be caused by hypoglycemia, fever, electrolyte imbalances, overdoses of drugs, withdrawal of alcohol or sedative-hypnotic drugs or as a result of epilepsy Epilepsy Seizures occur in a chronic, recurrent pattern Abnormal and excessive electrical discharges in a group of nerve cells affecting brain function Abnormality in neuronal plasma membranes results in increased permeability and responsiveness to stimuli Epilepsy Involves neuron fire with escalating frequency and amplitude, reaches threshold and spreads to adjacent normal neurons Diagnosed by clinical signs and symptoms of seizure activity and by abnormal brain wave patterns on the EEG Cause is idiopathic in 60-80% of children Different Kinds of Seizures Partial—begin in a specific area of the brain. Movements may be automatic, repetitive or aversive. Behavior may be bizarre. Generalized—bilateral and symmetric and w/o discernible point of origin in the brain. Tonic-clonic. Tonic phase is sustained skeletal contraction, clonic phase is rapid and rhythmic jerking movements. Seizures cont. Absence—abrupt alterations in consciousness that last only seconds Status Epilepticus—life-threatening, generalized tonic-clonic convulsions lasting for several minutes or at close intervals. Hypotension, hypoxia and cardiac dysrhythmias may occur. Antiepileptic Drugs (AEDs) Mechanisms of action Suppress seizures by decreasing movement of ions into nerve cells, altering the activity of neurotransmitters (GABA and glutamate) or both. Actions of drugs may increase GABA (inhibitory), decrease glutamate (excitatory) or affect Na+ and Ca++ ions thus decreasing responsiveness Indications Maintenance treatment of epilepsy Stop tonic-clonic seizures Status epilepticus Treatment of choice for status epilepticus is Ativan then maintenance on Dilantin or Cerebyx AEDs also useful in bipolar disorder and for neuropathic pain Contraindications/Precautions Caution if renal or hepatic impairment Caution if CNS depression History of hypersensitivity Dilantin in patients with bradycardia or heart block Tegretol with bone marrow depression Antiseizure Drugs Dilantin is the prototype. Often initial drug of choice. Careful in switching from generic to trade name as bioavailability may vary (can lead to toxicity). Monitor drug levels. May gibe IV or orally Pregnancy Cat. D. Dilantin (phenytoin) Adverse effects include: hypotension, bradycardia, cardiac dysrhythmias, thrombophlebitis, gingival hyperplasia, folic deficiency. Extremely irritating to veins. Dilute, use only saline Give no faster than 50mg/minute Cerebyx (fosphenytoin) Formulation that is hydrolyzed to dilantin. Approved for status epilepticus and for those who cannot take oral preparation. Less tissue irritation than phenytoin, can be diluted w/dextrose and can be given more quickly than phenytoin. Tegretol (carbamazepine) For partial, generalized tonic-clonic and mixed seizures. Also useful in treating trigeminal neuralgia and bipolar disorder. Contraindicated in bone marrow depression and in patients on MAOIs. MAOIs must be discontinued at least 14 days before starting Tegretol. Preg. Cat. D. Valium (diazepam) Indicated for acute convulsive seizures and for status epilepticus. Pregnancy Cat. D. Given in repeat doses then followed by long-acing anticonvulsant such as phenytoin (Dilantin) Phenobarbital Long acting barbiturate that is used alone or with another AED Causes sedation and cognitive impairment Long half-life taking 2-3 weeks to reach therapeutic levels Preg. Cat. D Neurontin (gabapentin) Treatment of partial seizures, often with other AEDs Eliminated by kidneys Adverse effects: dizziness, drowsiness, fatigue, loss of muscle coordination, tremors, nausea, vomiting, gingivitis, pruritus Preg. Cat. C Other AEDs Zarontin (ethosuximide)—choice for absence seizures Lamictal (lamotrigine) used w/other AEDs for treatment of partial seizures. Adverse effects: skin rashes to Stevens-Johnson syndrome, visual changes, ataxia, drowsiness. Caution w/co-admin. of Depakote (valproic acid) Other AEDs Topamax (topiramate)—broad spectrum of activity. Excreted by kidneys. Must decrease dosage if renally impaired. Most common side effects include: ataxia, drowsiness, dizziness, nausea and renal stones. Keppra (levetiracetam) Newer drug for tx of partial seizures Mechanism of action is unknown Inhibits abnormal firing w/o affecting normal neuronal excitability Not metabolized by liver Low potential for drug interactions Adverse effects: decreases in RBCs and WBCs, lability, paresthesias, pharyngitis General considerations in AEDs Take regularly to maintain serum levels Do not stop taking abruptly Do not drive a car, operate machinery which requires alertness Ensure provider is aware of other meds taken due to many interactions General considerations cont. Caution during pregnancy or breastfeeding No switching generic phenytoin to Dilantin due to differences in formulation May need to take folic acid, calcium, vitamin D or vitamin K if on Dilantin General considerations cont. Meticulous oral care If diabetic, closer monitoring of blood sugars Report unexplained bleeding, joint pains, rashes, fevers, sore throat, petechiae Lamictal may cause photosensitivity or serious skin rashes Monitoring AED therapy Based on client response Periodic measurements of serum drug levels necessary Baseline blood studies to include: CBC, platelet ct., LFTs, renal function tests then repeat on periodic basis Monitoring AED therapy Poor control of seizures—look at compliance, incorrect diagnosis of type of seizure, use of wrong drug for type of seizure, inadequate drug dosage, drug interactions (theophylline), use of alcohol or electrolyte imbalances Parkinson’s Disease Is a chronic, progressive, degenerative disorder of the CNS Results from destruction or degenerative changes in dopamineproducing nerve cells in the substantia nigra Cause is unclear Occurs equally in men and women between 50-80 years Parkinson’s Disease Early onset parkinsonism is felt to have genetic component (in those less than 45yo) Phenothiazines can cause druginduced parkinsonism Is characterized by tremors, bradykinesia, joint and muscular rigidity Neurotransmitter Imbalance Basal ganglia normally contains balance of dopamine and acetylcholine Balance necessary to regulate posture, muscle tone and voluntary movement In Parkinson’s, lack inhibitory dopamine and thus an increase in excitatory acetylcholine Anti-Parkinson drugs Drugs used in tx increased levels of dopamine or to inhibit the actions of acetylcholine in the brain Dopaminergic Drugs Levodopa is mainstay of drug therapy for idiopathic parkinsonism Serves as the prototype Increases dopamine concentrations in the brain Dopamine cannot penetrate bloodbrain barrier but levodopa can. Is then converted to dopamine by enzyme AADC. Levodopa Once converted to dopamine, then is stored in presynaptic dopaminergic neurons. With advanced disease, fewer neurons allow for less storage capacity. Thus, it has a shorter duration of action. Large amounts of Levodopa required as it undergoes extensive peripheral metabolism leaving less for use in the brain. Levidopa/Carbidopa Peripheral metabolism is reduced leaving more available for brain use when carbidopa is added to levodopa. Adding carbidopa “ties up” decarboxylase and enzyme COMT. This then allows greater utilization by the brain Levodopa reserved for later tx of Parkinson’s as body develops tolerance and loses effectiveness over time. Anticholinergics Centrally active agents are used Atropine and scopolamine not used due to side effects Anticholinergics decrease the effects of acetylcholine which decreases the excess of acetylcholine to dopamine Examples: Cogentin (benztropine) and Benadryl (diphenhydramine) Others Symmetrel (amantadine)-an antiviral that also increases release and inhibits the reuptake of dopamine in the brain Used initially, loses efficacy quickly w/continuous usage (6-8 weeks) Often used w/levodopa More effective than anticholinergics buts less so than levodopa Parlodel and Permax Parlodel (bromocriptine) and Permax (pergolide)—ergot derivatives that directly stimulate dopamine receptors in the brain Used with levodopa/carbidopa to prolong the effectiveness Caution in CAD, can cause pulmonary fibrosis Mirapex (pramipexole) and Requip (ropinirole) Are newer dopamine receptor stimulants Approved for both beginning and advanced stages Renal insufficiency affects excretion of Mirapex Eldepryl (selegiline) Increases dopamine in the brain by inhibiting metabolism by MAO-B (MAO-A acts more specifically on tyramine, norepinephrine, epinephrine, and serotonin which can result in severe hypertension and stroke) At oral doses of 10mg/day or less, Eldepryl is selective for MAO-B, higher doses will result in stimulation of both MAO receptors Drug Selection For drug induced parkinsonism or EPS, an anticholinergic is drug of choice Early parkinsonism, anticholinergic may be initial agent in younger than 60 years Symmetrel useful in bradykinesia or tremors Drug Selection cont. Dopamine agonist improves bradykinesia, rigidity, impaired dexterity, speech, gait and tremor In advanced disease-anticholinergic plus levodopa/carbidopa or Symmetrel in combination or Dopamine agonist in combination Drug Selection cont. Reserve levodopam/carbidopam as eventually loses its efficacy Drug Dosage Doses are adjusted as disease progresses Levodopa/carbidopa must be individualized Will gradually have to increase the levodopa to achieve therapeutic levels When adding a dopaminergic, will need to reduce dosage of levodopa/carbidopa