Pharmacy TAR Procedure - Previously
advertisement

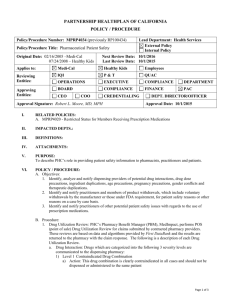
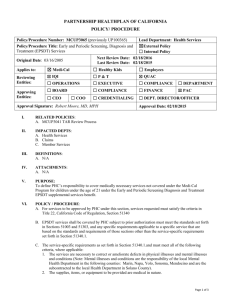
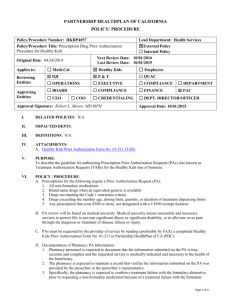
PARTNERSHIP HEALTHPLAN OF CALIFORNIA POLICY / PROCEDURE Policy/Procedure Number: MCRO4018 (previously RO100418) Lead Department: Health Services External Policy Policy/Procedure Title: Pharmacy TAR Procedure Internal Policy Original Date: 04/25/1994 (Pharmacy Next Review Date: 10/1/2016 Authorization) Last Review Date: 10/1/2015 Applies to: Medi-Cal Healthy Kids Employees Reviewing Entities: IQI P&T QUAC OPERATIONS EXECUTIVE COMPLIANCE DEPARTMENT Approving Entities: BOARD COMPLIANCE FINANCE PAC CEO COO Approval Signature: Robert L. Moore, MD, MPH CREDENTIALING DEPT. DIRECTOR/OFFICER Approval Date: 10/1/2015 I. RELATED POLICIES: N/A II. IMPACTED DEPTS.: III. DEFINITIONS: N/A IV. ATTACHMENTS: N/A V. PURPOSE: To describe the guidelines for authorizing pharmacy Treatment Authorization Requests (TARs) VI. POLICY / PROCEDURE: A. Prescriptions for the following require a Treatment Authorization Request (TAR): 1. All non-formulary medications 2. Brand name drugs when an equivalent generic is available 3. Drugs not meeting the Code 1 restriction criteria 4. Drugs exceeding the member age, dosing limit, quantity, or duration of treatment dispensing limits 5. Any prescription that costs $500 or more, not designated with a # $500 exempt footnote B. TAR review will be based on medical necessity. Medical necessity means reasonable and necessary services to protect life, to prevent significant illness or significant disability, or to alleviate severe pain through the diagnosis or treatment of disease, illness or injury. C. TARs must be requested by the provider of service by sending (preferably by FAX) a completed TAR form to Partnership HealthPlan of CA (PHC). D. Documentation of Pharmacy TAR Information 1. Pharmacy personnel is expected to document that the information submitted on the TAR is true, accurate and complete and the requested service is medically indicated and necessary to the health of the patient. 2. The pharmacy is expected to maintain a record that verifies the information submitted on the TAR was provided by the prescriber or the prescriber’s representative. 3. Specifically, the pharmacy is expected to confirm a treatment failure with the formulary alternative prior to requesting a non-formulary medication because of a treatment failure with the formulary alternative. The pharmacy is expected to keep written documentation of this information. Page 1 of 4 Policy/Procedure Number: MCRO4018 (previously RO100418) Lead Department: Health Services ☒External Policy ☐Internal Policy Next Review Date: 10/1/2016 Last Review Date: 10/1/2015 ☐ Healthy Kids ☐ Employees Policy/Procedure Title: Pharmacy TAR Procedure Original Date: 04/25/1994 (Pharmacy Authorization) Applies to: ☒ Medi-Cal E. The PHC Clinical Pharmacist, Pharmacy Technician, Pharmacy Director, or Registered Nurse HealthPlan staff will perform all initial TAR reviews. All reviews by the Pharmacy Technician adhere to PHC written criteria and are performed under supervision of a HealthPlan pharmacist. F. References used to determine authorization decisions shall include, but are not be limited to: 1. Medical references which list FDA labeling information including current editions of the Physicians’ Desk Reference, Drug Facts & Comparisons, USP Drug Information for the Health Care Professional, and other references as available on the internet. 2. PHC prior authorization criteria. 3. PHC Clinical Practice Guidelines. 4. Consultation with the Medical Director and/or outside consultants. G. The PHC Clinical Pharmacist, Pharmacy Technician, Pharmacy Director, or Registered Nurse HealthPlan staff reviewer may take the following TAR actions: 1. Approve: An approved TAR is a TAR approved for the requested drug, strength and quantity. If the reviewer changes the units (# of fills) requested or date of service, this is still considered an approved TAR. 2. Approve as Modified: A modified TAR is a TAR that is approved with a quantity that differs from the requested quantity submitted by the provider. The reviewer may approve a TAR as Modified on the basis of their clinical judgment without consultation from the Medical Director. 3. Deny based on the following administrative criteria: a. TAR not required b. Carve-out drug c. Member not eligible with PHC on date of service d. Duplicate request e. Member has other primary pharmacy insurance f. TAR not submitted on a timely basis g. Insufficient information submitted on the TAR to further review h. Additional requested information not received by PHC within 14 days of initial TAR 4. Defer to the requesting provider – PHC provides members with a notice of deferral of a request by a provider for a pharmacy service. Notice of the deferral shall be delayed for 14 days to allow the provider time to submit the additional information requested by the plan and to allow time for the plan to make a decision. If, after 14 days from the plan’s receipt of the request for prior authorization, the provider has not complied with the plan’s request for additional information, the plan shall provide the member notice of denial because lack of additional requested information not received within 14days of the initial TAR. If, within that 14 day period, the provider does comply, the plan shall take appropriate action on the request. If the member is sent notification of approval, modification or denial within the 14 day time period, a deferral notification is not sent. 5. Defer for Chief Medical Officer (CMO) or Medical Director Review H. The Chief Medical Officer (CMO) or Medical Director must be available, physically or by telephone, during business hours to assist with the review of TARs. 1. CMO/Medical Director reviews may be requested by the Clinical Pharmacist in cases of potential denial due to questionable medical necessity or inappropriate use of a drug. 2. The CMO/Medical Director may contact the prescribing physician and/or consultants for additional information, as required, to assist him/her in rendering a decision about the case. Page 2 of 4 Policy/Procedure Number: MCRO4018 (previously RO100418) Lead Department: Health Services ☒External Policy ☐Internal Policy Next Review Date: 10/1/2016 Last Review Date: 10/1/2015 ☐ Healthy Kids ☐ Employees Policy/Procedure Title: Pharmacy TAR Procedure Original Date: 04/25/1994 (Pharmacy Authorization) Applies to: ☒ Medi-Cal 3. The CMO/Medical Director and Clinical Pharmacists can authorize denials based on medical criteria or make any exceptions/changes to the established medical policy for pharmacy management. 4. If the CMO/Medical Director is not available, he/she may designate another physician or Clinical Pharmacist to fulfill the requirements under H 1, 2, 3. I. Determination and provider notification of PHC determinations will be made within one (1) business day of receiving a completed TAR. J. Determination and provider notification of PHC determinations for urgent TARs will be made the same business day the TAR is received, if the TAR is received by 3:00 PM. All TARs received by PHC designated as urgent by the submitting provider are subject to review to determine if the TAR should be processed as urgent. K. Determination and member notification of PHC determinations, which includes the reason for the denial, deferral, or modification and information about the appeals process, is made within two (2) working days of the following TAR actions: 1. A denied TAR that lacks medical justification for the intended use of the drug. 2. A denied TAR in which insufficient information was submitted on the TAR 3. A denied TAR in which additional requested information was not received by PHC within 14 days of the initial TAR 4. A modified TAR. 5. A deferred TAR in which insufficient information was submitted on the TAR. L. Determination and member notification of PHC determinations of deferred TARs are explained in G. 4. M. Emergency TARs outside of PHC’s normal business hours: 1. During PHC’s normal business hours (M-F 8 AM to 5 PM), pharmacies may call the PHC Pharmacy Department for an emergency 5 day fill. The pharmacy department may authorize up to a 5-day supply of medication, pending further authorization by PHC if the Pharmacy Department is not able to determine the medical necessity of the full prescription. 2. Outside of PHC’s normal business hours PHC’s contracted Pharmacy Benefit Manager (PBM) is authorized to respond to emergency TARs outside of PHC’s normal business hours, including weekends and holidays. The PBM may authorize up to a 5-day supply of medication, pending further authorization by PHC. 3. When both PHC and the contracted PBM are unavailable, PHC will authorize a retroactive TAR allowing the pharmacy to dispense up to a 5 day supply of a non-formulary drug. N. Retroactive TARs must be received by PHC within fifteen (15) business days of requested date of service. Retroactive TARs received after fifteen (15) business days of requested date of service may be considered for review under the following conditions: 1. When certification of the Medi-Cal beneficiary’s eligibility by the county welfare department was delayed. 2. When other coverage (e.g., Medicare or other health insurance programs) denied payment of a claim for services. 3. When a member does not identify himself/herself to the provider as a PHC member by deliberate concealment or because of physical or mental incapacity to so identify himself/herself. 4. If a member has obtained retroactive eligibility, the TAR must be received by PHC within 60 days of the members obtaining Medi-Cal eligibility. Page 3 of 4 Policy/Procedure Number: MCRO4018 (previously RO100418) Lead Department: Health Services ☒External Policy ☐Internal Policy Next Review Date: 10/1/2016 Last Review Date: 10/1/2015 ☐ Healthy Kids ☐ Employees Policy/Procedure Title: Pharmacy TAR Procedure Original Date: 04/25/1994 (Pharmacy Authorization) Applies to: ☒ Medi-Cal O. TAR approval will be granted for a member to continue the use of a non-formulary single source drug which is part of a prescribed therapy in effect before enrollment with PHC until the therapy is no longer prescribed by the member’s doctor. VII. REFERENCES: N/A VIII. DISTRIBUTION: A. PHC Department Directors, B. PHC Provider and Practitioner Manuals, C. SharePoint IX. POSITION RESPONSIBLE FOR IMPLEMENTING PROCEDURE: A. Associate Director of Pharmacy Operations X. REVISION DATES: 03/23/95; 10/10/97 (name change only); 05/28/99; 12/15/99, 10/17/01; 04/17/02; 11/20/02; 11/19/03; 04/21/04; 04/3/08; 01/27/11; 08/18/11; 01/17/13; 01/16/14; 10/1/2015 PREVIOUSLY APPLIED TO: XI. POLICY DISCLAIMER: A. In accordance with the California Health and Safety Code, Section 1363.5, this policy was developed with involvement from actively practicing health care providers and meets these provisions: 1. Consistent with sound clinical principles and processes; 2. Evaluated and updated at least annually; 3. If used as the basis of a decision to modify, delay or deny services in a specific case, the criteria will be disclosed to the provider and/or enrollee upon request. B. The materials provided are guidelines used by PHC to authorize, modify or deny services for persons with similar illnesses or conditions. Specific care and treatment may vary depending on individual need and the benefits covered under PHC. Page 4 of 4