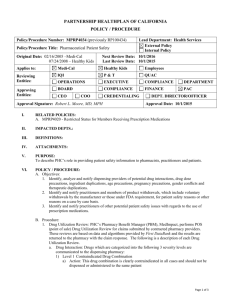
Prescription Drug Prior Authorization Procedure for Healthy Kids
advertisement

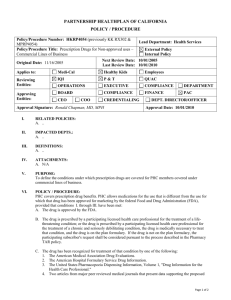
PARTNERSHIP HEALTHPLAN OF CALIFORNIA POLICY/ PROCEDURE Policy/Procedure Number: HKRP4057 Policy/Procedure Title: Prescription Drug Prior Authorization Procedure for Healthy Kids Lead Department: Health Services ☒External Policy ☐ Internal Policy Next Review Date: 10/01/2016 Last Review Date: 10/01/2015 Original Date: 04/24/2014 Applies to: ☐ Medi-Cal ☒ Healthy Kids ☐ Employees Reviewing Entities: ☒ IQI ☒P&T ☐ QUAC ☐ OPERATIONS ☐ EXECUTIVE ☐ COMPLIANCE ☐ DEPARTMENT ☐ BOARD ☐ COMPLIANCE ☐ FINANCE ☒ PAC ☐ CREDENTIALING ☐ DEPT. DIRECTOR/OFFICER Approving Entities: ☐ CEO ☐ COO Approval Signature: Robert L. Moore, MD MPH Approval Date: 10/01/2015 I. RELATED POLICIES: N/A II. IMPACTED DEPTS: III. DEFINITIONS: N/A IV. ATTACHMENTS: A. Healthy Kids Prior Authorization Form No. 61-211 (TAR) V. PURPOSE: To describe the guideline for authorizing Prescription Prior Authorization Requests (PAs) also known as Treatment Authorization Requests (TARs) for the Healthy Kids line of business. VI. POLICY / PROCEDURE: A. Prescriptions for the following require a Prior Authorization Request (PA): 1. All non-formulary medications 2. Brand name drugs when an equivalent generic is available 3. Drugs not meeting the Code 1 restriction criteria 4. Drugs exceeding the member age, dosing limit, quantity, or duration of treatment dispensing limits 5. Any prescription that costs $500 or more, not designated with a # $500 exempt footnote B. PA review will be based on medical necessity. Medical necessity means reasonable and necessary services to protect life, to prevent significant illness or significant disability, or to alleviate sever pain through the diagnosis or treatment of disease, illness or injury. C. PAs must be requested by the provider of service by sending (preferably by FAX) a completed Healthy Kids Prior Authorization Form No. 61-211 to Partnership HealthPlan of CA (PHC). D. Documentation of Pharmacy PA Information: 1. Pharmacy personnel is expected to document that the information submitted on the PA is true, accurate and complete and the requested service is medically indicated and necessary to the health of the beneficiary. 2. The pharmacy is expected to maintain a record that verifies the information submitted on the PA was provided by the prescriber or the prescriber’s representative. 3. Specifically, the pharmacy is expected to confirm a treatment failure with the formulary alternative prior to requesting a non-formulary medication because of a treatment failure with the formulary Page 1 of 4 Policy/Procedure Number: HKRP4057 Lead Department: Health Services Policy/Procedure Title: Prescription Drug Prior Authorization ☒ External Policy Procedure for Healthy Kids ☐ Internal Policy Next Review Date: 10/01/2016 Original Date: 04/24/2014 Last Review Date: 10/01/2015 ☒ Healthy Kids ☐ Employees Applies to: ☐ Medi-Cal alternative. The pharmacy is expected to keep written documentation of this information. E. The PHC Clinical Pharmacist, Pharmacy Technician, or Pharmacy Director will perform all initial PA reviews. All reviews by the Pharmacy Technician adhere to PHC written criteria and are performed under the supervision of a HealthPlan pharmacist. F. References used to determine authorization decisions shall include, but are not limited to: 1. Medical references which list Food and Drug Administration (FDA) labeling information including current editions of the Physicians’ Desk Reference, Drug Facts & Comparisons, USP Drug Information for the Health Care Professional, and other references as available on the internet. 2. PHC prior authorization criteria. 3. PHC Clinical Practice Guidelines. 4. Consultation with the Medical Director and /or outside consultants. G. The PHC Clinical Pharmacist, Pharmacy Technician, or Pharmacy Director reviewer may take the following PA actions: 1. Approve: An approved PA is a PA approved for the requested drug, strength and quantity. If the reviewer changes the units (# of fills) requested or date of service, this is still considered an approved PA. 2. Approve as Modified: A modified PA is a PA that is approved with a quantity that differs from the requested quantity submitted by the provider. The reviewer may approve a PA as Modified on the basis of their clinical judgment without consultation from the Medical Director. 3. Deny based on the following administrative criteria: a. TAR not required b. Carve-out drug c. Member not eligible with PHC on date of service d. Duplicate request e. Member has other primary pharmacy insurance f. TAR not submitted on a timely basis g. Insufficient information submitted on the PA to further review H. The Chief Medical Officer (CMO) or Medical Director must be available, physically or by telephone, during business hours to assist with the review of TARs. 1. CMO/Medical Director reviews may be requested by the Clinical Pharmacist in cases of potential denial due to questionable medical necessity or inappropriate use of a drug. 2. The CMO/Medical Director may contact the prescribing physician and/or consultants for additional information, as required, to assist him/her in rendering a decision about the case. 3. The CMO/Medical Director and Clinical Pharmacists can authorize denials based on medical criteria or make any exceptions/changes to the established medical policy for pharmacy management. 4. If the CMO/Medical Director is not available, he/she may designate another physician or Clinical Pharmacist to fulfill the requirements under section H 1, 2, and 3. Page 2 of 4 Policy/Procedure Number: HKRP4057 Lead Department: Health Services Policy/Procedure Title: Prescription Drug Prior Authorization ☒ External Policy Procedure for Healthy Kids ☐ Internal Policy Next Review Date: 10/01/2016 Original Date: 04/24/2014 Last Review Date: 10/01/2015 ☒ Healthy Kids ☐ Employees Applies to: ☐ Medi-Cal I. Provider notification of PHC determinations will be made within two (2) business days of receiving a completed PA for the following determinations: 1. The prescribing provider’s request is approved; or 2. The prescribing provider’s request is disapproved as not medically necessary or not a covered benefit; or 3. The prescribing provider’s request is disapproved as missing material information necessary to approve or disapprove the PA; 4. The beneficiary is no longer eligible for coverage; 5. The PA request was not submitted on the required form. Please resubmit your request on the Healthy Kids PA Form No. 61-211. J. Determination and provider notification of PHC determinations for urgent PAs will be made the same business day the PA is received if the PA is received by 3:00 PM. All PAs received by PHC designated as urgent by the submitting provider are subject to review to determine if the PA should be processed as urgent. K. In the event the notice of denial, consistent with the requirements under section I 2 and 3 is not sent to the prescribing provider within two (2) business days, the PA request shall be deemed approved. L. Determination and member notification of PHC determinations, which includes the reason for the denial or modification and information about the appeals process, is made within two (2) business days of the following PA actions: 1. A denied PA that lacks medical justification for the intended use of the drug or not a covered benefit. 2. A denied PA in which insufficient information was submitted on the PA. 3. A modified PA. M. Emergency PAs outside of PHC’s normal business hours: 1. During PHC’s normal business hours (M-F 8 AM to 5 PM), pharmacies may call the PHC Pharmacy Department for an emergency 5 day fill. The pharmacy department may authorize up to a 5-day supply of medication, pending further authorization by PHC if the Pharmacy Department is not able to determine the medical necessity of the full prescription. 2. Outside of PHC’s normal business hours PHC’s contracted Pharmacy Benefit Manager (PBM) is authorized to respond to emergency TARs outside of PHC’s normal business hours, including weekends and holidays. The PBM may authorize up to a 5-day supply of medication, pending further authorization by PHC. 3. When both PHC and the contracted PBM are unavailable, PHC will authorize a retroactive TAR allowing the pharmacy to dispense up to a 5 day supply of a non-formulary drug. N. Retroactive TARs must be received by PHC within fifteen (15) business days of requested date of service. Retroactive TARs received after fifteen (15) business days of requested date of service may be considered for review under the following conditions: 1. When certification of the Medi-Cal beneficiary’s eligibility by the county welfare department was delayed. 2. When other coverage (e.g., Medicare or other health insurance programs) denied payment of a claim for services. Page 3 of 4 Policy/Procedure Number: HKRP4057 Lead Department: Health Services Policy/Procedure Title: Prescription Drug Prior Authorization ☒ External Policy Procedure for Healthy Kids ☐ Internal Policy Next Review Date: 10/01/2016 Original Date: 04/24/2014 Last Review Date: 10/01/2015 ☒ Healthy Kids ☐ Employees Applies to: ☐ Medi-Cal 3. When a member does not identify himself/herself to the provider as a PHC member by deliberate concealment or because of physical or mental incapacity to so identify himself/herself. 4. If a member has obtained retroactive eligibility, the TAR must be received by PHC within 60 days of the members obtaining Medi-Cal eligibility. O. TAR approval will be granted for a member to continue the use of a non-formulary single source drug which is part of a prescribed therapy in effect before enrollment with PHC until the therapy is no longer prescribed by the member’s doctor. VII. REFERENCES: A. State of California Department of Managed Health Care Title 28, California Code of Regulations Section 1300.67.241 Prescription Drug Prior Authorization Form Process Control No. 2012-3880. VIII. DISTRIBUTION: A. PHC Department Directors, B. PHC Provider and Practitioner Manuals, C. SharePoint IX. POSITION RESPONSIBLE FOR IMPLEMENTING PROCEDURE: A. Associate Director of Pharmacy Operations X. REVISION DATES: Healthy Kids 04/24/14; 10/1/15 PREVIOUSLY APPLIED TO: XI. POLICY DISCLAIMER: A. In accordance with the California Health and Safety Code, Section 1363.5, this policy was developed with involvement from actively practicing health care providers and meets these provisions: 1. Consistent with sound clinical principles and processes; 2. Evaluated and updated at least annually; 3. If used as the basis of a decision to modify, delay or deny services in a specific case, the criteria will be disclosed to the provider and/or enrollee upon request. B. The materials provided are guidelines used by PHC to authorize, modify or deny services for persons with similar illnesses or conditions. Specific care and treatment may vary depending on individual need and the benefits covered under PHC. Page 4 of 4