Screening-Guidelines-revised

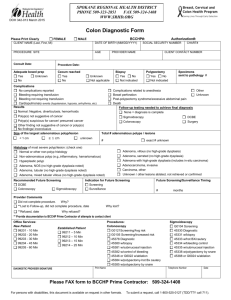
CCSP Reimbursable Screening Guidelines for Average, Increased, and High Risk Patients
(Revised 5/19/14)
Risk Category
Average Risk
Asymptomatic individuals who are not in the categories below (including those with a previous hyperplastic polyp as their most advanced lesion)
Age to Begin
50 years
Age to stop screening: 85
Note:
Cormorbidity should be
Reimbursable Screening Recommendation
Colonoscopy every 10 years OR Flexible
Sigmoidoscopy or DCBE every 5 years considered for those between
75-85
45 with symptoms
Colonoscopy
Increased Risk
Individuals age 45 and older with blood in the stool or a positive FOBT are eligible for endoscopic evaluation through CCSP
Individual with family history of CRC or a documented advanced adenomatous polyp in a first degree relative diagnosed at age 60 years or older
Either colorectal cancer or documented advanced adenomatous polyp(s), in any first degree relative before age 60, or in two or more first degree relatives at any age (if not hereditary syndrome)
On previous endoscopic screening, individual with one or two small (<1 cm) adenomatous polyps with only low grade dysplasia and/or sessile serrated polyp without dysplasia
On previous endoscopic screening, individual with any of the following:
Start screening at 40 years
Age 40 or 10 years before the youngest colon cancer/adenoma in the family, whichever is earlier
At initial time pf polyp diagnosis
At initial time of polyp diagnosis
Colonoscopy every 10 years OR Flexible
Sigmoidoscopy or DCBE every 5 years
Colonoscopy every 5-10 years
Colorectal cancer in relatives more distant than first degree does not increase risk substantially above the average risk group
Colonoscopy 5 years after initial polyp removal. If that exam is normal, then colonoscopy every 5-10 years thereafter.
Colonoscopy 3 years [providing that piecemeal removal has not been done and the adenoma(s) are
3-10 adenomas or
One large (>/=1 cm) adenomatous polyp or
Any adenoma with villous features or high grade dysplasia or
Any large (>/= 1 cm) sessile serrated polyp
Any sessile serrated polyp with cytologic dysplasia
On previous endoscopic screening, individual with more than 10 adenomas at one examination
Personal history of curative-intent resection of colorectal cancer
High Risk
Individual with family history of Familial
Adenomatous Polyposis (FAP)
Individual with family history of hereditary nonpolyposis colon cancer (HNPCC)
Personal history of inflammatory bowel disease:
(Chronic Ulcerative Colitis or Crohn’s disease) completely removed]
If the follow-up exam is normal or shows only one or two small tubular adenomas with low-grade dysplasia, then colonoscopy every 5 years thereafter.
At initial time of polyp diagnosis
One year after diagnosis
<3 years-interval established by clinical judgment
Colonoscopy one year after resection. If normal, then the interval before the subsequent exam should be 3 years. If normal, then the interval before the subsequent exam should be 5 years.
Puberty Sigmoidoscopy (or colonoscopy) and genetic testing.
If polyposis is confirmed by endoscopy and/or if genetic testing positive, then refer patient to a center with experience in managing FAP.
Age 21-25 years Colonoscopy and genetic testing. If genetic test is
Cancer risk begins to be significant 8 years after the onset of pancolitis
OR
12-15 years after the onset of left-sided normal, screen as per average risk.
If genetic test is positive or patient has not had genetic testing, then refer patient to a center with experience in managing HNPCC.
Colonoscopy with multiple biopsies every 1-2 years, and refer patient to a center with experience in surveillance and management of IBD.
Important Note: The program can only cover the costs of the colorectal cancer screening in patients with established, long-standing disease (>8 years) and not for the diagnosis or symptomatic evaluation of patients with IBD.
colitis.