2013 March Understanding How to Code Colonoscopies
advertisement

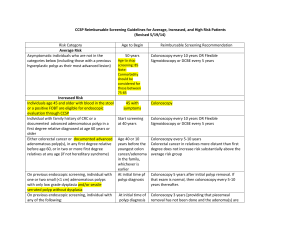
Understanding How to Code Colonoscopies Presented by Barbara Parker, CPC Prepared by Lori Dafoe, CPC Facts • More than two million colonoscopies are performed each • • • • year in the United states. Most of them are performed on an outpatient basis. Can be performed for screening, diagnostic, or therapeutic purposes. Coding can be challenging, especially those procedures that include biopsy and polyp removal. Accurate assignment of colonoscopy procedure codes depends on the documentation of the procedure performed and the technique used to perform the procedure. Facts • A colonoscopy includes an exam of the entire colon, from the rectum to the cecum, and may also include examination of the terminal ileum. In order to bill for a completed colonoscopy, the scope must be advanced past the splenic flexure. Factors to Consider Was another procedure(s) performed during the diagnostic colonoscopy? If so, what was the procedure(s)? What was the technique used? What instruments were used? Once the above factors are determined, use the following information as guidance to determine when each of the following codes is reported: CPT 45378, Colonoscopy, flexible, proximal to the splenic flexure; diagnostic, with or without collection of specimen(s) by brushing or washing, with or without colon decompression is used to report diagnostic colonoscopies. All surgical colonoscopy codes include a diagnostic colonoscopy. Therefore, if any other procedure but a brushing or washing is performed during the diagnostic colonoscopy, the surgical colonoscopy should be billed using codes 45380-45385. It would not be appropriate to report code 45378 in addition to the therapeutic procedure. HCPC G0105 & G0121 Effective January, 1, 1998, Medicare created HCPCS Level II codes which are equivalent to and are used in place of CPT code 45378 when reporting outpatient colonoscopies for screening of colorectal cancer on Medicare patients. Code G0105 to report a screening colonoscopy for patients who are at high risk for colorectal cancer. High risk is an individual with one or more of the following: close relative (sibling, parent or child) who has had colorectal cancer or an adenomatous polyp, family history of familial adenomatous polyposis, a family history of hereditary nonpolyposis colorectal cancer, a personal history of adenomatous polyps, a personal history of colorectal cancer, or inflammatory bowel disease, including Crohn’s Disease and ulcerative colitis. Code G0121 is used to report colonoscopies for colorectal screening on patients not meeting criteria for high risk. If an abnormality is found during a screening colonoscopy that results in a therapeutic procedure (e.g., biopsy, polypectomy, excision of lesion), then the appropriate CPT code is used instead of HCPCS Level II codes G0105 or G0121. Code Selection Surgical Colonoscopy Codes are determined by the physician’s documentation of the procedure performed. The record must state the method used to remove the tissue, lesion or polyp. CPT 45384, Colonoscopy, flexible, proximal to the splenic flexure; with removal of tumor(s), polyp(s), or other lesion(s) by hot biopsy forceps or bipolar cautery. This code is used when bipolar cautery and monopolary cautery forceps are used to remove tissue. Hot biopsy forceps, also called monopolar cautery forceps, create heat in the metal portion of the forceps cup by causing current to flow from the device to a grounding pad on the patient’s body to cauterize the lesion or polyp. Bipolar cautery uses current that runs from one portion of the tip of the cautery device to another to cauterize and remove a lesion or polyp. CPT 45385, Colonoscopy, flexible, proximal to the splenic flexure; with removal of tumor(s), polyp(s), or other lesion(s) by snare technique. This is the most often used technique for performing a polypectomy during a colonoscopy. When the snare cautery technique is used, a wire loop is heated and then placed around the desired piece of tissue or polyp to shave off the polyp or lesion. It’s important to note that the snare device may be used with or without heat or cautery. The key term in using this code is “snare” removal. Hot snare, cold snare, monopolar snare and bipolar snare should all be reported with code 45385. CPT 45383, Colonoscopy, flexible, proximal to splenic flexure; with ablation of tumor(s), polyp(s), or other lesion(s) not amenable to removal by hot biopsy forceps, bipolar cautery or snare technique. The description of this code is not as clear cut. It can be misleading because it only indicates what techniques the code should not be reported for. Hot biopsy and bipolar cautery techniques are reported with CPT 43584. Snare technique is reported with CPT 43585. CPT 45383 can be reported for the ablation of a tumor, polyp or other lesion (including arteriovenous malformations) using a number of different devices including heater probe, bipolar cautery prober, or argon laser, argon plasma coagulators (APC). Examples of CPT 45383, 45384, & 45385 45380, Colonoscopy with biopsy, single or multiple Describes the use of forceps to grasp and remove a small piece of tissue without the application of cautery. The procedure note may describe the biopsy using cold biopsy forceps, or may not mention the device at all. The biopsy may be from an obvious lesion that is too large to remove, from a suspicious area of abnormal mucosa, or from a lesion or polyp so small that it can be completely removed during the performance of the biopsy. Colonoscopy with removal by snare technique (45385) should not be used for the removal of a small polyp by “biopsy” or “cold forceps” technique. All lesions or polyps removed by cold biopsy foceps are reported using code 45380. CPT 45380 CPT 45381, Colonoscopy, flexible, proximal to the splenic flexure; with directed submucosal injection(s), any substance. Reported when any substance is injected into the submucosal. Substances include saline, India ink, methylene blue, Botox and steroids. For example, code 45381 would be reported for an injection to “tattoo” an area with India ink for later identification during a subsequent procedure. Code 45381 should be reported as an additional service to any other therapuetic procedure performed at the same time. Code 45381 is not used to report injections to control bleeding. CPT 45381 CPT 45382, Colonoscopy, flexible, proximal to the splenic flexure; with control of bleeding, (e.g., injection, bipolar cautery, unipolar cautery, laser, heater probe, stapler, plasma coagulator). Used to describe injection to control bleeding resulting from a number of causes including diverticulosis, angiodysplasia or prior session intervensions. Bleeding that starts as a result of an intervention performed during the colonoscopy, such as a polypectomy or biopsy, and is controlled by any method is considered part of the initial therapeutic procedure and should not be reported separately with code 45382. CPT 45382 Multiple Procedures When multiple colonoscopy procedures are performed during the same session, documentation must specifically describe the type of lesion(s), the location of the lesion(s), and the techinique used to perform each procedure. One code is used to report multiple procedures using the same technique. Multiple codes are reported when more than one procedure was performed using multiple techniques. When more than one colonoscopy code is reported for the same session, they should be listed in descending order value with modifier -59 (Distinct procedural service) to identify that the service was performed at a separate site. Modifiers Modifier 59, Separate Procedure. Used to indicate different sites, incisions, encounters. Example: Colonoscopy with removal of polyp at the transverse colon by snare technique (45385) is performed at the same session as a biopsy proximal to the splenic flexure (45380). Modifier -59 is appropriate because the two procedures are performed on separate lesions at separate locations. Report as 45385, 45380-59. Modifiers Modifier 51, Multiple Procedure. Used to indicate multiple procedures performed at the same session by the same provider. Multiple procedure discount should be applied to the reimbursement of the code, so it is very important to add this modifier to the second and subsequent code based on RVU order. It is not based on the order the services were performed or based the primary procedure based on what was done to address the patient’s illness. Example: Colonoscopy (45378) performed at the same session as upper endoscopy (43200). Use modifier 51 on the upper endoscopy because RVU’s are lower than the colonoscopy. Report as 45378, 43200-51. Modifiers Tells the payor, “This is a service that should be processed without a patient due balance, because it was a preventive service with an A or B rating from the USPSTF”. Modifier 33, Preventive Services. Used for commercial claims. Modifer PT, CRC screening test converted to diagnostic test or other procedure. Used for Medicare claims. If using these modifiers, make sure your primary diagnosis is the v-code describing the appropriate type of screening, followed by the diagnosis for the findings. Modifiers For coding purposes, the colonoscope must pass the splenic flexure. If this is not achieved, it is an incomplete colonoscopy. The documentation should clearly state how far the scope was inserted and the reason for the discontinuation. Modifier 53, Discontinued procedure. Used on physician claims. Not to be used to report the elective cancellation of a procedure prior to inducation of anesthesia or surgical preparation in the surgical suite. (NOTE: Prior to January 1, 2011, providers had been instructed to use modifier -52 to report an incomplete colonoscopy.) Modifer 73, Discontinued procedure prior to anesthesia. Used for facility claims. Modifier 74, Discontinued procedure after the administration of anesthesia. Used for facility claims. Modifiers Modifier 22, Increased Procedural services. Used to denote circumstances for which a procedure was complicated, complex, difficult, or took significantly more time than usually required by the provider to complete the procedure. Example: The physician performs a colonoscopy on a patient with a tortuous colon. The gastroenterologist spends 110 minutes navigating the scope through the twists and turns of the patient’s lower intestine. Even when justified, it can be difficult at best to obtain higher than normal reimbursement from payers. The documentation should clearly describe the unusual nature of the service to justify the additional charge! Diagnosis Coding - Screening Screening colonoscopy performed on a patient with no presenting signs or symptoms related to the digestive system, but have reached the age for routine screenings should be coded using: V76.51 Special screening for malignant neoplasm, colon. All additional findings are reported as secondary codes. Additional secondary codes for high risk can be used when the information is recorded in the patient’s record: V10.05 Personal history of malignant neoplasm, large intestine V12.72 Personal history of colonic polyps V16.0 Family history of malignant neoplasm, gastrointestinal tract High risk is coded when any of the following conditions are noted by the provider or in the patient's history: Close relative (sibling, parent, or child) has had colorectal cancer or an adenomatous polyposis Family history of hereditary nonpolyposis colorectal cancer Personal history of adenomatous polyps Personal history of colorectal cancer Personal history of inflammatory bowel disease, Crohn's disease, or ulcerative colitis Diagnostic colonoscopy performed the confirmed diagnosis should be coded. If no definitive findings are noted, then code(s) for the symptoms prompting the service should be used. Diagnosis Coding - Diagnostic Diagnostic colonoscopy performed the confirmed diagnosis should be coded. If no definitive findings are noted, then code(s) for the symptoms prompting the service should be used. For example, blood in stool/hemopositive stool, bleeding from rectum, iron deficiency anemia of unknown cause, change in bowel habits, persistent abdominal pain. THANK YOU!! Presented by Barbara Parker, CPC Prepared by Lori Dafoe, CPC