For moderate elevation (6 to 7 mEq/L), shift potassium intracellularly
advertisement

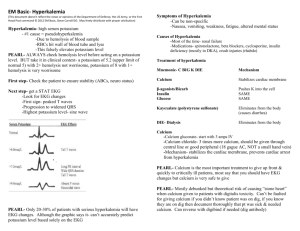
Top Introduction Potassium (K+) Sodium (Na+) Magnesium (Mg++) Calcium (Ca++) Summary References Potassium (K+) The magnitude of the potassium gradient across cell membranes determines excitability of nerve and muscle cells, including the myocardium. Rapid or significant changes in the serum potassium concentration can have life-threatening consequences. Evaluation of serum potassium must consider the effects of changes in serum pH. When serum pH falls, serum potassium rises because potassium shifts from the cellular to the vascular space. When serum pH rises, serum potassium falls because potassium shifts from the vascular space into the cells. Effects of pH changes on serum potassium should be anticipated during therapy for hyperkalemia or hypokalemia and during any therapy that may cause changes in serum pH (eg, treatment of diabetic ketoacidosis). Hyperkalemia Although hyperkalemia is defined as a serum potassium concentration >5 mEq/L, it is moderate (6 to 7 mEq/L) and severe (>7 mEq/L) hyperkalemia that are lifethreatening and require immediate therapy. Hyperkalemia is most commonly seen in patients with end-stage renal disease. Other causes are listed in the Table. Many medications can contribute to the development of hyperkalemia. Identification of potential causes of hyperkalemia will contribute to rapid identification and treatment.1–3 View this table: TABLE. Common Causes of Hyperkalemia [in this window] [in a new window] Signs and symptoms of hyperkalemia include weakness, ascending paralysis, and respiratory failure. A variety of electrocardiographic (ECG) changes suggest hyperkalemia. Early findings include peaked T waves (tenting). As the serum potassium rises further, flattened P waves, prolonged PR interval (first-degree heart block), widened QRS complex, deepened S waves, and merging of S and T waves can be seen. If hyperkalemia is left untreated, a sine-wave pattern, idioventricular rhythms, and asystolic cardiac arrest may develop. Treatment of Hyperkalemia The treatment of hyperkalemia is determined by its severity and the patient’s clinical condition. Stop sources of exogenous potassium administration (eg, consider supplements and maintenance IV fluids) and evaluate drugs that can increase serum potassium (eg, potassium-sparing diuretics, angiotensin-converting enzyme [ACE] inhibitors, nonsteroidal anti-inflammatory agents). Additional treatment is based on the severity of the hyperkalemia and its clinical consequences. The following sequences list the treatments for hyperkalemia in order of priority. For mild elevation (5 to 6 mEq/L), remove potassium from the body with 1. Diuretics: furosemide 40 to 80 mg IV 2. Resins: Kayexalate 15 to 30 g in 50 to 100 mL of 20% sorbitol either orally or by retention enema For moderate elevation (6 to 7 mEq/L), shift potassium intracellularly with 1. Glucose plus insulin: mix 25 g (50 mL of D50) glucose and 10 U regular insulin and give IV over 15 to 30 minutes 2. Sodium bicarbonate: 50 mEq IV over 5 minutes (sodium bicarbonate alone is less effective than glucose plus insulin or nebulized albuterol, particularly for treatment of patients with renal failure; it is best used in conjunction with these medications4,5) 3. Nebulized albuterol: 10 to 20 mg nebulized over 15 minutes For severe elevation (>7 mEq/L with toxic ECG changes), you need to shift potassium into the cells and eliminate potassium from the body. Therapies that shift potassium will act rapidly but they are temporary; if the serum potassium rebounds you may need to repeat those therapies. In order of priority, treatment includes the following: Shift potassium into cells: 1. Calcium chloride (10%): 500 to 1000 mg (5 to 10 mL) IV over 2 to 5 minutes to reduce the effects of potassium at the myocardial cell membrane (lowers risk of ventricular fibrillation [VF]) 2. Sodium bicarbonate: 50 mEq IV over 5 minutes (may be less effective for patients with end-stage renal disease) 3. Glucose plus insulin: mix 25 g (50 mL of D50) glucose and 10 U regular insulin and give IV over 15 to 30 minutes 4. Nebulized albuterol: 10 to 20 mg nebulized over 15 minutes5–7 Promote potassium excretion: 5. Diuresis: furosemide 40 to 80 mg IV 6. Kayexalate enema: 15 to 50 g plus sorbitol PO or per rectum 7. Dialysis Hypokalemia Hypokalemia is defined as a serum potassium level <3.5 mEq/L. The most common causes of low serum potassium are gastrointestinal loss (diarrhea, laxatives), renal loss (hyperaldosteronism, severe hyperglycemia, potassium-depleting diuretics, carbenicillin, sodium penicillin, amphotericin B), intracellular shift (alkalosis or a rise in pH), and malnutrition. The major consequences of severe hypokalemia result from its effects on nerves and muscles (including the heart). The myocardium is extremely sensitive to the effects of hypokalemia, particularly if the patient has coronary artery disease or is taking a digitalis derivative. Symptoms of mild hypokalemia are weakness, fatigue, paralysis, respiratory difficulty, constipation, paralytic ileus, and leg cramps; more severe hypokalemia will alter cardiac tissue excitability and conduction. Hypokalemia can produce ECG changes such as U waves, T-wave flattening, and arrhythmias (especially if the patient is taking digoxin), particularly ventricular arrhythmias. Pulseless electrical activity or asystole may develop. Treatment of Hypokalemia The treatment of hypokalemia consists of minimizing further potassium loss and providing potassium replacement. IV administration of potassium is indicated when arrhythmias are present or hypokalemia is severe (potassium level of <2.5 mEq/L). Gradual correction of hypokalemia is preferable to rapid correction unless the patient is clinically unstable. Administration of potassium may be empirical in emergent conditions. When indicated, the maximum amount of IV potassium replacement should be 10 to 20 mEq/h with continuous ECG monitoring duringinfusion. A more concentrated solution of potassium may be infused if a central line is used, but the tip of the catheter used for the infusion should not extend into the right atrium. If cardiac arrest from hypokalemia is imminent (ie, malignant ventricular arrhythmias are present), rapid replacement of potassium is required. Give an initial infusion of 10 mEq IV over 5 minutes; repeat once if needed. Document in the patient’s chart that rapid infusion is intentional in response to life-threatening hypokalemia. Introduction Background Diabetic ketoacidosis (DKA) is an acute, major, life-threatening complication of diabetes. DKA mainly occurs in patients with type 1 diabetes, but it is not uncommon in some patients with type 2 diabetes. DKA is defined clinically as an acute state of severe uncontrolled diabetes that requires emergency treatment with insulin and intravenous fluids. Biochemically, DKA is defined as an increase in the serum concentration of ketones greater than 5 mEq/L, a blood glucose level of greater than 250 mg/dL (although it is usually much higher), blood pH of less than 7.2, and a bicarbonate level of 18 mEq/L or less. Pathophysiology Diabetic ketoacidosis (DKA) is a complex disordered metabolic state characterized by hyperglycemia, acidosis, and ketonuria. DKA usually occurs as a consequence of absolute or relative insulin deficiency that is accompanied by an increase in counterregulatory hormones (ie, glucagon, cortisol, growth hormone, epinephrine). This type of hormonal imbalance enhances hepatic gluconeogenesis, glycogenolysis, and lipolysis. Hepatic gluconeogenesis, glycogenolysis secondary to insulin deficiency, and counter-regulatory hormone excess result in severe hyperglycemia, while lipolysis increases serum free fatty acids. Hepatic metabolism of free fatty acids as an alternative energy source (ie, ketogenesis) results in accumulation of acidic intermediate and end metabolites (ie, ketones, ketoacids). Ketones include acetone, beta hydroxybutyrate, and acetoacetate. Progressive rise of blood concentration of these acidic organic substances initially leads to a state of ketonemia. Natural body buffers can buffer ketonemia in its early stages. When the accumulated ketones exceed the body's capacity of extracting them, they overflow into urine (ie, ketonuria). If the situation is not treated promptly, more accumulation of organic acids leads to frank clinical metabolic acidosis (ie, ketoacidosis), with a drop in pH and bicarbonate1 serum levels. Respiratory compensation of this acidotic condition results in rapid shallow breathing (Kussmaul respirations). Ketones, in particular beta hydroxybutyrate, induce nausea and vomiting that consequently aggravate fluid and electrolyte loss already existing in DKA. Moreover, acetone produces the characteristic fruity breath odor of ketotic patients. Hyperglycemia usually exceeds the renal threshold of glucose absorption and results in significant glycosuria. Consequently, water loss in the urine is increased due to osmotic diuresis induced by glycosuria. This incidence of increased water loss results in severe dehydration, thirst, tissue hypoperfusion, and, possibly, lactic acidosis. Typical free water loss in DKA is approximately 6 liters or nearly 100 mL/kg of body weight. The initial half of this amount is derived from intracellular fluid and precedes signs of dehydration, while the other half is from extracellular fluid and is responsible for signs of dehydration. Hyperglycemia, osmotic diuresis, serum hyperosmolarity, and metabolic acidosis result in severe electrolyte disturbances. The most characteristic disturbance is total body potassium loss. This loss is not mirrored in serum potassium levels, which may be low, within the reference range, or even high. Potassium loss is caused by a shift of potassium from the intracellular to the extracellular space in an exchange with hydrogen ions that accumulate extracellularly in acidosis. A large part of the shifted extracellular potassium is lost in urine because of osmotic diuresis. Patients with initial hypokalemia are considered to have severe and serious total body potassium depletion. High serum osmolarity also drives water from intracellular to extracellular space, causing dilutional hyponatremia. Sodium also is lost in the urine during the osmotic diuresis. Typical overall electrolyte loss includes 200-500 mEq/L of potassium, 300-700 mEq/L of sodium, and 350-500 mEq/L of chloride. The combined effects of serum hyperosmolarity, dehydration, and acidosis result in increased osmolarity in brain cells that clinically manifests as an alteration in the level of consciousness. Frequency United States Currently, diabetic ketoacidosis (DKA) occurs less frequently in patients with known diabetes because of the introduction of diabetes educational programs in most diabetes clinics. These programs teach patients with diabetes how to test for urinary ketones and how to adjust their insulin regimen on sick days in order to avoid DKA. In spite of the advancement in self-care of patients with diabetes, DKA still accounts for 50% of diabetes-related admissions in young persons and 1-2% of all primary diabetes-related admissions. DKA frequently is observed during the diagnosis of type 1 diabetes and frequently indicates this diagnosis. Exact incidence is not known, but it is estimated to be 1 out of 2000. In a study of 127 patients with DKA who were admitted to a pediatric intensive care unit, Bradley and Tobias concluded that multiple weaknesses existed in the prehospital care of these patients.2 These included "lack of appropriate laboratory evaluation, excessive insulin dosing (both bolus doses and infusion rates), lack of fluid resuscitation, use of inappropriate fluids for resuscitation, and the use of sodium bicarbonate." Although DKA was a common problem in patients with diabetes who were treated with continuous subcutaneous insulin infusion (SCII) through insulin infusion pumps, incidence of DKA became less frequent with the introduction of new pumps equipped with sensitive electronic alarm systems that alert users when the infusion catheter is blocked. Frequent blood glucose monitoring at home makes DKA less likely to occur in such patients because they always can search, in a timely manner, for possible reasons for unexpectedly high blood glucose values before the condition progresses to DKA. DKA also occurs in pregnant women, either with preexisting diabetes or with diabetes diagnosed during pregnancy. Physiologic changes unique to pregnancy provide a background for the development of DKA. DKA in pregnancy is a medical emergency, because the mother and fetus are at risk for morbidity and mortality. International The incidence of diabetic ketoacidosis in developing countries is not known, but it may be higher than in industrialized nations.3 Mortality/Morbidity When diabetic ketoacidosis (DKA) is treated properly, it rarely causes any residual effects. The overall mortality rate from DKA ranges from 1-10% of all DKA admissions, according to hospital facilities and the experiences of people who have dealt with this acute metabolic condition. Better understanding of the pathophysiology of DKA and proper monitoring and correction of electrolytes has resulted in significant reduction in the overall mortality rate from this life-threatening condition in most developed countries. Mortality rates from DKA have markedly decreased from 7.96% 20 years ago to 0.67%.4 Best results are always observed in patients treated in ICUs during the first 1-2 days of hospitalization. In contrast, the mortality rate still is high in developing countries and among nonhospitalized patients. This high mortality rate illustrates the necessity of early diagnosis and the implementation of effective prevention programs. Cerebral edema remains the most common cause of mortality, particularly in young children and adolescents.5 Cerebral edema frequently results from rapid intracellular fluid shifts. Other causes of mortality include severe hypokalemia, adult respiratory distress syndrome, and comorbid states (eg, pneumonia, acute myocardial infarction). Race The incidence of diabetic ketoacidosis is higher in whites because of the higher incidence of type 1 diabetes in this racial group. Sex The incidence of diabetic ketoacidosis (DKA) is slightly greater in females than in males for reasons that are unclear. Recurrent DKA is frequently seen in young women with type 1 diabetes mellitus (DM) and is mostly caused by the omission of insulin treatment. Age Among persons with type 1 diabetes, diabetic ketoacidosis is much more common in young children and adolescents than it is in adults. Clinical History Insidious increased thirst (ie, polydipsia) and urination (ie, polyuria) are the most common early symptoms of diabetic ketoacidosis (DKA). Nausea and vomiting usually occur and may be associated with diffuse abdominal pain. Generalized weakness and fatigability may occur. Altered consciousness in the form of mild disorientation or confusion is a possible symptom. Although frank coma is uncommon, it may occasionally occur when the condition is neglected or if dehydration or acidosis is severe. Symptoms of possible associated intercurrent infection may include fever, dysuria, coughing, malaise, and arthralgia, among others. Acute chest pain or palpitation may occur in association with myocardial infarction. Painless infarction is not uncommon in patients with diabetes and should always be suspected in elderly patients. Patients may present with a history of failure to comply with insulin therapy or missed insulin injections due to vomiting or psychological reasons. History of rapid weight loss is a symptom in patients who are newly diagnosed with type 1 diabetes. Physical Signs of dehydration - Weak and rapid pulse, dry tongue and skin, hypotension, and increased capillary refill time Patient odor - Characteristic acetone odor Signs of acidosis - Shallow rapid breathing or air hunger (Kussmaul or sighing respiration), abdominal tenderness, and disturbance of consciousness o Although these signs are not usual in all cases of diabetic ketoacidosis (DKA), their presence signifies a severe form of DKA. o Emphasizing that no direct correlation exists between the degree of acidosis, hyperglycemia, and the disturbances in the level of consciousness is important. Signs of intercurrent illness - Myocardial infarction, urinary tract infection (UTI), pneumonia, and perinephric abscess, among others o Noticing that the body temperature may be within the reference range or low, even in the presence of intercurrent infection, is particularly important. o Search for signs of infection is mandatory in all cases. Causes Patients with type 1 diabetes6 o Diabetic ketoacidosis (DKA) present at diagnosis of type 1 diabetes due to acute insulin deficiency (occurs in 25% of patients) o Poor compliance with insulin through the omission of insulin injections either due to lack of patient or guardian education or as a result of psychological stress, particularly in adolescents o Bacterial infection and intercurrent illness (eg, UTI, vomiting) o Klebsiella pneumoniae (the leading cause of bacterial infections precipitating DKA) o Medical, surgical, or emotional stress o Brittle diabetes o Idiopathic (no identifiable cause) o Insulin infusion catheter blockage o Mechanical failure of insulin infusion pump Patients with type 2 diabetes7 o Intercurrent illness (eg, myocardial infarction, pneumonia, prostatitis, UTI) o Medication (eg, corticosteroids, pentamidine, clozapine) More on Diabetic Ketoacidosis Differential Diag Treatm References Further Reading Print This Email This Search for CME/CE on This Topic » RELATED EMEDICINE ARTICLES Diabetic Ketoacidosis (Pediatrics: Cardiac Disease and Critical Care Medicine) Diabetic Ketoacidosis (Emergency Medicine) Pediatrics, Diabetic Ketoacidosis (Endocrinology) Disorders of Carbohydrate Metabolism (Neurology) Patient Education Diabetic Ketoacidosis Overview Diabetes Center Diabetic Ketoacidosis Symptoms Diabetic Ketoacidosis Causes Diabetic Ketoacidosis Treatment RELATED MEDSCAPE ARTICLES News Glycemic Control Deteriorates Rapidly in Children With Type 2 Diabetes Sensor-Augmented Insulin Pump Therapy Trumps Safety of Continuous Potassium Chloride Infusion in Critical Care Summary Patients in critical care often require supplemental potassium chloride if levels in their blood are below acceptable level. Common practice is to administer a single dose of potassium chloride under controlled conditions via a drip, before checking if a further dose is required. The purpose of this study is to ensure that it is safe to administer potassium chloride continuously with the dose varied according to patient needs. Description The use of potassium supplementation is commonplace in the critical care environment. Patients often have abnormal serum potassium levels due to active disease processes. Conditions such as acute renal failure and metabolic acidosis precipitate hyperkalaemia, with ileus and insensible losses causing hypokalaemia. Both hypoand hyperkalaemia can cause life-threatening arrythmias so it is prudent to rectify aberrant levels. The standard treatment of hypokalaemia in intensive care units is by intravenous administration of potassium chloride. This can be given either as a dilute solution as maintenance intravenous fluid therapy, or as a concentrated solution by intermittent infusion. Alternatively potassium can be given as a concentrated solution by continuous infusion. All techniques require regular monitoring of the patient's serum potassium level with appropriate alterations to the administration regime. From a theoretical standpoint it would make sense to give potassium by continuous infusion as this allow slow but steady correction of hypokalaemia. A continuous infusion should prevent rapid fluctuations in the serum level that could be caused by intermittent infusions, which may precipitate arrhythmia. However continuous infusions require vigilant monitoring to ensure that hyperkalaemia does not occur and must be given into a central vein to avoid the risk of phlebitis. The use of intermittent infusions has been used safely in the critical care setting under physician guidance. A retrospective review reported the outcomes of the administration of 495 infusion sets to 190 individuals. While they identified 2 instances of post-infusion hyperkalaemia, neither was associated with any adverse sequelae. Analysis showed a no correlation between serum potassium increase post-infusion and serum creatinine, thus advocating the use of this therapy in patients with renal failure. In light of this valuable safety data, they proceeded with a prospective cohort study involving 40 patients on their Intensive Care Unit. Again the outcomes were favourable with a mean increase of 0.48mmol/L after administration of 20mmol in 100ml of saline over 1 hour. They reported no instances of hyperkalaemia, and data suggested a decreased instance of ectopic beats versus control patients. The use of a variable dose regime dictated by serum potassium concentration has also been assessed. In a prospective cohort study 20, 30 or 40mmol was administered over 1 hour to 48 patients based on their initial measured potassium level. They only reported 2 instances of hyperkalaemia but neither patient experienced any complications. Usefully they found that patients with oliguric renal failure (creatinine 283 ± 127 micromol/L) had no greater mean increase in potassium level after infusion than patients with normal creatinine clearance. Two other methods have been suggested. The first, assessed on a paediatric intensive care unit, administered potassium at a rate of 0.25mmol/kg/hr to patients with serum potassium < 3.5mmol/L and ECG abnormalities. The infusion was continued until the ECG abnormalities were corrected. Serum potassium wasn't measured until after completing the infusion, and although the mean increase was only 0.75mmol/L, this method did expose patients to a risk of unmonitored hyperkalaemia. The other involves use of a feedback system with a computer-algorithm driven protocol. This method was not developed into a full production model due to lack of cost-effectiveness. We were unable to find any trials assessing the efficacy and safety of continuous potassium infusions in the critical care population, so felt it was time this was rectified. Critically ill patients are often hypokalaemic due to insensible losses, inadequate supplementation prior to admission, and use of diuretics and betaagonists. At the same time they often have acute and/or chronic renal failure or may have a metabolic acidosis that will hamper normal potassium sequestration or excretion. Thus they are at risk of rapidly developing life-threatening hyperkalaemia if supplementation is not carefully titrated against serial monitoring. Continuous infusions administered with due vigilance should allow for correction of hypokalaemia in a safe and precise manner. Our department used to supplement potassium by intermittent infusion, but after internal discussion we have successfully implemented a continuous infusion protocol. We propose that continuous infusions administered by accredited nurses under physician direction can safely deliver potassium and correct abnormal levels. Study Design Allocation: Randomized, Control: Dose Comparison, Endpoint Classification: Safety/Efficacy Study, Intervention Model: Parallel Assignment, Masking: Open Label, Primary Purpose: Treatment Conditions Hypokalemia Intervention Sterile Potassium Chloride Concentrate, Sterile Potassium Chloride Concentrate Status Completed Source The Queen Elizabeth Hospital Results (where available) View Results Mechanisms of hypokalemia-induced ventricular arrhythmogenicity. Fundam Clin Pharmacol 2010,Oct,01;24(5):547-59; (PMID: 20584206) Publication Type: Journal Article Fundamental & clinical pharmacology Osadchii, Oleg E; Department of Biomedical Sciences, The Danish National Research Foundation Centre for Cardiac Arrhythmia, The Panum Institute, University of Copenhagen, Blegdamsvej 3, 2200, Copenhagen N, Denmark. article abstract Hypokalemia is a common biochemical finding in cardiac patients and may represen angiotensin system and high adrenergic tone. Hypokalemia is independent risk fact arrhythmic death. Animal studies demonstrate that hypokalemia-induced arrhythm and abnormal pacemaker activity. The prolongation of ventricular repolarization in often associated with increased propensity for early afterdepolarizations. Slowed co threshold. Abnormal pacemaker activity is attributed to increased slope of diastolic Ca(2+) overload secondary to inhibition of Na(+) -K(+) pump and stimulation of the is not uniform at distinct ventricular sites thereby contributing to amplified spatial r hypokalemic heart preparations, the prolongation ofaction potential may be associa for ventricular re-excitation over late phase of repolarization.Shortened refractorine facilitating re-entry. The interplay of triggering factors (early and delayed afterdepo electrophysiological substrate (unidirectional conduction block, reduced excitation for the mechanism of life-threatening tachyarrhythmias in hypokalemic patients. Mechanisms of hypokalemia-induced ventricular arrhythmogenicity Citation: Fundamental and Clinical Pharmacology, October 2010, vol./is. 24/5(547-559), 0767-3981;1472-8206 (October 2010) Author(s): Osadchii O.E. Abstract: Hypokalemia is a common biochemical finding in cardiac patients and may represent a side effect of diuretic therapy or result from endogenous activation of renin-angiotensin system and high adrenergic tone. Hypokalemia is independent risk factor contributing to reduced survival of cardiac patients and increased incidence of arrhythmic death. Animal studies demonstrate that hypokalemia-induced arrhythmogenicity is attributed to prolonged ventricular repolarization, slowed conduction, and abnormal pacemaker activity. The prolongation of ventricular repolarization in hypokalemic setting is caused by inhibition of outward potassium currents and often associated with increased propensity for early afterdepolarizations. Slowed conduction is attributed to membrane hyperpolarization and increased excitation threshold. Abnormal pacemaker activity is attributed to increased slope of diastolic depolarization in Purkinje fibers, as well as delayed afterdepolarizations caused by Ca 2+ overload secondary to inhibition of Na+-K+ pump and stimulation of the reverse mode of the Na+-Ca2+ exchange. Hypokalemia effect on repolarization is not uniform at distinct ventricular sites thereby contributing to amplified spatial repolarization gradients which promote unidirectional conduction block. In hypokalemic heart preparations, the prolongation of action potential may be associated with shortening of effective refractory period, thus increasing the propensity for ventricular re-excitation over late phase of repolarization. Shortened refractoriness and slowed conduction contribute to reduced excitation wavelength thereby facilitating re-entry. The interplay of triggering factors (early and delayed afterdepolarizations, oscillatory prepotentials in Purkinje fibers) and a favorable electrophysiological substrate (unidirectional conduction block, reduced excitation wavelength, increased critical interval for ventricular re-excitation) may account for the mechanism of life-threatening tachyarrhythmias in hypokalemic patients. 2010 Societe Francaise de Pharmacologie et de Therapeutique. Language: English Hypokalemia and arrhythmias Richard H. Helfant, M.D. Abstract The focus of this article is hypokalemia, its electrophysiologic properties, and clinical arrhythmias. The effects of potassium on the electrophysiologic properties of the heart have been extensively studied and clearly are arrhythmogenic. Hypokalemia increases resting membrane potential and increases both the duration of the action potential and the duration of the refractory period, the latter to a greater degree than the former. This combination is conducive to the genesis of reentrant arrhythmias. Hypokalemia also increases threshold potential as well as automaticity, thus providing the context for automatic arrhythmias as well. Lastly, hypokalemia decreases conductivity, which also predisposes to arrhythmias of the reentrant type. The electrocardiographic criteria for hypokalemia include the presence of U waves greater than 1 mm and U waves larger than the T wave in the same lead (with associated ST-segment depression). Other criteria have been a T:U ratio of 1 or less and a U wave greater than 0.5 mm in electrocardiographic lead II or greater than 1.0 mm in lead V3. The relationship between hypokalemia and clinical arrhythmias has long been recognized. In 1949, Bellet et al [1] reported extrasystoles with hypokalemic alkalosis that decreased with potassium administration. These observations were confirmed by several groups in the early 1950s. In 1953, Surawicz and Lepeschkin [2] described a series of patients with hypokalemia and frequent junctional and ventricular premature beats; in all cases the arrhythmias disappeared with administration of potassium. These clinical observations were strengthened by the 1962 findings of Gettes et al [3], who employed microelectrode techniques to show that perfusion of low potassium solutions resulted in ventricular ectopic beats, ventricular tachycardia, and ventricular fibrillation. In more recent years, several studies have evaluated the relationship between potassium levels and arrhythmias in patients with and without hypertension who were receiving diuretic therapy. These studies have demonstrated that there is an increased incidence of ventricular arrhythmias associated with the hypokalemia induced by diuretic therapy, an observation with obvious clinical implications. Diabetic ketoacidosis From Wikipedia, the free encyclopedia Diabetic ketoacidosis Classification and external resources Dehydration may be profound in diabetic ketoacidosis, and intravenous fluids are usually needed as part of its treatment ICD-10 E10.1, E11.1, E12.1,E13.1, E14.1 ICD-9 250.1 DiseasesDB 3709 MedlinePlus 000320 eMedicine med/548 MeSH D016883 Diabetic ketoacidosis (DKA) is a potentially life-threatening complication in patients withdiabetes mellitus. It happens predominantly in those with type 1 diabetes, but it can occur in those with type 2 diabetes under certain circumstances. DKA results from a shortage ofinsulin; in response the body switches to burning fatty acids and producing acidic ketone bodies that cause most of the symptoms and complications.[1] DKA may be the first symptom of previously undiagnosed diabetes, but it may also occur in known diabetics due to a variety of causes, such as intercurrent illness or poor compliance with insulin therapy. Vomiting, dehydration, deep gasping breathing, confusion and occasionally coma are typical symptoms. DKA is diagnosed with blood and urine tests; it is distinguished from other, rarer forms of ketoacidosis by the presence of high blood sugarlevels. Treatment involves intravenous fluids to correct dehydration, insulin to suppress the production of ketone bodies, treatment for any underlying causes such as infections, and close observation to prevent and identify complications.[1][2] DKA is a medical emergency, and without treatment it can lead to death. DKA was first described in 1886; until the introduction of insulin therapy in the 1920s it was almost universally fatal.[3] It now carries a mortality of less than 5% with adequate and timely treatment.[4] Contents [hide] 1 Signs and symptoms 2 Cause 3 Mechanism 4 Diagnosis o 4.1 Investigations o 4.2 Criteria 5 Prevention 6 Management o 6.1 Fluid replacement o 6.2 Insulin o 6.3 Potassium o 6.4 Bicarbonate o 6.5 Cerebral edema o 6.6 Resolution 7 Epidemiology 8 History 9 References [edit]Signs and symptoms The symptoms of an episode of diabetic ketoacidosis usually evolve over the period of about 24 hours. Predominant symptoms are nauseaand vomiting, pronounced thirst, excessive urine production and abdominal pain that may be severe. Those who measure their glucose levels themselves may notice hyperglycemia (high blood sugar levels). In severe DKA, breathing becomes labored and of a deep, gasping character (a state referred to as "Kussmaul respiration").[4] The abdomen may be tender to the point that an acute abdomen may be suspected, such as acute pancreatitis, appendicitis or gastrointestinal perforation.[4] Coffee ground vomiting (vomiting of altered blood) occurs in a minority of patients; this tends to originate from erosion of the esophagus.[3] In severe DKA, there may be confusion, lethargy, stupor or even coma (a marked decrease in the level of consciousness).[4][5] On physical examination there is usually clinical evidence of dehydration, such as a dry mouth and decreased skin turgor. If the dehydration is profound enough to cause a decrease in the circulating blood volume, tachycardia (a fast heart rate) and low blood pressuremay be observed. Often, a "ketotic" odor is present, which is often described as "fruity", often compared to the smell of pear drops whose scent is a ketone. If Kussmaul respiration is present, this is reflected in an increased respiratory rate.[4] Small children with DKA are relatively prone to cerebral edema (swelling of the brain tissue), which may cause headache, coma, loss of thepupillary light reflex, and progress to death. It occurs in 0.7–1.0% of children with DKA, and has been described in young adults, but is overall very rare in adults. [1][4][6] It carries a 20–50% mortality.[7] [edit]Cause DKA most frequently occurs in those who already have diabetes. It may also be the first presentation in someone who had not previously been known to be diabetic. There is often a particular underlying problem that has led to the DKA episode. This may be intercurrent illness (pneumonia, influenza, gastroenteritis, a urinary tract infection), pregnancy, inadequate insulin administration (e.g. defective insulin pen device), myocardial infarction (heart attack), stroke or the use of cocaine. Young patients with recurrent episodes of DKA may have an underlying eating disorder, or may be using insufficient insulin for fear that it will cause weight gain.[4] In 5% of cases, no cause for the DKA episode is found.[1] Diabetic ketoacidosis may occur in those previously known to have diabetes mellitus type 2 or in those who on further investigations turn out to have features of type 2 diabetes (e.g. obesity, strong family history); this is more common in African, African-American and Hispanic people. Their condition is then labeled "ketosis-prone type 2 diabetes".[1][8] [edit]Mechanism Diabetic ketoacidosis arises because of a lack of insulin in the body. The lack of insulin and corresponding elevation of glucagon leads to increased release of glucose by the liver (a process that is normally suppressed by insulin) from glycogen and through gluconeogenesis. High glucose levels spill over into the urine, taking water and solutes (such as sodium and potassium) along with it in a process known asosmotic diuresis. This leads to polyuria, dehydration, and compensatory thirst and polydipsia. The absence of insulin also leads to the release of free fatty acids from adipose tissue, which are converted, again in the liver, into ketone bodies (acetoacetate and β-hydroxybutyrate). β-Hydroxybutyrate can serve as an energy source in absence of insulinmediated glucose delivery, and is likely a protective mechanism in case of starvation. The ketone bodies, however, have a low pH and therefore turn the blood acidic (metabolic acidosis). The body initially buffers this with the bicarbonate buffering system, but this is quickly overwhelmed and other mechanisms to compensate for the acidosis, such as hyperventilation to lower the blood carbon dioxide levels (a form of compensatory respiratory alkalosis). This hyperventilation, in its extreme form, may be observed as Kussmaul respiration.[1][4] Ketones, too, participate in osmotic diuresis and lead to further electrolyte losses.[1] In various situations such as infection, insulin demands rise but are not matched by the failing pancreas. Blood sugars rise, dehydration ensues, and resistance to the normal effects of insulin increases further by way of a vicious circle.[1][3] As a result of the above mechanisms, the average adult DKA patient has a total body water shortage of about 6 liters (or 100 mL/kg), in addition to substantial shortages in sodium, potassium, chloride, phosphate, magnesium and calcium. Glucose levels usually exceed 13.8 mmol/L or 250 mg/dL[1] β-hydroxybutyrate, despite chemically not actually being a ketone, is the principal "ketone body" in diabetic ketoacidosis. DKA is common in type 1 diabetes as this form of diabetes is associated with an absolute lack of insulin production by the islets of Langerhans. In type 2 diabetes, insulin production is present but is insufficient to meet the body's requirements as a result of end-organ insulin resistance. Usually, these amounts of insulin are sufficient to suppress ketogenesis. If DKA occurs in type 2 diabetics, their condition is called "ketosis-prone type 2 diabetes".[8] The exact mechanism for this phenomenon is unclear, but it appears that very high levels of glucose suppress the release of insulin from the pancreas through "glucotoxicity", leading to levels that are insufficient to suppress ketogenesis.[1] Furthermore, insulin resistance may be so severe that ketogenesis cannot be suppressed.[8] Once the condition has been treated, insulin production resumes and often the patient may be able to resume diet or tablet treatment like other type 2 diabetics. Nevertheless, a small proportion of this population has detectable antibodies against islets of Langerhans, and could therefore be regarded as having a form of type 1 diabetes.[1] The clinical state of DKA is associated, in addition to the above, with the release of various counterregulatory hormones such as glucagonand adrenaline as well as cytokines, the latter of which leads to increased markers of inflammation, even in the absence of infection.[1][2] Cerebral edema, which is the most dangerous DKA complication, is probably the result of a number of factors. Some authorities maintain that it is the result from overvigorous fluid replacement, but the complication may develop before treatment has been commenced.[6][7] It is more likely in those with more severe DKA,[2] and in the first episode of DKA.[6] Likely factors in the development of cerebral edema are dehydration, acidosis and low carbon dioxide levels; in addition, the increased level of inflammation and coagulation may, together with these factors, lead to decreased blood flow to parts of the brain, which then swells up once fluid replacement has been commenced.[6] The swelling of brain tissue leads to raised intracranial pressure ultimately leading to death.[2][7] [edit]Diagnosis [edit]Investigations Diabetic ketoacidosis may be diagnosed when the combination of hyperglycemia (high blood sugars), ketones in the blood or on urinalysisand acidosis are demonstrated. Arterial blood gas measurement is usually performed to demonstrate the acidosis; this requires taking a blood sample from an artery. Subsequent measurements (to ensure treatment is effective), may be taken from a normal blood test taken from a vein, as there is little difference between the arterial and the venous pH.[1][5] In addition to the above, blood samples are usually taken to measure urea and creatinine (measures of kidney function, which may be impaired in DKA as a result of dehydration) and electrolytes. Furthermore, markers of infection (complete blood count, C-reactive protein) and acute pancreatitis (amylase and lipase) may be measured. Given the need to exclude infection, chest radiography and urinalysis are usually performed.[1] If cerebral edema is suspected because of confusion, recurrent vomiting or other symptoms, computed tomography may be performed to assess its severity and to exclude other causes such as stroke.[7] [edit]Criteria Diabetic ketoacidosis is distinguished from other diabetic emergencies by the presence of large amounts of ketones in blood and urine, and marked metabolic acidosis. Hyperosmolar hyperglycemic state (HHS, sometimes labeled "hyperosmolar non-ketotic state" or HONK) is much more common in type 2 diabetes and features increased plasma osmolarity (above 320 mosm/kg) due to profound dehydration and concentration of the blood; mild acidosis and ketonemia may occur in this state, but not to the extent observed in DKA. There is a degree of overlap between DKA and HHS, as in DKA the osmolarity may also be increased, but in most situations it is possible to classify a case into either DKA or HHS.[1] Ketoacidosis is not always the result of diabetes. It may also result from alcohol excess and from starvation; in both states the glucose level is normal or low. Metabolic acidosis may occur in diabetics for other reasons, such as poisoning with ethylene glycol or paraldehyde. Type 2 diabetics taking metformin may develop lactic acidosis as a rare side-effect of their medication.[1] A 2006 American Diabetes Association statement (for adults) categorizes DKA into one of three stages of severity:[1] Mild: blood pH mildly decreased to between 7.25 and 7.30 (normal 7.35–7.45); serum bicarbonate decreased to 15–18 mmol/l (normal above 20); the patient is alert Moderate: pH 7.00–7.25, bicarbonate 10–15, mild drowsiness may be present Severe: pH below 7.00, bicarbonate below 10, stupor or coma may occur A 2004 statement by the European Society for Paediatric Endocrinology and the Lawson Wilkins Pediatric Endocrine Society (for children) uses slightly different cutoffs, where mild DKA is defined by pH 7.20–7.30 (bicarbonate 10–15 mmol/l), moderate DKA by pH 7.1–7.2 (bicarbonate 5–10) and severe DKA by pH<7.1 (bicarbonate below 5).[2] [edit]Prevention Attacks of DKA can be prevented in known diabetics to an extent by adherence to "sick day rules"; these are clear-cut instructions to patients on how to treat themselves when unwell. Instructions include advice on how much extra insulin to take when sugar levels appear uncontrolled, an easily digestible diet rich in salt and carbohydrates, means to suppress fever and treat infection, and recommendations when to call for medical help (such as a certified diabetes educator).[1][5] [edit]Management The main aims in the treatment of diabetic ketoacidosis are replacing the lost fluids and electrolytes while suppressing the high blood sugars and ketone production with insulin. Admission to an intensive care unit or similar high-dependency area or ward for close observation may be necessary.[1][5] [edit]Fluid replacement The amount of fluid depends on the estimated degree of dehydration. If dehydration is so severe as to cause shock (severely decreasedblood pressure with insufficient blood supply to the body's organs), or a depressed level of consciousness, rapid infusion of saline (1 liter for adults, 10 ml/kg in repeated doses for children) is recommended to restore circulating volume.[1][9] Slower rehydration based on calculated water and sodium shortage may be possible if the dehydration is moderate, and again saline is the recommended fluid.[1][9][10] Very mild ketoacidosis with no associated vomiting and mild dehydration may be treated with oral rehydration and subcutaneous rather than intravenous insulin under observation for signs of deterioration. [9][10] A special but unusual consideration is cardiogenic shock, where the blood pressure is decreased not due to dehydration but due to inability of the heart to pump blood through the blood vessels. This situation requires ICU admission, monitoring of the central venous pressure(which requires the insertion of a central venous catheter in a large upper body vein), and the administration of medication that increases the heart pumping action and blood pressure.[1] [edit]Insulin Some guidelines recommend a bolus (initial large dose) of insulin of 0.1 unit of insulin per kilogram of body weight. This can be administered immediately after the potassium level is known to be higher than 3.3 mmol/l; if the level is any lower, administering insulin could lead to a dangerously low potassium level (see below).[1][5] Other guidelines recommend delaying the initiation of insulin until fluids have been administrered. [9] In general, insulin is given at 0.1 unit/kg per hour to reduce the blood sugars and suppress ketone production. Guidelines differ as to which dose to use when blood sugar levels start falling; some recommend reducing the dose of insulin once glucose falls below 16.6 mmol/l (300 mg/dl)[1] but other recommend infusing glucose in addition to saline to allow for ongoing infusion of higher doses of insulin.[9][5] [edit]Potassium Potassium levels can fluctuate severely during the treatment of DKA, because insulin decreases potassium levels in the blood by redistributing it into cells. Serum potassium levels are initially often mildly raised even though total body potassium is depleted—as potassium from the intracellular space would have been shifted to the extracellular space in an exchange for hydrogen ions that accumulate extracellularly in acidosis of DKA. A large part of the shifted extracellular potassium would have been lost in urine because of osmotic diuresis. Hypokalemia (low blood potassium concentration) often follows treatment. This increases the risk of dangerous irregularities in the heart rate. Therefore, continuous observation of the heart rate is recommended,[9] as well as repeated measurement of the potassium levels and addition of potassium to the intravenous fluids once levels fall below 5.3 mmol/l. If potassium levels fall below 3.3 mmol/l, insulin administration may need to be interrupted to allow correction of the hypokalemia.[1] [edit]Bicarbonate The administration of sodium bicarbonate solution to rapidly improve the acid levels in the blood is controversial. There is little evidence that it improves outcomes beyond standard therapy, and indeed some evidence that while it may improve the acidity of the blood, it may actually worsen acidity inside the body's cells and increase the risk of certain complications. Its use is therefore discouraged, [2][5][10]although some guidelines recommend it for extreme acidosis (pH<6.9), and smaller amounts for severe acidosis (pH 6.9–7.0).[1] [edit]Cerebral edema Cerebral edema, if associated with coma, often necessitates admission to intensive care, artificial ventilation, and close observation. The administration of fluids is slowed. The ideal treatment of cerebral edema in DKA is not established, but intravenous mannitol and hypertonic saline (3%) are used—as in some other forms of cerebral edema—in an attempt to reduce the swelling.[2] [edit]Resolution Resolution of DKA is defined as general improvement in the symptoms, such as the ability to tolerate oral nutrition and fluids, normalization of blood acidity (pH>7.3), and absence of ketones in blood (<1 mmol/l) or urine. Once this has been achieved, insulin may be switched to the usual subcutaneously administrered regimen, one hour after which the intravenous administration can be discontinued.[9][5] In patients with suspected ketosis-prone type 2 diabetes, determination of antibodies against glutamic acid decarboxylase and islet cellsmay aid in the decision whether to continue insulin administration long-term (if antibodies are detected), or whether to attempt treatment with oral medication as in type 2 diabetes.[1] [edit]Epidemiology Diabetic ketoacidosis occurs in 4.6–8.0 per 1000 type 1 diabetics annually. In the United States, 100,000 hospital admissions occur annually as a result of DKA, at an estimated cost of $1 billion or half the total cost of caring for type 1 diabetics. Since the 1980s there has been a documented increasing trend to hospital admissions. The risk is increased in those with an ongoing risk factor, such as an eating disorder, and those who cannot afford insulin.[1] About 30% of children with type 1 diabetes receive their diagnosis after an episode of DKA.[11] [edit]History The first full description of diabetic ketoacidosis is attributed to Julius Dreschfeld, a German pathologist working in Manchester, United Kingdom. In his description, which he gave in an 1886 lecture at the Royal College of Physicians in London, he drew on reports by Adolph Kussmaul as well as describing the main ketones, acetoacetate and β-hydroxybutyrate, and their chemical determination.[12] The condition remained almost universally fatal until the discovery of insulin in the 1920s; by the 1930s, mortality had fallen to 29%,[3] and by the 1950s it had become less than 10%.[13] The entity of cerebral edema due to DKA was described in 1936 by a team of doctors from Philadelphia.[7][14] Numerous research studies since the 1950s have focused on the ideal treatment for diabetic ketoacidosis. A significant proportion of these studies have been conducted at the University of Tennessee Health Science Center and Emory University School of Medicine.[13] Treatment options studied have included high- or low-dose intravenous, subcutaneous or intramuscular (e.g. the "Alberti regime") insulin, phosphate supplementation, need for a loading dose of insulin, and appropriateness of using bicarbonate therapy in moderate DKA.[13] Various questions remain unanswered, such as whether bicarbonate administration in severe DKA makes any real difference to the clinical course, and whether an insulin loading dose is needed in adults. [13] The entity of ketosis-prone type 2 diabetes was first fully described in 1987 after several preceding case reports. It was initially thought to be a form of maturity onset diabetes of the young,[15] and went through several other descriptive names (such as "idiopathic type 1 diabetes", "Flatbush diabetes", "atypical diabetes" and "type 1.5 diabetes") before the current terminology of "ketosis-prone type 2 diabetes" was adopted.[1][8] [edit]References 1. ^ a b c d e f g h i j k l m n o p q r s t u v w x y z aa ab ac Kitabchi AE, Umpierrez GE, Murphy MB, Kreisberg RA (December 2006)."Hyperglycemic crises in adult patients with diabetes: a consensus statement from the American Diabetes Association". Diabetes Care 29 (12): 2739–48.doi:10.2337/dc06-9916. PMID 17130218. 2. ^ a b c d e f g Dunger DB, Sperling MA, Acerini CL, et al. (February 2004). "European Society for Paediatric Endocrinology/Lawson Wilkins Pediatric Endocrine Society consensus statement on diabetic ketoacidosis in children and adolescents". Pediatrics113 (2): e133–40. doi:10.1542/peds.113.2.e133.PMID 14754983. 3. ^ a b c d Eledrisi MS, Alshanti MS, Shah MF, Brolosy B, Jaha N (May 2006). "Overview of the diagnosis and management of diabetic ketoacidosis". American Journal of Medical Science 331(5): 243– 51. doi:10.1097/00000441-200605000-00002.PMID 16702793. 4. ^ a b c d e f g h Powers AC (2005). "Diabetes mellitus". In Kasper DL, Braunwald E, Fauci AS, et al.. Harrison's Principles of Internal Medicine (16th ed.). New York, NY: McGraw-Hill. pp. 2152–2180.ISBN 0-071-39140-1. 5. ^ a b c d e f g h Joint British Diabetes Societies Inpatient Care Group (March 2010). "The Management of Diabetic Ketoacidosis in Adults" (PDF). NHS Diabetes. Retrieved 2010-06-06. 6. ^ a b c d Glaser N (June 2006). "New perspectives on the pathogenesis of cerebral edema complicating diabetic ketoacidosis in children". Pediatric Endocrinology Reviews 3 (4): 379–86. PMID 16816806. 7. ^ a b c d e Brown TB (March 2004). "Cerebral oedema in childhood diabetic ketoacidosis: is treatment a factor?". Emergency Medical Journal 21 (2): 141– 4. doi:10.1136/emj.2002.001578.PMID 14988335. PMC 1726262. 8. ^ a b c d Umpierrez GE, Smiley D, Kitabchi AE (March 2006)."Narrative review: ketosis-prone type 2 diabetes mellitus".Annals of Internal Medicine 144 (5): 350–7. PMID 16520476. 9. ^ a b c d e f g Edge J (May 2009). "BSPED Recommended DKA Guidelines 2009". British Society for Paediatric Endocrinology and Diabetes. Retrieved 2009-07-12. 10. ^ a b c National Institute for Health and Clinical Excellence. Clinical guideline 15: Diagnosis and management of type 1 diabetes in children, young people and adults . London, 2004. 11. ^ Silverstein J, Klingensmith G, Copeland K, et al. (January 2005)."Care of children and adolescents with type 1 diabetes: a statement of the American Diabetes Association". Diabetes Care 28 (1): 186– 212. doi:10.2337/diacare.28.1.186.PMID 15616254. 12. ^ Dreschfeld J (1886). "Diabetic coma; Bradshawe lecture".British Medical Journal 2: 358– 63. doi:10.1136/bmj.2.1338.358. 13. ^ a b c d Kitabchi AE, Umpierrez GE, Fisher JN, Murphy MB, Stentz FB (May 2008). "Thirty years of personal experience in hyperglycemic crises: diabetic ketoacidosis and hyperglycemic hyperosmolar state". Journal of Clinical Endocrinology and Metabolism 93 (5): 1541–52. doi:10.1210/jc.2007-2577.PMID 18270259. 14. ^ Dillon ES, Riggs HE, Dyer WW (1936). "Cerebral lesions in uncomplicated fatal diabetic acidosis". American Journal of the Medical Sciences 3: 360–365. doi:10.1097/00000441-193609000-00007. 15. ^ Winter WE, Maclaren NK, Riley WJ, Clarke DW, Kappy MS, Spillar RP (February 1987). "Maturity-onset diabetes of youth in black Americans". New England Journal of Medicine 316 (6): 285– 91. doi:10.1056/NEJM198702053160601. PMID 3543673.