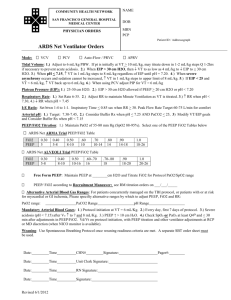
PEEP - Clinical Departments
advertisement

Rob Bartlett Keywords July 19, 2010 I. PEEP: PaO2, Lung Volumes, LV effect a. Positive end expiratory pressure – continuous pressure exerted throughout the respiratory cycle (CPAP) – 3 indications i. Prevent derecruitment, by returning the functional residual volume to the physiologic range. ii. Protect the lungs against injury by preventing phasic opening and closing of atelectatic units iii. Assist cardiac performance, during heart failure, by increasing mean intrathoracic pressure b. Lung Volumes i. FRC (functional residual capacity) – about 2.5 liters of volume left at the end of normal tidal breathing that serves as our O2 reservoir during apnea (capacity composed of two volumes) 1. Residual volume – about 1 liter 2. Expiratory reserve volume ii. FRC decreased under general anesthesia due to low tidal volume ventilation and reduced sigh breaths to prevent atelectasis. 1. PEEP maintains small airway tone and prevents pt from reaching closing capacity thereby Increasing FRC 2. Decreased atelectasis improves the Low V/Q mismatch (shunt with venous admixture) and raises PO2 c. Cardiac Effects i. Increased intrathoracic pressure may decrease venous return and right heart preload ii. Left Ventricle - Afterload is decreased by acting as external compression of the LV making it easier to achieve a given systemic pressure. d. Complications of PEEP i. Alveolar overdistention – Heterogenicity of alveoli means Nondependent zone/healthy alveoli tend not to collapse at end expiration and added peep may over distend alveoli collapsing capillaries creating increased Dead space and large V/Q mismatch (wasted ventilation) ii. Cardiac – 1. Decrease Venous Return - PEEP increases intrathoracic pressure and may decrease venous return to right heart leading to decreased cardiac output a. Most pronounced with extreme PEEP and hypovolemia 2. Elevated Pulmonary vascular resistance – PEEP increases pressure on intrapulmonary vasculature and increases PVR leading to increased RV afterload. a. Most pronounced with acute increases PVR (ie new PE) or extreme PEEP b. If RV failure and over distention may reduce LV compliance secondary to interventricular interdependance (shared septum) iii. Neuro - May reduce CPP by two mechanisms 1. Reduction of cardiac output 2. Increased intrathoracic pressure can be transmitted to SVC and decrease venous drainage from jugular veins. References: http://www.ccmtutorials.com/rs/peep/page10.htm, accessed on 9/17/2010. Marino, Paul. The ICU Book. 3rd edition 2007. pg481-486.