File - Respiratory Therapy Files
advertisement
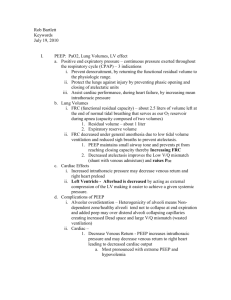
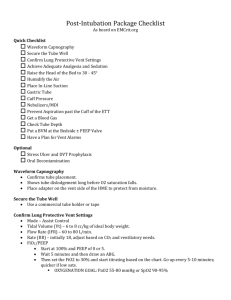
Ventilators: -There are 3 modes: AC/VC, SIMV, and Spontaneous/CPAP -AC/VC: is when the patient is not spontaneously breathing and the vent is breathing for them -SIMV: is when the vent is breathing for the patient but the patient can take spontaneous breaths in between the mechanical breaths -CPAP: the patient is breathing spontaneously, but the vent may be giving some type of support to help the patients tidal volumes, or overcoming RAW Breath types: -Volume Control: Set a patients tidal volume (Normal is 8-12 mL/kg unless have COPD or restrictive disease then we use protective measures and use 5-7mL/kg), we set patients flow (4060), we set a rate (8-12), we set a PEEP (0-5 starting), we set Fi02 (40-60) -Pressure Control: We set a pressure limit (15-25 cmH20), rise time, Fi02, PEEP, rate, and inspiratory time -PRVC: It's a mix of both pressure control and volume control. -You set everything in this breath type except flow. -you set a target tidal volume, and a pressure alarm. The vent will give a pressure support to support the patients tidal volume. If the pressure comes within 5 of the limit, the vent will begin to dump the volumes to prevent injury -Volume Support: occurs in spontaneous modes only. Gives pressure support to support the patients tidal volumes. It is essentially the same as PRVC except spontaneous breaths. -APRV: use for ARDS. you set a high PEEP, low PEEP, high time, and low time. The patient will be breathing spontaneously. The high time will be longer than the low time as well, and when the patient goes from the high peep level to the low is when they blow off their C02. To wean the patient you are dropping the high pressure, extending the high time, and subsequently adding pressure support at the same time. Once the patient reaches a time when the pressure support and high peep are both 15, they can be switched over to just pressure support. High peep is initially set at 20-25, high time initially set at 3-6, low peep 0-5, and low time 0.2-0.8 -Proportional Assist Ventilation: gives support in proportion to patients effort. -ATC: Vent gives enough flow just to overcome RAW of ET tube -VAPS: set min Vt, rr, flow, peep, Fi02. If min Vt not met, vent will keep delivering flow until Vt met. PS is minimum pressure pt receives Graphs/waveforms: -Flow-Time: auto-peep -Pressure-time: patient triggers, rise-time, flow starvation -Pressure-Volume: increased RAW, overdistention, leaks -Flow-Volume: pre/post bronchodilator From homework #1 -Lung compliance= the lungs' ability to stretch and accept volume -Elasticity= the ability to return to its normal state after being stretched -frictional resistance= made up of tissue viscosity and airway resistance -static compliance is the the compliance of the lungs without air flow. It's calculation is Vt/plat P - PEEP -Dynamic compliance is the compliance of the lungs with air flow. It's calculation is Vt/PIPPEEP From homework #2 -To wean a patient from a vent, the underlying issue must be resolved -To wean a patient from a vent, their MIP must be at least -20 cmH20 (Normal is -80 to -100) -to wean a patient from a vent, their MEP must be at least 50 because it shows the patients ability to cough and clear secretions (Normal is 100 - 150) -to wean a patient from a vent, their vital capacity must be at least 10 - 15 mL/kg (Normal vital capacity is 3-5 liters) -there is no concrete evidence that shows weaning techniques that decrease a patients time on a ventilator From homework #3 -APRV was described up above. But research has not shown that APRV decreases a patients mortality in ARDS. However, research is pointing to the idea if it is caught early enough, it may decrease mortality From Homework#4 -HFV is the use of an oscillator. What is scary about the oscillator is that the patient is not ventilating. The lungs are just pressurized and gas is pushed in and sucked out by a drum. You can set a patients MAP (5 above what MAP was on the ventilator). We set amplitude which is the height of the vibrations a patient gets. Increasing the amplitude will blow off more C02 due to higher pressure gradients, and we set a patients Hertz (frequency). Decreasing hertz also blows off C02 because now the patient has the greatest amount of pressure gradients. Hemodynamics: study of blood flow -CVP: measures pressures of Right heart (Right Atrium, Right Ventricle, Vena Cava). Normal =2-6mmHg, or 4-12cmH20 -PA cath: measures CVP, PAP, PCWP, and CO -Right Atrium: 0-6mmHg -RV: 20-30/0-5 -PA: 20-30/6-15 -wedge: 4-12 Clinical Hemodynamics: -Right Heart fail: -CVP: increased -PAP: N or decreased -PCWP: N or decreased -Lung disorder (PE, HTN) -CVP: increased -PAP: increased -PCWP: N or decreased -Left heart fail -CVP: N or increased (Late sign) -PAP: increased -PCWP: increased CO: decreased -Hypovolemia -all hemodynamic pressures decreased Important hemodynamic values: -SV: 60-130 mL per beat - pulse pressure: 40mmHg (difference between systolic and diastolic pressures -Ejection fraction: 65-75% -SVR: <20 mmHg -PVR <2.5 mmHg