Chloral hydrate adverse reaction in newborns Seyedeh Fatemeh
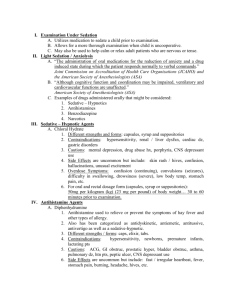
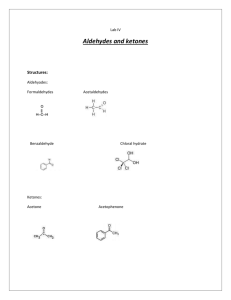
advertisement
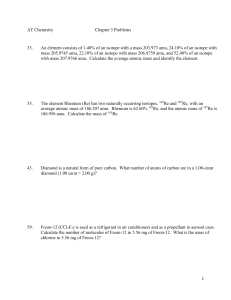
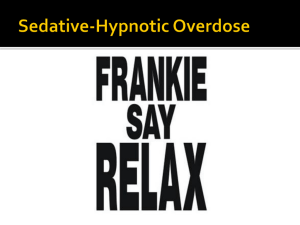
Chloral hydrate adverse reaction in newborns Seyedeh Fatemeh khatami Neonatologist Associate professor of Mashhad University of Medical Sciences Background: Chloral hydrate (CH) is a sedative-hypnotic (general central nervous system depressant) agent, and it has been widely used for sedation in the pediatric population. There are some adverse effects related to central nervous, dermatologic, gastrointestinal, genitourinary, and hematologic systems that have been recorded, Herein we report a newborn infant who developed respiratory arrest due to ingestion a dose of CH, to draw attention to the importance of adverse reaction especially when coadministered with barbiturates in newborn infants. Introduction: Chloral hydrate belongs to one of the oldest classes of pharmaceutical hypnotics, the chloral derivatives. It was introduced in 1832 and is still widely used to sedate children before diagnostic procedures. The unstable chloral hydrate rapidly converts by reduction to trichloroethanol (TCE), its major active metabolite with a half-life from 6 to 30 h. In the literature, nausea, vomiting, gastric irritation, nervousness, unusual excitement, respiratory depression, and mild or severe hypoxia have been reported during oral sedation consisting of chloral hydrate with or without other sedative -hypnotic drugs. Because of the current case, we would like to emphasize that CH may cause respiratory arrest in newborn infants; and, we suggest that all infants sedated with CH should be carefully monitored for respiratory arrest. Case report: A 8-day-old boy , birth weight 4020 gr, presented with a convulsion. He was the product of a 40-week term of gestation and labor. After the delivery, he had been hospitalized in another hospital with the diagnosis of perinatal asphyxia and given Phenobarbital. He was admitted to our hospital. The patient was hospitalized in order to investigate the etiology of the seizures and for management. The physical examination was normal. A magnetic resonance imaging (MRI) of the brain and electroencephalogram (EEG) were scheduled. In our clinic we routinely use oral CH (30 mg/kg/dose) for sedation before doing EEG, and this was ordered. Three hours after giving the CH hypotonicity, hyporeflexy, poor feeding, and hypotension were noted. Later, respiratory depression and hypoxia developed. Oral feeding was discontinued and he was monitored. Intravenous fluid and nasal oxygen were given. Serum glucose, calcium, electrolytes, renal and liver function tests were measured and all were found to be normal. A chest X-ray study was also normal. Ten hours after ingestion of CH he showed respiratory insufficiency in need of intubation and ventilation. While the brain MRI was found to be normal, the EEG was abnormal. During the hospitalization, serum phenobarbital level was normal (30). He improved and extubated after 3 days and then he was discharged. At the two weeks of follow-up he was symptom free. We could not determine the serum concentration of the main metabolite (i.e. trichloroethanol). Discussion: Chloral hydrate is frequently used in the pediatric population for sedation prior to procedures or radiologic testing, with apparent safety and efficacy at doses ranging from 25 to 50 mg/kg/dose. Although most authorities recommend dosages of 25–50mg/kg, doses up to 80 to 100 mg/kg have been given to children less than 5 years old with good effect and without toxicity. Chloral hydrate is rapidly absorbed following oral or rectal administration and extensively metabolized within minutes in the liver by alcohol dehydrogenase and by erythrocytes to its major active metabolite. trichloroethanol (TCE). Children metabolize chloral hydrate more slowly. The parent compound can be detected for several hours in infants up to 2 years of age and for 28 to 40 h in preterm infants. The average half-life of TCE in adults is 8 h, ranging from 4 to 12 h . In paediatric patients, TCE may be detected for up to 48 h . Peak concentration of TCE declines with increasing age with the highest peak concentrations in preterm infants .Trichloroethanol is 70–80% bound to plasma proteins and is widely distributed to all body issues including CFS, breast mild and placenta . Chloral hydrate intoxication may cause ventilatory failure, hypotension and hypothermia. Miosis, vomiting, areflexia and muscle flaccidity may also occur, as detected in our patient. Although chloral hydrate levels can assist in documenting the ingestion, they correlate poorly with clinical findings. TCE levels may be a more reliable indicator of toxicity. Management of chloral hydrate intoxication consists of considering gastric decontamination and general supportive and symptomatic therapy including maintenance of an adequate airway, assisted ventilation, maintaining body temperature and treating the often therapy resistant arrhythmias with IV beta blockers. Hemodialysis reportedly enhances the elimination of trichloroethanol; peritoneal dialysis may also be beneficial. It may be considered in patients with prolonged coma and refractory dysrrhythmias or hypotension. Although we could not determined the serum concentration of the main metabolite (i.e. trichloroethanol) but the clinical course suggested the side effects of this coadministration. Conclosion:Chloral hydrate intoxification is a potentially serious condition, in newborns when coadministered with phenobarbital, often requiring intensive care management. Everybody who works with newborns in a health care setting should be very careful with sedation in order to avoid intoxications. Key words: newborn, chloral hydrate, side effects, toxicity