outline5448
advertisement

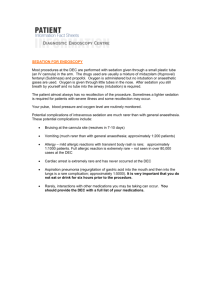
I. Examination Under Sedation A. Utilizes medication to sedate a child prior to examination. B. Allows for a more thorough examination when child is uncooperative. C. May also be used to help calm or relax adult patients who are nervous or tense. II. Light Sedation / Anxiolysis A. “The administration of oral medications for the reduction of anxiety and a drug induced state during which the patient responds normally to verbal commands.” Joint Commission on Accreditation of Health Care Organizations (JCAHO) and the American Society of Anesthesiologists (ASA) B. “Although cognitive function and coordination may be impaired, ventilatory and cardiovascular functions are unaffected.” American Society of Anesthesiologists (ASA) C. Examples of drugs administered orally that might be considered: 1. Sedative – Hypnotics 2. Antihistamines 3. Benzodiazepine 4. Narcotics III. Sedative – Hypnotic Agents A. Chloral Hydrate 1. Different strengths and forms: capsules, syrup and suppositories 2. Contraindications: hypersensitivity, renal / liver dysfxn, cardiac dz, gastric disorders 3. Cautions: mental depression, drug abuse hx, porphyria, CNS depressant use 4. Side Effects are uncommon but include: skin rash / hives, confusion, hallucinations, unusual excitement 5. Overdose Symptoms: confusion (continuing), convulsions (seizures), difficulty in swallowing, drowsiness (severe), low body temp, stomach pain, etc. 6. For oral and rectal dosage form (capsules, syrup or suppositories): 50mg per kilogram (kg) (23 mg per pound) of body weight… 30 to 60 minutes prior to examination. IV. Antihistamine Agents A. Diphenhydramine 1. Antihistamine used to relieve or prevent the symptoms of hay fever and other types of allergy. 2. Also has been categorized as antidyskinetic, antiemetic, antitussive, antivertigo as well as a sedative-hypnotic. 3. Different strengths / forms: caps, elixir, tabs. 4. Contraindications: hypersensitivity, newborns, premature infants, lactating pts 5. Cautions: ACG, GI obstruc, prostatic hyper, bladder obstruc, asthma, pulmonary dz, htn pts, peptic ulcer, CNS depressant use 6. Side Effects are uncommon but include: fast / irregular heartbeat, fever, stomach pain, burning, headache, hives, etc. V. VI. VII. VIII. 7. Overdose Symptoms: Clumsiness or unsteadiness, convulsions (seizures), drowsiness (severe), dryness of mouth, nose, or throat (severe), etc. 8. For oral dosage form (capsules, tablets, or liquid): 1 to 1.5 mg per kilogram (kg) (0.45 to 0.7 mg per pound) of body weight… 60 to 120 minutes prior to examination. Emergency Medicine: Stat Kit or Crash Cart A. Oxygen System 1. Your Stat Kit or Crash Cart must have oxygen delivery equipment. 2. Know basic life support and how to intervene in the event of complications Patient Selection A. Infants and young children 1. ASA Class I or II qualify for sedation 2. Diagnostic / therapeutic procedure are required 3. Previous attempts (unsedated) have been unsuccessful. B. ASA Physical Status Classification 1. Class I: Normal, healthy patient 2. Class II: Patient with mild systemic dz 3. Class III: Patient w/ severe systemic dz 4. Class IV: Pt w/ syst dz w/ threat to life 5. Class V: Pt who is needs sx to survive 6. Class VI: Brain-dead pt w/ donor organs Pre-sedation Counseling A. Informed consent by parent / legal guardian B. Parent / legal guardian must be present before, during and after sedation C. Patient should not drink fluids or eat solid foods as directed (Fasting Protocol) 1. Age of Child a) < 6 months b) 6 – 36 months c) 36 months 2. Solids and Nonclear Liquids a) 4 – 6 hours b) 6 hours c) 6 – 8 hours 3. Clear Liquids a) 2 hours b) 2 – 3 hours c) 2 – 3 hours Presedation Preparation A. Review of systemic condition w/ PCP B. Choose appropriate sedative agent C. Weigh patient and calculate dosage 1. Weight: 39 pounds 2. 2.2 pounds = 1 kilogram 3. 39 / 2.2 = 17.73 kilograms 4. 50 mg / kg std dosage 5. 50 mg x 17.73 kg = 886.50mg 6. Syrup (500 mg / 5ml) 7. 886.50 mg x 5 ml = 500mg (?ml) 8. 8.87 ml Syrup given D. Rx / obtain sedative agent E. Schedule EUS appropriately IX. Requirements During Sedation A. Obtain baseline vital signs 1. Blood Pressure 2. Pulse 3. Respiration B. Administer medication 1. ONLY in office by physician or technician 2. Document time 3. Using a 5cc syringe works great 4. Squirt medication to back of mouth C. Patient Monitoring 1. Continuous throughout the procedure by parent / guardian 2. Every 15 minute by physician / technician 3. Retake vital signs every 30 minutes 4. Also monitor alertness X. Patient Recovery A. Examination or procedure is complete 1. Check patients level of consciousness 2. Vital signs are recorded B. Patient Discharge 1. Patient is discharged to the care of parent / guardian 2. Vital signs are stable 3. Patient is responsive to stimuli 4. Written post – discharge instructions are reviewed w/ parent / guardian 5. Include after effects of sedation 6. Follow – up appointment if necessary 7. Emergency Service 24 / 7 protocol XI. Video Case Presentation A. Wild Child 1. 3 YO AA M presents for consultation from pediatrician ref possible eye turn OS since birth 2. Hx – Normal birth weight, 1 mo premature, borderline asthma, no previous eye exam 3. 5ml given @ 2:00 pm; vital signs normal 4. Another 3.75 ml given @ 2:30 pm; vital signs normal B. Examination Results 1. UCVA 20 / 30 OD & OS on Allen Chart; No significant RE w/ cycloplegic refraction 2. EOMS: Full w/ intermittent exotropia @ distance; eyes are straight @ near fixation; no signs of Duane’s Syndrome 3. No proptosis; pupils, SLE & DFE normal XII. Practice Management Considerations A. Scheduling Appointments B. Coding and Billing C. Medico-Legal Issues XIII. Reading References 1. Noske W, Papadopous G. Chloral Hydrate for pediatric ophthalmologic examinations. May; 2(3); 189-93. 2. Lipshitz M, Marino BL, Sanders ST. Chloral hydrate side affects in young children: causes and management. Heart Lung. 1993 Sep-Oct; 22(5): 40814. 3. Binder LS, Leake LA. Chloral hydrate for emergent pediatric procedural sedation: a new look at an old drug. Am J Emerg Med. 1991 Nov; 9(^): 530-4. 4. Rumm PD, Takao RT, Fox DJ, Atkinson SW. Efficacy of sedation of children with chloral hydrate. South Med J. 1990 Sep; 83(9): 1040-3. 5. Fox BE, O’Brien CO, Kangas KJ, Murphree AL, Wright KW. Use of high dose chloral hydrate for ophthalmic exams in children: a retrospective review of 302 cases. J Pediatric Ophthalmol Strabismus. 1990 Sep-Oct; 27(5): 242.4. 6. ACR Practice Guideline For Pediatric Sedation/Analgesia. American College of Radiology 2002; 301-7.